Nerve root
anatomy
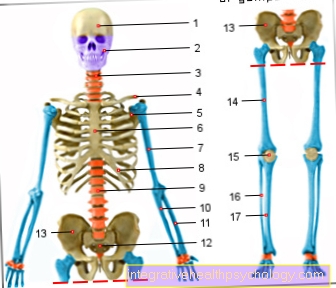
Most people's spine is made up of 24 freely moving vertebrae, which in turn are movably connected to one another by a total of 23 intervertebral discs.
The lower lying vertebrae of the coccyx and sacrum have grown together bony. However, deviations can occur from person to person.

The vertebrae of the different spinal column sections differ in their external shape and size, but the general structure of a vertebra remains similar.
So every vertebra is made up of a round one Vertebral bodies and one at the back Vertebral arch together.
All vertebral arches together form the Vertebral or spinal canalin which the Spinal cord runs.
This is done by the Cerebrospinal fluid, the Liquor, washed around. In addition, it is supported by the connective tissue Spinal membranes surrounded which in the Meninges skip and also as Meninges are designated.
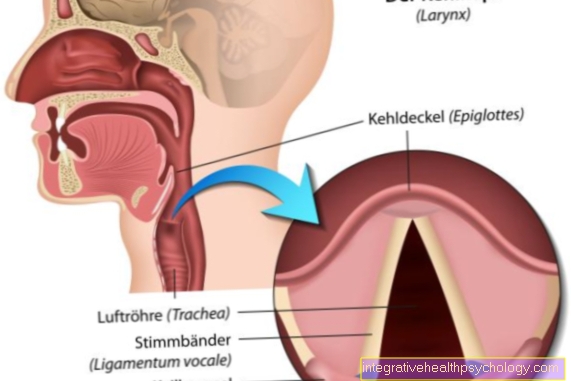
Viewed from the side, there is always a small, round space between two adjacent vertebral arches, the Intervertebral hole (Inervertebral foramen). The Spinal nerves which originated from the spinal cord on each floor.
These holes exist not only between the freely moving vertebrae, but also in the lower rigid sections of the spine.
In total there are mostly 31 of these intervertebral holes and thus also 31 spinal nerves. Here, too, there can be deviations from person to person.
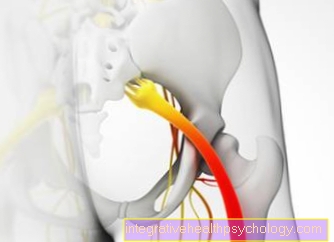
The points at which the spinal nerves arise are called Nerve roots designated. In each segment of the spine, there are two of these on both the right and left sides of the spinal cord.
These unite after a short process into one Spinal nerves each side, which then soon emerges through the intervertebral hole.
Interestingly, however, the adult spine is longer than the spinal cord. In adults, this only extends to about second lumbar vertebra.
The reason for this is the greater length growth of the spine compared to the spinal cord, which still fills the entire spinal canal up to the 3rd embryonic month.
The spinal nerves then have to cover an increasingly longer path downwards until they pass through the Intervertebral hole can escape. In their entirety, these spinal cord nerves, which run freely through the spinal canal, form the so-called Ponytail (Cauda equina).
function
As already described arise from this Spinal cord on each side and level two Nerve tractswhich only becomes a Spinal nerves unite. This rear and front Nerve roots carry different qualities of nerve fibers.
While the anterior nerve roots motor, impulses coming from the brain to the Muscles send, conduct the posterior nerve roots sensitive Impulses, for example information about ours Touch and temperature sensation in the spinal cord.
Here they are transferred to a second nerve cell and passed on to the brain. The cell nuclei of the sensitive nerve fibers lie exactly in the intervertebral hole and form a rounded expulsion of the nerve, the so-called Spinal ganglion.
In order to make it easier to name the various nerve fibers within a single nerve, they are differentiated according to their direction. Regardless of where exactly they run in the body and what quality of information they carry, nerve fibers running to the brain are generally called afferent and nerve fibers leading away from the brain as efferent designated.
The nerve roots thus fulfill the function of conveying information from the rest of the body to the brain and from the brain to the body.
The peripheral body is systematically different Spinal nerves allocated.
This is very clear in the case of the nervous supply to the skin. If you imagine the person sitting upright with arms and legs stretched out straight forward and then draw lines between the supply areas of the individual spinal nerves, it becomes clear that these supply areas largely form precisely drawn transverse stripes. They even form almost perfect rings around the fuselage.
This Skin supply areas of the spinal cord nerves will be as Dermatomes designated.
They are also less clear, but also very systematic Muscles divided among the spinal nerves.
