Neuroborreliosis - What is it?
introduction
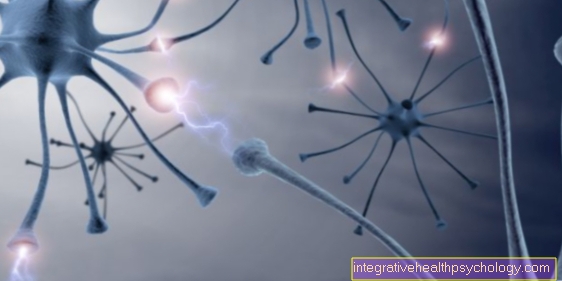
Neuroborreliosis is a form of borreliosis that is caused by bacteria Borrelia burgdorferi is triggered. The bacterium is most frequently transmitted to humans in Europe through tick bites.
Borreliosis is most often expressed by the so-called wandering redness (Erythema migrans), a rash after a tick bite, but half of patients with Lyme disease also develop neuroborreliosis.
Meningitis (meningitis) as well as various other neurological complaints.
The reasons
Neuroborreliosis is caused by an infection with the Borrelia burgdorferi bacterium. In Europe, the pathogens most frequently enter the patient's body through a tick bite. The common wooden goat (Ixodes ricinus) is the main carrier of the bacteria.
In contrast to early summer meningoencephalitis (TBE), which can also be triggered by tick bites and whose high-risk area is concentrated in southern Germany, borreliosis is widespread throughout Germany.
The transmission of Borrelia from ticks to humans begins no earlier than six hours after the animal is bitten. The longer the tick stays on the patient, the higher the risk of Borrelia being transmitted. In addition, if the tick is improperly removed, the pathogen is often transmitted, for example if the tick is squeezed out during removal.
Find out all about the topic here: The tick bite.
The symptoms
Neuroborreliosis usually only develops a few weeks to months after infection with the bacterium Borrelia burgdorferi. Up to 95% of cases are manifested by meningitis (meningitis). The affected person often suffers from headaches, fever and stiff neck. Nerve roots can also be affected by the inflammatory process, which can manifest itself through paralysis, sensory disorders and pain. Unilateral or bilateral facial paralysis is not uncommon when the facial nerve is affected (facial paralysis).
Symptoms usually resolve within six months. In the remaining 5-10% of patients, not only the meninges and nerve roots become inflamed, but also the brain and spinal cord. Affected patients develop gait disorders, dizziness, balance disorders, epileptic seizures, incontinence, hallucinations, speech and hearing difficulties, extreme tiredness or other psychological symptoms. Concentration and memory are often restricted. Relatives or acquaintances of the patient sometimes notice a change in character. Processes that directly affect the brain are usually more protracted than when the meninges are involved alone.
Read more on the topic:
- Neuroborreliosis can be recognized by these symptoms.
- Facial palsy
The diagnosis
The most important indication of a possible neuroborreliosis is a past tick bite. If the doctor is informed about such a condition and the patient shows typical symptoms for neuroborreliosis, then nerve fluid (liquor) can be taken to confirm the diagnosis. To do this, a cannula is inserted into the spinal canal between the extensions of the vertebral bodies on the back and some liquor is drained off. This can then be examined in the laboratory.
In neuroborreliosis, there are typically more white blood cells in the CSF to fight the infection. There is also an increased level of antibodies against the pathogen.In some cases it can be difficult to diagnose neuroborreliosis with certainty, as there are often no inflammation levels in the nerve water, especially in the early stages. It can also take a while for antibody production to begin.
In order to rule out other causes for the patient's symptoms, imaging is often requested (e.g. CT, MRI of the brain). If the brain itself is affected, multiple sclerosis-like lesions can often be observed in the imaging.
CSF diagnostics in neuroborreliosis
The nerve fluid that surrounds the brain and spinal cord is called liquor. The nerve water is obtained as part of a lumbar puncture for CSF diagnostics.
In the case of neuroborreliosis, there are often indications of the infection in the CSF, for example an increased number of white blood cells, an increased level of antibodies against the pathogen Borrelia burgdorferi and sometimes increased protein levels. Especially when the antibody level in the liquor is higher than in the blood, this is an indication of neuroborreliosis.
However, especially in the early stages of the disease, the changes in the CSF can also be absent, so that the CSF examination / CSF diagnostics cannot be 100% relied on for the diagnosis.
Read more on the subject at: CSF diagnostics
The MRI for neuroborreliosis
In neuroborreliosis, changes can sometimes be detected in magnetic resonance imaging (MRI of the brain).
When the brain is infected, damage to the white matter of the brain often shows up, which can look similar to that in multiple sclerosis (MS).
If the meninges are predominantly affected, an accumulation of contrast agent can be observed there in the imaging.
Read more on this topic at: MRI of the brain.
How is neuroborreliosis different from MS?
