Retinal detachment
Synonyms
Medical: Amotio retinae, Ablatio retinae
Definition of retinal detachment
Retinal detachment is a lifting of the retina from the fundus, i.e. the pigment epithelium (choroid). The detachment can affect the entire retina.

Epidemiology
The Retinal detachment is a relatively rare disease. However, it is very important because if left untreated, it leads to Amotio retinae to Blindness.
This disease occurs much more frequently in old age than in young people. In myopic people (from - 6 Diopters = severe nearsightedness) retinal detachment is at least three times as frequent as in people with normal vision. This is due to the fact that the eyes of nearsighted patients (nearsightedness) are longer in longitudinal section than normal-sighted eyes. From a purely anatomical point of view, the risk of retinal detachment is thus higher.
Familiar accumulation can also be observed.
What is the classification of a retinal detachment?
Primary retinal ablation
This retinal detachment of unknown cause is the most common form of ablatio.The tear in the retina tends to develop in the periphery, not in the center.
The reason for this is the detachment of the vitreous humor in old age or with nearsightedness. This creates a pull on the retina, which tears the retina. These tears are seen much more often in the upper half of the retina than in the lower half. This is due to the falling glass body following the force of gravity.
Giant tear ablation
A special form of retinal tears is Giant tear amotio. The cracks can grow so large that they affect over a quarter of the eye. The second eye is always at risk.
Secondary retinal ablation
This detachment of the retina occurs secondary, i.e. due to a cause that determines it. There is usually a history of diabetes. Other causes can be:
- Retinal vein occlusions
- Consequences of premature retinopathy
- Inflammation
- Retinal surgery
- Bruises of the eye (can still be symptomatic years later)
- Perforating injuries to the eye
Exudative retinal detachment
Here there is a disturbance of the vascular permeability. Fluid collects between the pigment epithelium and the retina.

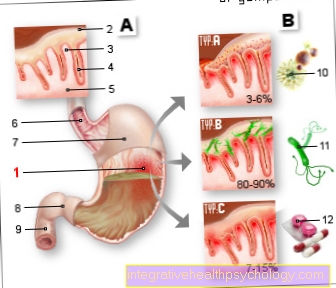
Figure eyeball
- Optic nerve (optic nerve)
- Cornea
- lens
- anterior chamber
- Ciliary muscle
- Vitreous
- Retina
Detecting retinal detachment
What are the symptoms of retinal detachment?
The patients report about "Flashes of light". These result from the pull on the retina. Then the patients notice "Soot rain" or one "Swarm of mosquitoes“.
Both represent the shadows of vitreous hemorrhage that occur when the retina is torn. If the retina becomes detached after the tears, the patient will notice shadows in the field of vision. So you no longer have a normal field of vision that you can perceive the impressions of your entire environment. Parts are missing. For example, the lateral part can be missing, so that the patient cannot see everything on the outside of the affected eye (med. Temporal). An ophthalmologist can intervene here with an eye test.
A flicker in front of the eyes is often mistaken for flashes of light. However, a flicker speaks more for a migraine and not for a retinal detachment. The accompanying complaints that occur can help to differentiate. Retinal detachment is usually painless. A migraine, on the other hand, is usually associated with severe headache and possibly eye, jaw or neck pain. If these symptoms occur, among other things, retinal detachment is probably not the cause of the flicker in front of the eye.
Read more on the topic: Retinal detachment symptoms and eye pain
How is retinal detachment diagnosed?
A retinal detachment can be recognized by typical symptoms. This includes the occurrence of flashes of light, which are particularly evident at dusk or in the dark. Some people also describe a lateral glow in the eye, which has an arch-like shape. The flashes of light and the glow become more intense as you move your head. Shadows can be perceived in the eye, which are described as a wall or a growing bubble. The perception of a kind of soot rain or a swarm of black mosquitoes are further signs of retinal detachment. Some people describe other sudden changes in their vision, such as seeing spider web. It is also characteristic that the retinal detachment is painless, as the retina has no pain fibers. This often allows them to be distinguished from other eye and head diseases. Sometimes it is difficult to distinguish it from vitreous detachment. If the symptoms mentioned above occur, a doctor should always be consulted.
