Operation of a herniated disc
introduction
Nowadays the indication for surgery is on one disc prolapse only very cautious. As a rule, only acute (medians) Mass incidents (= Mass prolapse), mostly in the area of Lumbar spine With Signs of paralysis, advised to have surgery. This is due, among other things, to the fact that there is a great chance of healing through conservative forms of therapy consists.
In addition to acute paralysis, symptoms of failure to hold water and stool (cauda equina syndrome), there is also a relative indication for surgery if the pain from the herniated disc is caused by a conservative treatment cannot be adequately controlled.

Indications for surgery
If a long-term conservative therapy of the herniated disc does not cause any or only insufficient pain regression, there is a so-called "relative indication for surgery“.
In general, surgical therapy cannot prevent a new incident. A proliferating scar tissue can also call the surgical measure into question, as scar tissue can arise again after an operation, which then presses on nerves or spinal cord like a herniated disc. In this case, one speaks of a post-nucleotomy syndrome.
Find out more about the topic here: When should a herniated disc be operated on?
1. Minimally invasive procedures
Since traditional, open surgical procedures are generally associated with risks and involve a longer stay in hospital, so-called minimally invasive procedures for surgery have been developed.
These minimally invasive procedures can - provided the framework conditions are right - be carried out on an outpatient basis and under local anesthesia. Risks that cannot be ruled out by anesthesia are reduced.
However, minimally invasive procedures cannot be carried out in every stage of the herniated disc disease. Traditionally, this procedure is performed on simple and relatively new intervertebral disc protrusions and prolapses. A sequestration (Protrusion of intervertebral disc tissue) is usually not treated with a minimally invasive approach.
A previous operation is also an exclusion with regard to this type of surgical measure.
That means: Patients who have already been operated on for a herniated disc should not be treated again with this method.
The classic minimally invasive procedures include:
- Chemonucleolysis
- Laser ablation of the intervertebral disc
- Percutaneous nucleotomy
- Microsurgical surgery
1.1 Chemonucleolysis
As Chemonucleosis This is the name given to the chemical liquefaction and the subsequent suction of the inner gelatinous ring of the intervertebral disc.
1.2 Laser ablation of the intervertebral disc
Another therapeutic measure of the herniated disc is laser ablation Intervertebral disc Similar to minimally invasive therapy, this procedure is only for uncomplicated, fresh incidents suitable.
This measure is also based on the principle of volume reduction in the area of the intervertebral disc by means of a medical YAG - (yttrium aluminate garnet) - laser is performed.
1.3 Percutaneous nucleotomy
This procedure is similar to Chemonucleosis to the extent that here, too, a volume reduction takes place by suctioning off the inner gelatinous core. In contrast to chemonucleosis, however, no enzyme is used for liquefaction, but the herniated disc is removed mechanically.
1.4 Microsurgical surgery / minimally invasive surgery (MIS)
Since large skin wounds and large surgical fields usually result in a longer recovery phase for patients after the operation of the herniated disc, minimally invasive surgical Procedure tries to keep the area of intervention as small as possible.
Especially with uncomplicated herniated discs in the area of the Lumbar spine, this procedure can be used and operated well. Over a small cut becomes under Use of a microscope the herniated disc is excised in a minimally invasive manner.
2. Conventional open surgery

More difficult herniated discs can be done using minimally invasive methods (see above) are not treated. These are, for example, herniated discs that affect neurofamina, herniated discs that have existed for a long time or are spread over several floors. In these serious cases, a larger, open access route must be chosen that allows a broader view of the surgical area.
To make this possible, at least part of the Ligamentum flavum removed on one or both sides. One speaks here of a "Windowing“, Which allows access to the intervertebral disc and the nerve root concerned. If you have to depict the nerve roots of two adjacent levels, the distance of one may be necessary Vertebral semicircle or the entire vertebral arch is necessary. This allows you to see all the relevant structures and make them accessible for treatment. The herniated disc can be completely or partially removed. The convalescence (= Recovery) is inevitably longer than with the microsurgical procedure due to the more extensive preparation.
As with all other surgical interventions, scar tissue inevitably develops at the treated area, the extent of which varies from person to person. In the worst case, this scar tissue tends to overgrow, which in turn takes up space and puts pressure on the nerves. In such cases, another surgery to reduce the scar tissue may be necessary (Post-nucleotomy syndrome). Post-nucleotomy syndrome can only be tackled surgically in exceptional cases. Hence, to combat chronic pain only stand conservative therapy methods available.
As part of the therapy for chronic pain, we have developed a program with the pain specialists on our team.
