Mouth rot in children and toddlers
definition
Oral rot in children is a very painful inflammatory disease of the oral mucosa. The mouth rot (also Herpetic gingivostomatitis usually occurs between the ages of 10 months and three years and is caused by the child's first contact with the Herpes simplex virus type 1 triggered.
Usually during the illness there is a fever and - due to the painful inflammation in the mouth - the refusal to eat. Many small canker sores form, especially on the gums and the palate and yellowish coated wounds, also the inside of the lips and the tongue can be affected.
General information can be found here: The mouth rot

Causes of Oral Rot
The cause of oral rot in children is the first contact with the herpes simplex virus type 1, which is transmitted from person to person. Most adults carry the herpes virus, but a strengthened immune system does not always cause the disease to break out, but they can still transmit the herpes virus.
It is different with children: They come into contact with the herpes virus for the first time and their immune system is still building up, so it quickly comes to an infection and the spread of the oral rot in the oral cavity. The disease is highly contagious and is transmitted through saliva.
The herpes virus is very often transmitted from parents to children. Everyday situations are often the trigger, it is enough to lick the pacifier, use the cutlery together or a simple kiss, to transmit the herpes virus.
Especially in the case of an acute cold sore in one of the parents, any mouth contact with the child should be avoided. Sometimes child-to-child transmission occurs through toys that the children put in their mouths.
Read also: Herpes in the baby
That is the way of infection
Herpes simplex viruses are transmitted via contact infection, including smear and droplet infections. The virus is mainly transmitted through saliva.
Children suffering from oral rot excrete the viruses through their saliva to the environment; the viruses survive and can be ingested by other people. Depending on the state of the immune system, there is an initial infection or a secondary infection; the latter manifests itself in a cold sore, whereby the initial infection usually develops into a mouth rot. During the period of the illness, one should pay more attention to adequate hygiene.
Find out more about the topic here: Contagion with mouth rot
Such is the course of oral rot
Mouth rot in children often begins with a fever, which can sometimes be quite high. The fever usually lasts up to five days.
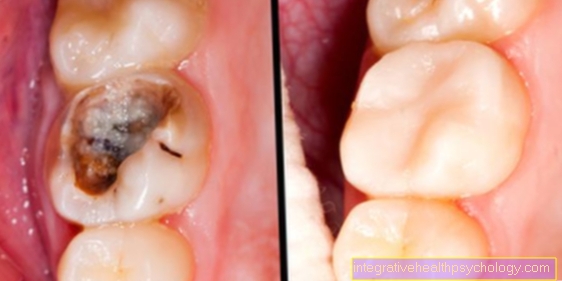
After the first two to three days, blisters and canker sores are usually formed on the oral mucosa. Mainly localized on the roof of the mouth and gums, but the insides of the lips and tongue can also to be affected. The gums can also swell.
In the first few days there is usually no pain, only when the oral rot has spread further and small open wounds have formed in addition to the increased vesicles. There is then burning, persistent pain, so that food intake is only possible to a very limited extent.
In addition, the gums can bleed and the gums turn darker red. Since the tongue is also inflamed, the tongue papillae may appear whitish. The inflammation can also cause the tongue to swell, which can lead to additional swallowing difficulties.
The cervical lymph nodes can also swell during this time. After about a week the blisters will dry out and the wounds will heal. Only then does the pain subside and the acute risk of infection no longer exists.
Learn more about this at:
- Course of the mouth rot
- Canker sores - Different options for treatment
This is how dangerous mouth rot can be
Due to the fever and the severe pain in the mouth, the children feel very ailing and often refuse to eat, especially regular and sufficient drinking is very important. It can often lead to dehydration (dry out) of the child and thereby lead to dangerous conditions.
If the toddler does not want to eat or drink, see the pediatrician immediately. Babies and toddlers are particularly at risk. They can develop severe oral rot and even inflammation of the brain. The disease is then called herpes simplex encephalitis.
If there is an additional infection of the skin near the eye, the worst case scenario is an infection of the cornea in the eye.
You may also be interested in this topic: Dehydration in children
diagnosis
Mouth rot is a common and relatively easily recognizable disease for medical professionals. The connection between the initial fever and the course of the disease, in which blistering and burning pain occur, is a typical characteristic indication for oral rot disease.
Nevertheless, a pure visual diagnosis is not one hundred percent certain and an additional laboratory test is recommended, especially in the case of severe oral rot. This can be done with a saliva test or a mouth swab. There are numerous other diseases of the mouth, especially oral thrush which can show similar symptoms.
This doctor treats the oral rot
Oral rot in the child should first be examined by a pediatrician. The pediatrician can make a diagnosis relatively quickly. Medicines are only needed in exceptional cases and used differently depending on the severity of the disease. First, the fever is controlled by antipyretic drugs (e.g. Paracetamol juice) treated. The pain can be relieved by applying gel or tincture.
A dentist can also make the diagnosis and, if necessary, prescribe the appropriate medication. Often homeopathic medication and home remedies can also help, but a visit to the doctor for a diagnosis should always be made.
These symptoms can help you identify mouth rot
Typical symptoms of oral rot are an initial high fever, which can last up to five days. Externally palpable and possibly visible swollen lymph nodes on the neck and swollen gums in the mouth. The gums are colored a darker red and bleeding gums may occur. In addition, the entire oral mucosa can be swollen.
On the oral mucosa, especially on the roof of the mouth and gums, one can discover fluid-filled vesicles and aphthae, from which small open wounds often emanate. Especially when eating there is increased pain and therefore often a refusal to eat. In addition, there are sore throats, difficulty swallowing and increased salivation. Overall, the children feel battered and weak and often have a sour halitosis.