In order to adequately differentiate neuroborreliosis from multiple sclerosis, different investigations and factors must be taken into account. This includes the differentiation of the disease circumstances, the complaints, findings, magnetic resonance tomography, electrophysiological examinations, liquor diagnostics, laboratory examinations, ophthalmological examinations, scintigraphy and examinations of the heart.
The onset of the disease in multiple sclerosis is between the ages of 23-30 or 35-40, depending on the form. There may be a genetic predisposition. Some authors suggest a relationship between infectious diseases and multiple sclerosis. Other authors can also imagine a connection to intestinal diseases. As far as we know today, the disease only affects the central nervous system. On the other hand, neuroborreliosis can develop at any age. A tick bite is the trigger for neuroborreliosis. The risk of infection can vary due to individual and genetic factors. The disease is not just limited to the CNS, but can manifest in other organs.
The symptoms of neuroborreliosis and multiple sclerosis can be very similar. With neuroborreliosis, however, facial paralysis, myocarditis and other symptoms and abnormalities in the heart, skin changes, damage to the liver, gastrointestinal tract, urogenital system, pharynx, lungs and sinuses can usually be identified . With multiple sclerosis, these symptoms usually do not show up. Multiple sclerosis, on the other hand, is characterized by the Charcot triad. All other symptoms are very similar, so that no differentiation can be made based on the symptoms alone.
However, one can distinguish the course. Multiple sclerosis is characterized by intervals of relapses and phases of remission. As a rule, the onset of illness is sudden, within minutes or hours or a maximum of days. However, weeks to months before the onset, multiple sclerosis can manifest itself with unspecific symptoms such as tiredness, weight loss, a general feeling of illness and muscle and joint pain. In contrast, the neurological symptoms of acute neuroborreliosis develop more slowly within days. The resolution of symptoms can take weeks to years. Residual symptoms and long-term damage can be retained. In chronic neuroborreliosis, the symptoms are less pronounced than in the acute form. But in contrast to multiple sclerosis, there are no completely symptom-free phases.
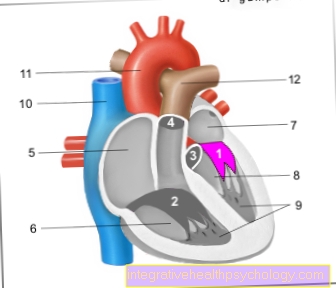
Often no significant differences can be seen in magnetic resonance imaging. In the CSF diagnostics, specific antibodies against Borrelia can sometimes be detected in neuroborreliosis. But if no antibodies are detectable, this is still not a safe exclusion criterion. It is important to remember that the antibodies are only detectable a few weeks later after the event. However, certain signal proteins can be detected in the early stages of neuroborreliosis. In addition, other methods can show a typical picture of neuroborreliosis. But this is not the case in all cases either. With a very precise ophthalmological examination, the different eye complaints of neuroborreliosis or multiple sclerosis can sometimes be assigned appropriately. In a further examination, a scintigraphy of the scintillator, in neuroborreliosis, nuclide accumulations can be found in various joints in arthritis. But even this cannot be used as a certain individual differentiator. The heart can be examined using different methods. Multiple sclerosis does not usually cause heart problems. In contrast, with neuroborreliosis, various limitations and damage to the heart are not uncommon. In order to differentiate neuroborreliosis from multiple sclerosis, a comprehensive examination and several criteria are required.
The so-called McDonald criteria can be used to reliably rule out or determine multiple sclerosis. These describe the important characteristics of multiple sclerosis.
Find out all about the topic here: Diagnosis of multiple sclerosis.
What is the typical course?
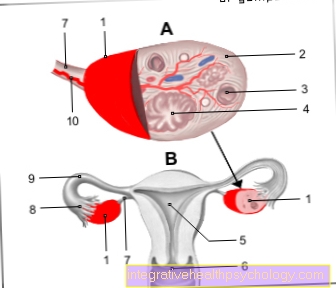
There are 3 stages. In the first stage, skin changes appear at the site of the tick bite. In some cases, red, raised skin appearances on other parts of the body. Accompanying this can be increased temperature, tiredness, a general feeling of illness, headache and muscle pain, swelling of the liver and spleen, conjunctivitis and blood in the urine. In this phase the "nerve water", the liquor, is inconspicuous. The 1st stage lasts about a few weeks to months.