In this area, the progressive muscle relaxation, that is aimed at people who are under chronic Back pain suffer, judges.
For more information, see Progressive Muscle Relaxation.
Painful spinal instability can also develop after clearing out a single disc. Follow-up operations may also be necessary here, e.g. a stiffening operation.
3. Intervertebral disc prosthesis
To an increasing extent, too Intervertebral disc prosthesis are used, which are supposed to imitate the function of a normal intervertebral disc and in particular are supposed to protect against the dreaded spinal instability.
The intervertebral disc prostheses have so far been attested to have a long shelf life, but more extensive research studies are still lacking. It remains to be seen what significance the intervertebral disc prosthesis will have in the future and which type of intervertebral disc prosthesis will ultimately prevail.
Since the topic of intervertebral disc prosthesis is so extensive, it should not only be touched on at this point.
An intervertebral disc prosthesis is only suitable for relatively narrow indications, so the choice of an intervertebral disc prosthesis over a stiffening (spondylodesis) must be carefully considered.
So read on under: Intervertebral disc prosthesis
Duration of a disc surgery
The duration of the operation depends on the surgical method used and also on the severity of the herniated disc.
Minimally invasive interventions that are performed using an endoscope often take between 30 and 60 minutes.
On the other hand, operations on more complicated herniated discs or those that affect several vertebral bodies can take longer than 120 minutes.
After the operation, the patient usually remains in the hospital for about a week. The stay can also vary depending on the surgical method and the individual healing process.During this time, the patient is supported with the help of physiotherapy to move correctly again.
A longer period of regeneration is often planned even after the hospital stay.
Some patients go to a rehabilitation clinic, others take advantage of outpatient physiotherapy.
The duration of the sick leave depends on the follow-up treatment and can sometimes be necessary longer or longer. Often a sick leave is first given for the next two to three weeks. Gradually the patient becomes more flexible again and can go back to his job and leisure activities.
Benefits of surgery
A herniated disc can meanwhile minimally invasive and outpatient surgery, sometimes only under local anesthesia. If the indications for surgical treatment of the herniated disc are met, appropriate treatment should be given promptly. The herniated disc operations have proven themselves and are very useful good results so that most of those affected benefit from it.
The minimally invasive procedure creates no major scarsso that wound healing disorders rarely occur. In addition, the modern surgical technique lateral access to the intervertebral disc, which offers the advantage that surrounding structures in the area of the spine such as ligaments and nerve tissue are only extremely rarely damaged.
The greatest advantage is the fact that operated patients are a lot compared to conservatively treated patients symptom relief faster Experienced. In summary, it can be said that if the indication for surgery is appropriate, those affected generally benefit from the procedure.
Disadvantages of an operation
The risks of an operation for a herniated disc are described in detail in the following section.
Besides the general risks of surgery and the associated anesthesia, there are special complications that can occur depending on the surgical procedure used. This includes the damage to structures in the vicinity of the surgical field, for example the Injury to nerves, blood vessels or internal organs. The anesthetic risks were reduced by the increasing use of minimally invasive procedures local anesthesia can be significantly reduced.
The most significant disadvantage for many patients is this uncertaintywhether the operation of the herniated disc really leads to an improvement in your symptoms. Since back pain is often not only caused by the herniated disc, but also by an incorrect strain on the muscles and lack of exercise, the operation does not always lead to complete freedom from pain. Here are special ones Exercises essential for strengthening the back muscles.
There at invasive Surgical procedure the The statics of the spine changed and the surrounding structures may be injured, pain can rarely be exacerbated by the operation. Minimally invasive procedures, however, often lead to an improvement in back pain. Recurrences herniated disc are possible despite surgery.
Another disadvantage is the fact that with the minimally invasive procedure, a slight X-ray exposure exists, since the position of the surgical instruments must be checked intraoperatively with X-ray images.
In summary, the better outcome of the operated patients be advised regarding freedom from complaints. In the case of absolute surgical indications such as bladder and rectal disorders or acute paralysis, surgery is the only possible therapy for the herniated disc.
Risks of a disc surgery
Thanks to medical advances, herniated discs are now a part of a minimally invasive surgery operated on.
In general, the risks of the operation are very low, but possible complications can never be completely ruled out. Intraoperatively, unexpected problems can occur, which lead to an acute deterioration of the patient's situation.
As with most surgeries, there is a general risk of complications like Secondary bleeding, Infections of the wound, Strength Pain and Swelling occur during and after the procedure.
After an operation there is also the risk for Thrombosis and Pulmonary embolism elevated.