The ophthalmologist (specialist in ophthalmology) can determine whether the retina has been detached by reflecting the fundus.
For this purpose, eye drops are first applied, which dilate the pupil. This allows the examiner a better insight and overview of the fundus. The reflection is done with the help of a magnifying glass and a light source. If the retina is detached, then the retinal tear must be looked for.
In addition to the reflection, the retina can also be diagnosed with a detachment of the retina by means of an examination called OCT (Optical Coherence Tomography). Here the retina is shown especially at the point of sharpest vision. Actually, this examination is more specialized in the detection of macular edema (accumulation of fluid under the retina at the point of sharpest vision).
The ultrasound of the eyes can also provide information about a retinal detachment.
Treating retinal detachment
Can a retinal detachment be treated surgically?
There are several methods of surgically treating retinal detachment. All procedures are based on 3 basic goals: The vitreous body should be relieved, the retina should be closed and an artificial scar should be created.
Depending on the type of retinal inflammation, the procedure is different. If the retinal detachment is uncomplicated, a denting operation is usually performed. A silicone seal is sewn onto the dermis of the eye. This seal dents the dermis, the choroid and the pigment epithelium. As a result, contact is made again between them and the detached retina. The conjunctiva is then closed with the seal.
Sometimes instead or in addition a ribbon, a so-called cerlage, is placed around the eye. Holes at the posterior pole cannot be treated with this method. In the case of retinal detachments with a central hole, removing the vitreous and inserting a kind of "internal tamponade" is recommended in some cases. The inner tamponade usually consists of a silicone oil or a gas. The silicone oil is removed after about 3-6 months, while the gas is spontaneously absorbed by the body itself after 8-14 days.
In the case of complicated retinal detachments, indenting surgery and vitreous removal are advisable. An internal tamponade is often used here as well.
Can a retinal detachment be treated with laser?
The laser method is usually painless and has relatively few side effects. But no existing retinal detachment can be treated with the laser. It is only possible to successfully seal off an existing retinal hole or preliminary stages of retinal tears as part of a laser treatment. This is done by arranging laser scars around the hole in the form of a 2 or 3-row chain. The energy of the laser is only absorbed by the choroid and the pigment epithelium. The retina itself cannot absorb the laser energy. However, it can be drawn into the area where it happens, provided it is in contact with the pigment epithelium. This can cause scarring with the pigment epithelium. This is therefore only possible if the retina is still in contact, while the laser is ineffective if the retina has already been detached.
Can retinal detachment be treated conservatively?
There is no drug treatment for retinal detachment. If a preliminary stage of retinal detachment or a predisposition is known, one can try to minimize the risk factors as far as possible. This cannot prevent retinal detachment, but it may reduce the risk. For example, with the colloquial "diabetes", a so-called diabetes mellitus, an adapted lifestyle should be adopted. As this can, among other things, favor a retinal detachment as a long-term consequence. In addition, inadequately healed infections can have a negative impact on the retina. Inflammations should always be cured well. Negative stress and overexertion during sport should be avoided as far as possible if there is a previous stress. The immune system should be strengthened through a balanced diet and lifestyle. Flying should also be reduced or, in some cases, even completely stopped. In the preliminary stages of a retinal detachment, medical consultations and controls are highly recommended.
What should be considered after retinal detachment treatment?
Patients are not allowed to read for a week after treatment. This rule applies to prevent the glass from jerking that occurs when reading. If the retina closes in a few days after the operation, the patient does not have to expect any restrictions in daily life.
If the eye is filled with gas, the affected person must not fly under any circumstances. The gas expands in height and leads to dangerously high intraocular pressure (see also glaucoma). It can even cause an artery occlusion.
Preventing Retinal Detachment
What are the causes of retinal detachment?
The most common causes of retinal detachment include degenerative changes in the retina and vitreous humor that lead to tears in the retina. The retina practically attaches itself to the eye from within. At its origin, it is fused with the underlying pigment epithelium, the choroid. It has also grown together with its base on the papilla. The papilla is the term used to describe the exit of the nerve fibers of the optic nerve from the eye. If there is now a hole in the retina, fluid can collect underneath. Such holes can have various causes:
- Retinal and vitreous shrinkage
- Injury to the eyeball
- diabetic retinopathy
Severely myopic people are particularly at risk. Your eyeball is particularly long and thus favors the detachment of the retina, as it is very stretched.