The knowledge of these coverage areas is of enormous importance what the diagnosis of Herniated discs and others Nerve root irritation concerns.
So, due to these diseases occur Pain, abnormal sensation, or muscle weakness always in the area or muscle supplied by the irritated nerve. Complaints caused by a Damage or irritation to a nerve root conditional are called radicular (from the Latin radix = root).
Nerve root irritation
A Irritation of the spinal nerve roots can be caused by various pathological processes in the area of origin of the spinal nerves. In most cases, however, degenerative changes in the spine, i.e. changes caused by wear and tear and age, can be identified as the cause of nerve root irritation.
This includes, for example Foramen stenosis, a narrowing of the intervertebral hole. Although these occur more frequently in old age, they are also caused by a chronic incorrect and overstressing of the spine promoted, which the body tries to balance by strengthening its bony structures.
Long-lasting inflammatory processes in the spinal area can also cause problems Foramen stenosis entail.
The has a similar background Spinal stenosis, a narrowing of the spinal canal. This usually takes place through bony outgrowths on the vertebral bodies, which as a result of the Wear of the articular surfaces are formed. However, if they protrude too far into the spinal canal, this can result in a Irritation of the spinal nerve roots or, in severe cases, irritation of the spinal cord.
The non-degenerative causes of nerve root irritation include, for example Spondylolisthesis (Vortex sliding), a very common disease in the western population, which occurs mainly between the ages of 12 and 17.
Here it comes to one Sliding of the vertebral body as a result of a gap in the vertebral arch.
In most cases this will result exercise-related pain. Nerve root irritation can also occur, albeit rarely.
Other non-degenerative causes of radical irritation are also space-occupying processes such as TumorsWith regard to the nerve root irritation, it initially makes no difference whether these are benign or malignant in nature.
Also viral or bacterial inflammation, for example by the herpes virus or the bacterium Borrelia burgdorferi, the causative agent of Lyme disease, lead to nerve root irritation.
In principle, all of these diseases can occur at any height of the spine. However, the one most frequently affected by nerve root irritation is Lumbar spine, followed by the Cervical spine. This is simply due to the fact that these two sections of the spine have to carry very heavy loads in everyday life and are stressed incorrectly in our everyday life, among other things, through frequent sitting.
disc prolapse
Many people suffer from in the course of life serious back pain. However, only about 5% of these ailments are at one disc prolapse (Disc prolapse or even just Prolapse).
Nonetheless, the herniated disc is the most common cause radical pain represent.
The most common disc herniation occurs between the ages of 30 and 50. Like spinal stenosis, disc prolapse is also one of the degenerative spinal diseases.
Each of the 23 intervertebral discs consists of two parts: one gelatinous core and one surrounding him outer fiber ring.
Age-related changes in the structure of the intervertebral discs can cause fine cracks in the latter, through which the gelatinous core begins to bulge if the cracks are sufficiently pronounced.
If the nucleus of the intervertebral disc presses on neural structures, such as the Nerve roots, failure phenomena are the result.
Depending on the height of the Disc prolapse occurs, other symptoms or other locations are to be expected. Since the damage to the intervertebral discs ultimately depends on the load, herniated discs are for the most part heavily loaded Lumbar spine area to be found.
The diagnosis of a herniated disc is first made with the help of the neurological examination. A series of different tests provide the attending physician with a very precise picture of the extent and location of the incident.
The suspicion of a herniated disc is subsequently carried out imaging diagnostics as the Computed tomography or the Magnetic resonance imaging approved.
Treatment is then given in nine out of ten cases conservative. So surgery is rarely necessary.
The conservative therapy consists mainly of Back training and exercise therapy. Bed rest, as it was recommended in the past for herniated discs, is now considered a disadvantage. Instead, an attempt is made to reintegrate the patient into everyday life as early as possible, which is done with the help of an adequate Pain therapy is achieved. In some cases it can also inject one Local anesthetic in combination with a Glucocorticoid near the affected nerve root may be useful.
L5 syndrome
If the spinal nerve roots at the level of the fifth lumbar vertebra (L5) are affected by irritation, a characteristic symptom complex results, which is also known as the L5 syndrome.
The L5 syndrome is mainly characterized by pain along the back of the thigh, the outside of the knee, the lower leg to the back of the foot and the big toe.
As in other parts of the spine, the most common cause of nerve root irritation at this level is herniated discs.
Should actually be a Prolapse If the intervertebral disc is responsible for the nerve root irritation, the pain mainly increases depending on the load. Likewise, increases in pressure in the abdomen, for example from sneezing or coughing, lead to an increase in pain.
In the case of a tumor, the symptoms tend to worsen at rest. Sensory disturbances such as tingling or numbness may occur in the same area where the pain occurs.