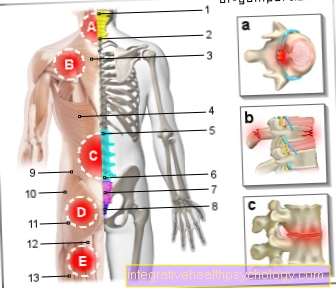
Disc operations in the lumbar spine can lead to special problems. These include, for example, injuries to vessels and nerve roots, to the peritoneum (peritoneum) or on the intestines, bladder and ureter injuries, and erectile dysfunction in men.
The risk of injury to internal organs exists especially during operations on the lower lumbar spine.
Similar operations on the cervical spine can damage blood vessels and nerves. Since there are important structures for voice formation in the neck area, in rare cases injuries to the responsible nerves can lead to a temporary hoarseness (Recurrent palsy).
In addition to these general risks, there are special complications that the attending physician should inform about before the procedure. Used as part of a Disc surgery If the intervertebral disc is replaced by an artificial disc, this prosthesis can cause problems (see also: Intervertebral disc prosthesis).
If the implant is not properly seated or if it grows incorrectly with the surrounding tissue, it can become increasingly loose or migrate. It can sink in and also detach from the bone, which in turn creates the risk of nerve compression.
This results in symptoms like tingle, Numbness or Functional failures different body structures. This depends on the height of the vertebral body to be operated on.
Furthermore, the loosening of the prosthesis can also restrict the patient's mobility in the spine.
In some cases, these complications can mean that another operation is necessary to remove the implant and replace it with a new one. The doctor must now weigh up whether another surgical technique is more suitable for the patient. Furthermore, the implants used can wear out after years and then no longer achieve the desired effect. In these cases, a new operation may also be indicated.
Operation of a herniated disc in the lumbar spine
A herniated disc in the lumbar spine is not uncommon. However, many patients can do without an operation, especially one herniated disc Lumbago (lumbago) It is not always possible to distinguish directly from the symptoms and therefore not to act too hastily.
During a MRI scan for a herniated disc It should be clarified whether there is a herniated disc and whether it is classified as dangerous. Before the indication for an operation is made, treatment should be conservative. This includes movement and strength training as well as occupational therapy so that the patient can adjust to the situation and learn which movements are beneficial and which can even be harmful.
A reinforced indication for the operation of a herniated disc on the lumbar spine, if the patient Symptoms of paralysis, tingling sensations, strong and worsening symptoms and Continence problems Has. These are signs that the intervertebral disc is pinching off the spinal cord or the emerging nerve root and that action must be taken quickly to prevent the symptoms from worsening.
The operation takes place under general anesthetic in most cases from the back; i.e. the patient lies on his stomach. An access is then prepared on the affected disc so that the surgeon can operate on the herniated disc.
Today this access can be via microsurgical procedures can be kept very small. In many places there is also an endoscopic, so minimally invasive variant offered. A tube is pushed up to the intervertebral disc and the surgeon works on the intervertebral disc with a camera and tiny instruments. Due to the small size of the interventions, most patients are already resilient after a few days and can go to rehab.
Read more about the topic here: Operation of a slipped disc of the lumbar spine
Operation of a herniated disc of the cervical spine
The operation of a herniated disc on the cervical spine should not be done recklessly. First should be with conservative therapy consisting of pain therapy, physiotherapy with movement and strength training as well as training for those affected in how to deal with the herniated disc (relief, incorrect movements, etc.).
Only after this approach has failed or if there are neurological deficits and worsening of the problem should an operation be performed. There are two main procedures, both of which are shown below general anesthetic occur. On the one hand the Operative access from anterior (from the front over the neck). An incision is made in the neck and the structures on the neck are prepared to the side in order to then access the herniated disc of the cervical spine from the front. On the other hand there is the possibility that Operation from the dorsal side to do (from the neck). An incision is also made here and then worked your way up to the corresponding intervertebral disc. Depending on the type and location of the herniated disc on the cervical spine, one of the two or a combination of the methods is used.
In the operating room, the affected intervertebral disc removed and then one Intervertebral disc prosthesis (artificial disc) or a Cage brought in. A cage is a kind of cage that connects the two adjacent vertebrae. Ideally, patients are symptom-free a few days after the operation. It is also essential to have a Rehab to think so that the patient can prevent further problems through good training and education and also fully participate in life again.
Pain after the intervertebral disc surgery
The occurrence of pain after surgery is not primarily a cause for concern, but rather normal to a certain extent. Every surgical procedure puts a heavy strain on the body. Depending on how long and how long the body has been positioned during the operation, pain is often caused muscular tension caused.
