Open leg
introduction
The so-called open leg, also called ulcus cruris, is one of the greatest challenges in medicine with almost a million affected patients and sometimes very protracted processes.
Due to the relatively frequent occurrence and the complex treatment, the open leg is also a cost factor for health insurance companies that should not be underestimated. Since mainly older patients with many other previous illnesses (multimorbid patients) have to struggle with this, no stagnation but rather a further increase in the number of cases is to be expected in the near future.

root cause
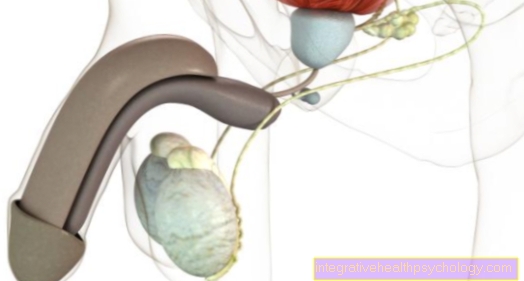
The leg ulcer is often based on a venous disease as the primary cause. However, it can also be triggered by diseases of the arteries or a combination of both factors. In rare cases, open legs can also have other causes. This includes infections that heal poorly and / or are treated incorrectly, some blood diseases, joint damage and also, for example, cancer of the affected tissue.
In general, however, as already described above, the cause lies within the blood supply system. Due to the disruption in the vascular system, there is an undersupply of the tissue on the leg or a disturbed drainage and thus a build-up of blood. In the most common case (around 80% of cases) the cause is a weak vein, which means that used blood from the legs is no longer pumped back to the heart effectively enough. The congestion of blood initially causes edema (swelling of the leg due to increased water retention) in the area of the lower leg. The skin and the underlying tissue become hardened and overstretched.
This backwater slows the blood flow in the leg or even allows it to dry up completely. Without the blood flow as a transport system, the tissue lacks important nutrients and above all oxygen. Waste products accumulate. This last step can also be observed in an arterial open leg; in this case, the arteries themselves, due to the changes that they have undergone as part of an illness and that make them calcified and narrow, prevent the legs and feet from being adequately supplied with oxygenated blood.
You might also be interested in these topics:
- arteriosclerosis
- Chronic venous insufficiency
diabetes
An extreme risk factor for an arterial open leg is the diabetes mellitus. Like high blood pressure, smoking and greatly increased blood lipid levels (hyperlipidemia), they promote arteriosclerotic processes that permanently damage the arteries.
In addition, diabetes mellitus leads to a reduction in pain and pressure sensations in the foot area (diabetic polyneuropathy). Undiscovered minor injuries can then, in combination with a corresponding circulatory disorder, turn into lengthy open wounds. It is therefore important that diabetics regularly examine their feet and legs themselves and look out for changes in the skin and other signs of circulatory disorders. Finally, the increased sugar content in the tissue of the entire body due to diabetes mellitus also promotes the development of a leg ulcer, since bacteria can multiply much better and faster in a sugar-containing environment after entering the body.
After a thrombosis
A thrombosis is a blood clot that lodges in a vessel and blocks it.
If this happens in a vein, the blood can no longer be transported away and fluid builds up. Similar to a weak vein, tissue damage occurs and, as a result, open areas on the leg. Characteristically, a thrombosis also leads to overheating of the affected leg, which is an indication of inflammatory processes.
- Thrombosis in the leg
- Post-thrombotic syndrome
Symptoms
Typical symptoms of the open leg are skin changes on the lower leg; these can appear as pigment spots or as a yellowish-brown discoloration. These are often associated with eczema of the skin, which can ooze, and varying degrees of itching.
Over time, the skin loses its elasticity and appears hard, before finally there is an (rarely more than one) open area that no longer heals. If such a defect has existed for more than 6 weeks without any signs of healing, it is called an open leg. In addition, there may have been long-standing and frequent leg swelling in the past. The legs felt limp and tired. In some cases, a wreath of veins is already visible on the edges of the foot in this preliminary stage. This is understood to be a spider web-like vascular drawing, which can often be observed on the inner edge of the foot and the inner ankles.
Pain in an open leg
An open leg usually arises on the basis of a weak vein. Fluid accumulates in the feet and lower legs over a longer period of time. This water retention causes the skin to feel tight, but it can also cause pain.
At some point the tissue is so badly damaged that open areas arise. Suddenly there is no protective skin left, so that external influences such as touch, pressure, heat or cold hit the pain-conducting nerve fibers much more directly. As a result, they often cause disproportionate pain.
In addition, the open areas become easily inflamed, which also causes pain. At the same time as the damage to the tissue, however, there is often damage to the nerve fibers. If these are only partially damaged, they can convey misinformation to the brain, which is why actually harmless stimuli are suddenly interpreted as pain. If the nerve fibers are completely destroyed, the opposite occurs: The brain no longer receives any information from the affected area, so a feeling of numbness occurs and pain is no longer felt.