Symptoms on the tongue
The tongue papillae can become inflamed with oral rot and appear as whitish spots. The inflammation of the tongue can also be very painful and lead to difficulty swallowing. Swelling of the tongue is also possible, which makes swallowing more difficult and should be carefully observed. The pain in the tongue often makes speaking difficult.
Treatment and therapy
Therapy is usually symptomatic, which means that you fight the symptoms and not the cause. It is important to visit the pediatrician in order to make an exact diagnosis and accordingly choose the right therapy. Above all, make sure you drink enough fluids to avoid dehydration of the body.
The fever-lowering drug paracetamol is often used to lower fever used. In children, often in the form of a juice or a suppository.
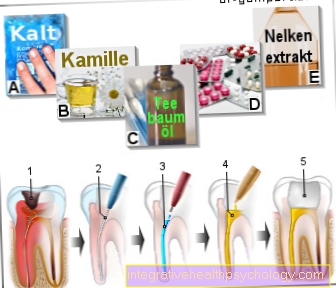
In addition, an anesthetic gel (e.g. Teething Gel) can be applied to the sore spots. It is recommended to drink cold chamomile tea, which is said to have a healing effect and at the same time relieve pain by cooling it.
The children should rest and not go to kindergarten until the mouth rot has healed completely. There are also other homeopathic remedies such as clove oil, which is said to have a pain-relieving effect.
Soft, low-salt and cool dishes make the food more bearable and a portion of ice is said to relieve pain and counteract inflammation by cooling.
You might also be interested in: Fever in the toddler
When does my child need antibiotics?
Since mouth rot is a viral disease caused by the herpes simplex virus, antibiotics are not used for therapy. Antibiotics only work against bacterial infections.
One option would be to use antivirals, such as acyclovir. However, these are only used in very serious cases and use in children is only indicated in exceptional cases.
Home remedies for mouth rot
A tried and tested home remedy for mouth rot is chamomile tea. This should be allowed to cool down well before drinking and, ideally, also cool in the refrigerator. It has a calming effect and because of the cooling it also has an analgesic effect. Since adequate hydration is also very important, a straw can make drinking easier.
Soft, cool foods and even ice cream provide pain relief. Hot, spicy or sour foods are unsuitable, and salty foods should also be avoided. In addition, fruit juice can trigger additional burning due to the fruit acid.
Cold compresses such as calf compresses help reduce the fever.
Learn more about the topic at: Home remedies for mouth rot
homeopathy
As homeopathic alternatives for treating oral rot in children, there are clove oil, colloidal silver or a myrrh tincture.
For treatment, soak the clove oil or myrrh tincture with the cotton swab and dab the blisters with it. The colloidal silver is used undiluted as a mouthwash, it should be kept in the mouth as long as possible and then spit out. A concentration of 10 ppm or 25 ppm (parts per million) is completely sufficient in this case. The myrrh tincture, on the other hand, has a bitter taste and can also sting the wounds. Although it is said to have good healing properties, children do not like to accept it due to its taste and the additional burning sensation.
Oral rot is so contagious
Mouth rot in children is a smear and droplet infection and is highly contagious. It is transmitted through saliva.
Especially in kindergarten, children can quickly become infected with toys that are often put in their mouths. The first contact with the herpes simplex virus type 1 leads to the outbreak of oral rot in children.
When can my child go back to kindergarten?
Oral rot is highly contagious and the infection phase is only over once the blisters have healed and dried out completely. Only then can the child have contact with other children again. Therefore, the complete healing should be awaited before visiting the kindergarten. In addition, the affected children feel very weak and bruised from the fever and pain in the mouth, so that a visit to kindergarten is not possible.
incubation period
The incubation period is the period between contact with the herpes virus and the actual onset of the disease. It usually lasts for 1 to 26 days for mouth rot and varies from child to child.
The relatively long period of time makes it difficult to find out what exactly caused the infection, but it is usually found in the immediate vicinity of the child. The incubation time depends on the physical condition and the strength of the immune system of the respective child. Especially in very young children, the immune system is still developing and infection occurs more quickly.
At first the illness begins with a high fever in some cases and when the first blisters appear on the oral mucosa, the typical pain and side effects of oral rot begin.
Duration
Mouth rot in children is usually accompanied by fever, which lasts up to five days, after the first 2-3 days the typical vesicles usually form on the oral mucosa. The acute phase of oral rot lasts approximately depending on the severity and course of the disease one to two weeks on, then the blisters and wounds dry out and slowly heal, this can take up to three weeks.
After healing, the acute risk of infection is overcome, but the herpes viruses remain in the body and can later trigger an infection again, even in adulthood. This secondary infection usually occurs with a weakened immune system or stress and manifests itself as cold sores, the so-called cold sore.
In babies, the disease can last longer and be more severe. In the acute state, oral rot in babies usually lasts for about two weeks until there is an improvement and the entire course of the disease can last up to six weeks in the baby. Babies in particular should be checked by a pediatrician at the first signs; there is often a refusal to eat and this can lead to dangerous dehydration (dry out) come.
Read also:
- Mouth rot in the baby
- Duration of mouth rot
Recommendations from our editorial team
- Oral rot in the adult
- How long will it take for apths to go away?
- Canker sores on the tongue
- Herpes in the mouth
- Cold Sores - How To Treat It Right













.jpg)