Pain in the area of the surgical scar are also harmless up to a certain point, as the skin and surrounding tissue were damaged by the cut and then have to regenerate again. Shortly after the operation, this area is irritated, sensitive and can therefore also be painful. However, pain in the area of the scar can also be caused by a Inflammation of the wound arise, which must be treated promptly.
The one relieved by the disc surgery Spinal nerve also needs a certain Regeneration timet. This explains why the pain caused by the herniated disc does not go away immediately after the operation, but rather subsides day by day.
Another cause of pain after a herniated disc surgery is that Scarring. The pain caused by this can appear immediately after the operation or it can only develop later. Scarred tissue forms in the nerve root area, which leads to Nerve irritation can lead. In this case, those affected often complain of pain radiating into the legs.
In addition to scar tissue, you can also Bleeding or Inflammation cause pain in the operated nerve root area. Here it is essential to take appropriate countermeasures quickly. Perhaps one occurs as a common surgical risk Material incompatibility which is associated with pain after the operation.
After excluding all other possible causes of pain, the Unsuccessful operation be considered. On the one hand, it is possible that, despite the surgical intervention, the underlying problem, the herniated disc, has not been resolved. On the other hand, nerves or surrounding structures may have been affected, which now causes the pain.
A final reason for pain after a herniated disc operation is the so-called "Post nucleotomy syndrome". This is one therapy-resistant and often chronic pain after a herniated disc operation. The reasons for this are variable and must be clarified individually. A burning and electrifying pain character can be indicative of the presence of such a syndrome. In addition, the pain is part of a post-discectomy syndrome movement dependent and often goes with additional Paresthesia like tingling and numbness.
Regardless of the cause of the pain after a herniated disc operation, a doctor must be consulted urgently in the event of long-term pain. A timely re-presentation is of therapeutic and prognostic relevance.
Rehabilitation after a herniated disc operation
A rehabilitation is after the surgery of the herniated disc enormous importance. The patient has to learn to adapt his movements and posture to the new situation. In rehab it is through Physiotherapy, muscle building, postural exercises and strain the muscles of the spine and the rest of the body are strengthened. In this way, the patient should recover quickly after the operation and future complaints should also be prevented.
Thanks to today's microsurgical interventions, rehab can often be done within the first week to be started after the operation. The duration and type of rehab depends on the condition and severity of the symptoms. The Duration the rehab can be between 3 and 8 weeks lie.
There is the possibility of one outpatient, partial inpatient or stationary Rehab. Depending on the cost unit, the costs for this are not fully covered and an own contribution must be expected.
Payers can the Health insurance, but also the Pension insurance be. In the case of patients who tend to be able to go back to work after rehabilitation, the pension fund often acts as the cost bearer, as the patient will continue to pay into the pension fund when they are able to work again. The patient submits the application for rehab together with his treating specialist or family doctor. In severe cases, the ward doctor can apply for follow-up treatment. This should bring the patient into the physical condition to live independently at home again and then go to the requested rehab. In addition to medical rehab, occupational rehab can also be relevant. In this, the patient is trained again at his workplace or retrained if he can no longer work in his original job.
Also read more on the topic Rehabilitation after a herniated disc
Cost of a disc surgery
The cost of an intervertebral disc operation can vary widely.
The costs are calculated based on the surgical technique performed and the prosthesis used. A distinction is made between the possible approaches invasive and minimally invasive Method.
Depending on which method was used, the costs can vary. Furthermore, the costs for a general anesthetic, i.e. the anesthesia, and for the drugs used during the operation.
Then there are costs for the length of the hospital stay. Such an operation is usually billed as a flat rate per case, which can vary from hospital to hospital due to the individual patient case.
About up 3000 to 5000 € the cost can be estimated.
Furthermore, the assumption of costs depends on the insurance company with which the patient is registered. It is possible that in some cases the patient will have to pay the remaining amount himself.
To this end, he can, on the one hand, seek detailed information in a preliminary discussion with the treating doctor, and on the other hand, such interventions should also be discussed with the health insurance company in advance. This can avoid any unexpected invoices.
Appointment with a back specialist?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The spine is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
The treatment of the spine (e.g. herniated disc, facet syndrome, foramen stenosis, etc.) therefore requires a lot of experience.
I focus on a wide variety of diseases of the spine.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
What can you do conservatively with a herniated disc?
We have summarized everything you can do with a herniated disc without surgery on a completely separate page.
It is important that each herniated disc is viewed individually and that each person affected has something different to do.
Read more about this under our topic: Herniated disc - what to do?