In the case of pronounced damage to the roots, in addition to damage to the sensory nerve fibers, there is also impairment of motor pathways.
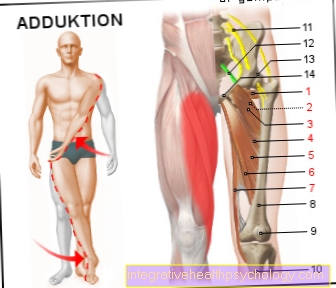
As a result, certain muscles that are responsible for lifting the foot and the big toe and spreading the leg can become weak.
Damage to motor fibers is always a warning sign and should urgently result in treatment, as otherwise permanent nerve damage is to be feared.
The treatment of nerve root irritation at the level of the fifth lumbar vertebra depends on its cause. A tumor usually requires surgical removal, while a herniated disc in most cases is treated purely conservatively, i.e. with physiotherapy and medication.
Read more about this under
- Herniated disc of the lumbar spine
- L5 syndrome
L4 syndrome
A Root damage or irritation at the level of the fourth lumbar vertebra (L4) leads to characteristic symptoms, which are called L4 syndrome be summarized.
This syndrome is mainly characterized by pain in the front and central part of the thigh, the front of the knee and the front and central part of the lower leg.
As in other parts of the spine, the most common cause of root damage is the disc prolapse. In many cases, whether this is actually the case can also be seen in the clinical picture and the severity and localization of the symptoms.
In the event of a herniated disc, the pain increases when exposed to stress. An increase in pressure in the abdominal cavity, such as occurs when coughing, sneezing and pressing the abdomen, leads to an increase in symptoms in this case.
If a tumor were responsible for the root irritation, the pain would intensify, especially at rest.
In addition to pain, it can also cause pain in the skin areas described above Sensory disturbances such as tingling or numbness.
If the nerve root irritation is correspondingly strong, it can also damage the sensory pathways Motor nerve fiber impairments occur. This is expressed in a Thigh muscle weakness, as a result of which it is difficult or impossible to stretch the knee and it is also difficult to pull the thigh in the hip. The placement of the corresponding thigh on the other is also impaired.
Motor fiber damage should always be viewed as a warning sign and treated quickly to avoid permanent nerve damage.
The treatment of nerve root irritation at the level of the fifth lumbar vertebra depends on its cause.
So requires one tumor an operative removal of the same while a disc prolapse in most cases it is treated purely conservatively, i.e. with physiotherapy and medication.
Sacral spine
The nerve fibers originating in the spinal cord segment S1 at the level of the first sacral vertebra are in the formation of the Sacral plexus involved, a network of nerves that is primarily responsible for supplying the gluteal muscles and the rear thigh muscles.
In the event of damage to the nerve root at the level of S1, flexion in the knee joint and extension of the thigh in the hip are accordingly more difficult.
Since with the Triceps surae muscle the calf muscles are also supplied, walking on tiptoe is difficult and the Achilles tendon reflex is weakened or even eliminated.
However, the pain caused by the damage to the roots is much more obvious to the patient and the treating physician. These radiate into the areas supplied by the first spinal nerve, which are mainly located on the back and side of the upper and lower legs and on the outer edge of the foot. Sensitivity disorders such as tingling or numbness can also occur in the same skin areas.
The most common cause of nerve root irritation is the herniated disc. If a prolapse is actually responsible for the nerve root irritation, the pain increases mainly depending on the load.
Sneezing and coughing and performing an abdominal crunch also lead to an increase in pain due to the pressure increase in the abdominal cavity.
In the case of a tumor, the symptoms of nerve root irritation intensify, especially at rest.
The treatment of spinal nerve root irritation at the level of the first sacral vertebra depends on its cause and can be conservative or surgical.
Cervical spine
The spinal nerves, which are attached to the spinal cord segment at the level of the seventh cervical vertebra (C7) are involved in the formation of an as Brachial plexus called nerve plexus involved.
From this go sensory and motor nerve fibers for the Arms, shoulders and chest emerged.
A herniated disc at this level of the spinal cord results in muscle weakness in muscle groups in these parts of the body.
The is particularly badly affected Triceps brachialis musclewhat based on the Triceps tendon reflex can be checked. If it is eliminated or at least greatly weakened, this indicates a disk prolapse at the level of C7.
Furthermore, root damage on C7 leads to pain on the back shoulder, which can extend over the outside of the forearm to the index and middle fingers. In these areas it can also be too Sensory disturbances such as tingling or numbness come.
The most common cause of nerve root irritation is here as well as in other spinal cord sections disc prolapse. The symptoms caused by it increase mainly depending on the load.
In the case of nerve root irritation by a tumor, the symptoms would instead intensify at rest.