Unpleasant smell
If an open leg starts to smell bad, it indicates a colonization of the tissue with bacteria or dead tissue.
Due to the lack of blood circulation and the poor protection of the open area, such infections can develop very quickly. In this case, it is imperative to consult a doctor who can initiate suitable therapy against the bacterial colonization. In an emergency, part of the tissue must be cut out to prevent infection.
Water leakage
In most cases, the cause of an open leg is weakness in the veins. Veins are the vessels that are supposed to transport blood from the legs back to the heart. Since this transport must arrive against gravity, so-called venous valves are located in these vessels. They let blood up against gravity and then prevent it from flowing back into the feet.
Often, however, these venous valves fail in old age, which is why the blood constantly sinks back into the feet. Without this venous return flow, however, many waste materials are not removed from the legs, instead they attack the tissue. The extra pressure from the liquid also damages the tissue. This leads to open spots on the legs and feet over time. Since the skin no longer holds the jammed fluid in the tissue, water escapes.
On the other hand, therapeutic measures such as good wound care help. Wound dressings are used to prevent the liquid from escaping. Wrapping your legs is also helpful to prevent further water retention.
therapy
Depending on the cause of the open leg, there is a different therapy for the patient. For this reason, the exact differentiation of the type when making a diagnosis by a doctor is of great importance for further treatment.
Venous leg ulcers, which usually occur on the ankle (usually on the inside) and which are often preceded by long-standing suffering with varicose veins and / or venous thrombosis, should be treated with strong compression. Solid bandages or compression stockings are suitable for this. Regular walking training and any removal or interruption of varicose veins or poorly functioning veins complete the therapy concept. The latter measure, however, requires an operative intervention.
On the other hand, the situation is quite different with open legs with an arterial cause; These wounds, which often appear for the first time on the toes, heels or balls of the feet and can be very painful, should not be compressed any further. Compression would also decrease the remaining blood flow, making symptoms worse. In the treatment of these ulcera cruri, the main focus is on the expansion of the arterial vessels. Surgical expansion or bridging of the constriction with vascular prostheses or bypasses are conceivable. However, these operations are not always feasible and useful. An experienced doctor should carefully identify the indication for therapy and advise the patient in detail.
With all forms of open legs, it is of course at least as important to treat the wound itself at the same time. It must be cleaned regularly and covered with special dressing material that keeps the wound bed slightly damp (not wet!) At all times and thus can promote healing. It may be possible to approach the wound surgically: the removal of the old wound surface is followed by cleaning of the wound base (debridement) under light or local anesthesia. Then it can make sense to close the defect with a skin graft. However, this type of treatment is only possible if the vascular supply in the affected leg is so good that the operating surgeon can be sure that the skin graft will grow. If the blood circulation is very poor and no improvement can be achieved in the healing process, the application of specially grown fly maggots (free or packed in special bags) is recommended. These only eat away the dead tissue and thus clean the wound very effectively. The healthy tissue remains complete.
Since all these factors have to be considered when making a therapy decision and decisions in this regard are not always easy to make, self-chosen therapy is strictly inadvisable; On the one hand, the reason for the open leg must be clearly defined and also treated and, on the other hand, a doctor can prescribe specific aids and precisely guide the treatment and the further procedure. Many over-the-counter medications or home remedies are also suspected of triggering severe allergies or even worsening the symptoms of those affected.
You might also be interested in these topics:
- Therapy of peripheral arterial occlusive disease
- Removal of varicose veins
Which ointments can help?
An open leg that is not caused by an acute injury is usually caused by changes in the vascular system. As a result of these diseases, open areas arise that then heal very poorly and slowly.
Bandages must be applied to protect the open tissue. However, wound dressings and ointments should be applied to the tissue beforehand. Since an open leg is usually a symptom of a serious illness and the open leg in turn harbors many dangers such as infections, the open areas should definitely be treated professionally.
Experimentation without prior medical advice should definitely be avoided. Experts usually use a zinc paste to treat the open leg. This is primarily intended to protect the surrounding tissue from infections. Usually, a wound pad is also applied to the open area. This contains a gel or a foam that offers molecular structures in which newly formed tissue can find support. This supports the body's self-healing powers. In doing so, substances such as hydrocolloids, hydrogels, alginates or polyurethane foam are used.
Treatment with maggots
Maggots are often used to treat an open leg. Because of the poor supply of nutrients to the tissue, many cells die there. However, the body cannot eliminate them all. Maggots, on the other hand, like to eat away this dead tissue, but leave the intact tissue alone and are therefore ideally suited to cleaning up the open areas. The maggots are not brought directly into the wound but are placed in special bags in the open areas.