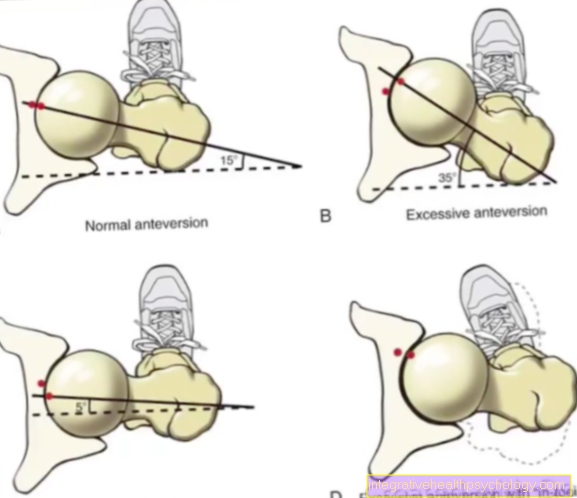
One month after the tick bite event, the first stage changes to the second stage. The disease now generalizes. The skin symptoms persist. In addition, those affected often complain of very severe radicular pain in the trunk, arms and legs. Paralysis occurs about 2 weeks after the onset of pain, usually affecting the facial muscles and a certain eye muscle that turns the eyes outwards. It can also cause muscle and joint pain, as well as damage to the eyes, liver and heart.
In the third stage, the chronic complaints mentioned above develop.
Symptoms of chronic neuroborreliosis
In about 5-10%, the neuroborreliosis goes into a third stage. At this stage, chronic inflammation of the spinal cord and brain develops, causing characteristic symptoms. The technical jargon also speaks of progressive encephalomyelitis. This can occur in stages and last for months to years.
Chronic neuroborreliosis can be recognized by various cognitive limitations, as well as speech, hearing, gait, coordination, movement and urination disorders. Inflammation of the blood vessels can lead to a stroke. In addition, a sensory disorder with numbness and abnormal sensations can develop. This is also known as chronic polyneuropathy. In addition, in rare cases, chronic seizures, hallucinations and impaired consciousness can occur.
Read more about the topic here: Inflammation of the spinal cord.
What are the stages of neuroborreliosis?
There are 3 stages of neuroborreliosis in which typical symptoms appear
The 1st stage is also known as the local infection stage. This means that at this stage local / local infection occurs. The 2nd stage is also called the generalization or scattering stage. At this stage, the pathogen reaches other areas of the body through the blood. Stage 3 is the late stage
The therapy
Since neuroborreliosis is a bacterial infectious disease, it is treated with antibiotics. Suitable preparations are penicillins, cephalosporins and doxycycline. The drug treatment usually lasts about three weeks.
In severe forms, especially if the brain was also affected, permanent damage can also occur.
Read more on the topic: Treatment of borreliosis.
What does the therapy look like in the late stage?
Therapy in the late stage consists of various measures. Usually antibiotics are used. In the late stage, treatment with intravenous penicillin G is recommended for 2-3 weeks or, in the case of penicillin allergy, therapy with cephalosporins is recommended for 2-4 weeks.
In addition, individually symptomatic, drug and non-drug therapies may be advisable. For example, ergotherapy, physiotherapy and speech therapy can be indicated. The aim of these therapies is to preserve existing skills and expand resources. The focus is on improving the quality of life and maintaining the greatest possible independence in all areas of life.
It is also important that relatives are advised and instructed by the therapists and doctors. In some cases, aids are also required and adequate advice on aids is required.
Prognosis
The prognosis and the chances of a cure in neuroborreliosis depend on the severity of the disease. In the case of a form that only affects the meninges, the prognosis is good overall with timely antibiotic therapy.
If the brain is also affected, permanent damage occurs more often, for example in the form of symptoms of paralysis or numbness. If the disease is recognized too late or not recognized, a chronic course can develop, which can also manifest itself in relapsing forms.
Long-term effects of neuroborreliosis
If the symptoms from stage 2 neuroborreliosis are not healed sufficiently, damage to the joints and thus arthritis can result. It can also damage the liver, heart and eyes. If necessary, paralysis, such as facial paralysis, persists.
In addition, some authors discuss a post-Lyme disease syndrome, which is also referred to as "fibromalgia-like" symptoms or "chronic fatigue". This describes unspecific complaints after a neuroborreliosis. The symptom complex includes tiredness, poor concentration and lack of drive. Whether these complaints are actually related to neuroborreliosis is controversial.
The prophylaxis
In contrast to early summer meningoencephalitis (TBE) there is no vaccination against Lyme disease. Accordingly, you cannot get medical protection against neuroborreliosis either. So the most important prophylaxis focuses on avoiding tick bites. When you are in the great outdoors, it is best to wear long clothes and closed shoes.
Most ticks are found near the ground in the grass or on bushes, where they are stripped off by the patient as they pass. Light-colored clothing can help spot the dark ticks faster. After a day in the great outdoors, you should check your whole body for ticks as soon as possible. The faster a tick is removed, the lower the risk of the transmission of pathogens. Even if you have already had a Borrelia infection, there is no subsequent immunity.
Read more on the topic: Tick bite.
Is neuroborreliosis contagious?
Neuroborreliosis is transmitted via ticks that are infected with Borrelia. Infection from person to person is not possible. The risk of infection depends on the region, but overall not very high.
For more information, read on: Is Lyme Disease Contagious?




.jpg)