Statistically speaking, there is also an increased risk after cataract surgery (cataract surgery), i.e. removal of the lens, which is usually cloudy due to age.
How can you prevent retinal detachment?
The preliminary stage of retinal detachment are cracks in the retina. These must be recognized through regular visits to the ophthalmologist. These cracks can be scarred by means of a laser (they practically stick to the underlying choroid) and thus prevent further detachment of the retina. Particularly myopic people (nearsightedness) and patients who have already suffered from retinal detachment should be particularly careful and have the retina thoroughly examined by the ophthalmologist as regularly as possible.
Course of retinal detachment
What is the prognosis for retinal detachment?
The prognosis depends on the severity of the retinal detachment. With an uncomplicated replacement, success of up to 90% can be recorded. The smaller the retinal detachment and the faster the treatment, the better the prognosis. The prognosis of vision depends on whether the macula (yellow spot = the point of sharpest vision) was impaired.
How long is the duration of a retinal detachment?
When it comes to the duration of retinal detachment, one has to distinguish the duration of this from the duration of a retinal tear or hole. Both an untreated retinal detachment and an untreated retinal tear or hole do not heal on their own. If the adjacent retinal hole is lasered, it can take about 2 weeks for a scar to form. This scar is supposed to prevent retinal detachment. On the other hand, with an operation to detach the retina, it takes a few days for the retina to become firmly attached and a scar to form. After about 2-3 weeks after the operation, the person affected can calmly and unreservedly continue their lifestyle.
How long it takes for the achievable vision to be regained depends on various circumstances. The regeneration of the retina is influenced by the extent and duration of the retinal detachment. How long the so-called macula (the yellow spot) was raised also plays a role. It often takes weeks or months for the eyesight to improve satisfactorily after the operation. After prolonged macular detachment, it can take up to a year for vision to be regained to an achievable level. Untreated retinal tears, holes or detachments have a progressive course. That is, they last without therapy.
How long do retinal detachment symptoms last?
Vitreous hemorrhage and retinal detachment often occur together. In this case, the discomfort caused by the vitreous hemorrhage may subside as the bleeding heals. The duration of the regression of the bleeding and the accompanying symptoms is very variable. The duration depends on the extent of the bleeding and other individual factors. The discomfort caused by the retinal detachment itself does not go away on its own. Only through an operation is it possible to contain the symptoms.
What are the chances of recovery from a retinal detachment?
Retinal detachment can only be treated successfully with surgery. According to some authors, an uncomplicated retinal detachment could be successfully treated in 85-95% of the cases using the indenting method. The chances of recovery increase the earlier the retinal damage is recognized and treated. If the retinal detachment is complicated and / or in combination with other eye diseases, the diagnosis is less favorable. However, with the help of the vitreous body removal and the insertion of an internal tamponade, satisfactory visual improvements can often be achieved. The extent to which the visual performance improves in each case depends on many factors.
Further questions about retinal detachment
Can stress trigger retinal detachment?
Some studies show that stress could play a role in retinal detachment. There are suspected connections with an increased release of the hormone cortisol. It is believed that many different factors are associated with retinal detachment. If the retina is preloaded, stress could be a risk factor in promoting retinal detachment. Stress as the sole or general cause of retinal detachment is unlikely.
Can a retinal detachment be triggered by a vitreous hemorrhage?
A retinal detachment can develop from a vitreous hemorrhage. The vitreous humor of the eye borders on the retina at the back and attaches there. Due to this connection, a vitreous detachment can affect the retina. As a result, a vitreous detachment can trigger a pull on the vessels. If the lift-off happens suddenly, the pulling force can tear the vessels. This can lead to vitreous hemorrhage and cause a retinal tear or hole. Should liquid then wash under the retina, there is a risk that it will peel off.
You may also be interested in this topic: Vitreous detachment