Home remedies
In addition to professional wound treatments, home remedies can be a good addition to therapy.
For example, you can use a topping with witch hazel extract. Envelopes with curd cheese or fenugreek can also help. An overlay soaked in a marigold infusion can also be used. Other herbal remedies that are used are bindweed, comfrey, oak bark tea and arnica.
Honey for treatment
Medicinal honey can be used to treat open legs. This is placed on a wound pad so that it can be applied directly to the open area.
Many manufacturers sell wound dressings soaked in medical honey. The honey can also be purchased as a wound gel. The effect of honey is both wound cleansing and antibacterial. In addition, the honey can mask and eliminate unpleasant smells.
amputation
The amputation of a body part is always the final stage of a treatment sequence. This alternative would only be considered in the event of absolute therapy failure or tissue that can no longer be saved.
Unfortunately, the existing circulatory disorder often caused a great deal of damage to the tissue over a very long time, so that amputation of more or less large parts of the leg is the last option.This can be the amputation of individual toes, the removal of the entire forefoot or even the entire foot with or without parts of the lower leg. However, as long as there are other options available, everything would be done to use them and to preserve the leg if possible.
Nonetheless, some patients report the relief they have experienced from amputation; the problem is finally resolved. Individual views and theories of illness play just as important a role as advice from the treating doctor and the individual suffering of the individual.
Also read our article:
- Toe amputation
When do you need an amputation?
An amputation is necessary when the open area has become infected and the infection can no longer be tamed. The circulatory disorders that cause open legs also mean that the open areas do not close again. Fighting pathogens is also made more difficult by poor blood circulation. Infections can quickly get out of control.
Another cause of an amputation can be the death of the tissue on the leg.
diagnosis
The diagnosis of an open leg is usually made clinically, i.e. through questioning and examination by the doctor.
A special ultrasound examination of the vessels in the leg (Doppler sonography) and an X-ray examination with contrast agent (phlebography with contrast agent, angiography) can also be helpful for special questions - such as a suspected thrombosis or to assess the arterial status.
In addition, other possible causes for non-healing wounds should also be clarified; a blood sample to discover disorders in the sugar or fat metabolism or in the coagulation system should also be carried out. In addition, a sample can be taken from the affected tissue and examined if there is a suspicion that the vessels are not the cause of the open leg in this case. If, for example, the colonization of the wound with a germ can be detected and the cause of the open leg is this infection, an antibiogram of the pathogen should finally be made in order to start an optimal antibiotic therapy.
Which doctor treats an open leg?
Since an open leg is usually due to vascular diseases, vascular surgeons primarily treat this disease.
If an infection occurs, microbiologists are sometimes called in. In general, doctors from the fields of internal medicine are also involved in the treatment. They are usually more responsible for drug therapy. Wound treatment can also be taken over by a family doctor or his specialist staff.
Duration
The wounds that appear on an open leg are extremely protracted injuries.
With good cooperation from the patient and adequate therapy, healing can be achieved within a few months. If the disease is preceded by arterial problems, it usually progresses more slowly; Venous open legs usually heal faster.
cure
Complete healing of the open leg is quite possible.
However, it can only be achieved with the active help of the patient. It is important here that the person affected knows exactly what to do and is active in supporting the healing process. Last but not least, existing risk factors should be minimized or, in the best case, avoided entirely.
forecast
As already mentioned above, the prognosis of the open leg is highly variable: In any case, it is a protracted, frequently recurring (recurring) disease.
Unfortunately, in many cases it is not possible to achieve consistent cooperation from the patient, in particular which reduces risk factors. Serious complications are rarely to be expected, but an open wound is of course a potential entry point for bacteria, viruses and other pathogens that can lead to inflammation and, in the worst case, to life-threatening blood poisoning (sepsis).
prophylaxis
There are a few simple behaviors that can help you avoid an open leg; If you have known venous disorders, regular compression therapy and frequent walks are advisable.
Remaining immobile in the same position for a long time should be avoided, as should crossing your legs while sitting. The legs should be put up regularly to promote venous blood flow.
In addition, one should reduce risk factors if possible; So avoid smoking, reduce obesity and, if you have known diabetes mellitus, ensure that your blood sugar is controlled well. The blood lipid levels should also be within the normal range. All diabetics are advised to choose suitable, comfortable footwear as well as very careful foot care (ideally by specially trained medical podiatrists). In no case should injuries occur during foot or nail care. Patients in the risk group should consult a doctor at an early stage - i.e. if there are changes in the skin on the ankles or lower legs - and have minor injuries checked regularly.
Find out more:
- Compression stockings
- Quitting Smoking - The Best Practices


.jpg)



.jpg)