psychosis
Definition - what is a psychosis?
A psychosis is a mental disorder. Patients suffering from a psychosis have an altered perception and / or processing of reality. While outsiders clearly perceive this perception as abnormal, those affected themselves are not aware of their misperception. Psychosis can be accompanied by various symptoms. These include hallucinations, delusions and pronounced thought disorders.
Psychoses can occur as a single episode. However, a recurring course can also occur. How a psychosis progresses depends, among other things, on the triggering cause. Acute psychosis should be treated with medication as soon as necessary.

causes
With regard to the possible triggering causes, psychoses are divided into two broad groups: the organic psychoses and the non-organic psychoses.
Organic psychosis can be triggered by various somatic (physical) diseases.These include, for example, diseases of the brain such as dementia, epilepsy and Parkinson's disease or masses in the area of the brain (tumors). In rare cases, brain injury can also lead to psychotic episodes. Certain autoimmune diseases can also trigger psychoses. Examples of this are multiple sclerosis (MS) or lupus erythematosus.
One of the most common causes of organic psychosis, however, is the consumption of drugs, which is referred to as substance- or drug-induced psychosis. Substance-induced psychosis can be triggered by a wide variety of drugs.
Read more about this under Drug psychosis
In addition to the organic psychoses, there is the large group of non-organic psychoses. These include psychoses that occur as part of an underlying mental illness. Schizophrenia is the most common mental illness associated with psychosis. But psychotic episodes can also occur in the context of mood disorders, i.e. depression or bipolar disorders. However, a direct trigger cannot be found for every acute psychotic episode.
Read about this too
- Symptoms of schizophrenia
- Symptoms of depression
What role does vitamin D play?
Some studies deal with the question of what effects a deficiency in certain vitamins has on mental function. Some studies have suggested that there may be a link between a vitamin deficiency and mental disorders such as psychosis. The subjects of these studies included vitamins D, B12 and folic acid. One study indicated that there is an above-average rate of vitamin D deficiency in patients with psychotic disorders. So far, however, there is no proven connection that a deficiency in vitamin D can be a trigger for a psychotic episode. In the coming years, further studies on the subject may be able to uncover more details.
Concomitant symptoms
Psychosis is accompanied by numerous symptoms that are usually very frightening for the patient. Acoustic hallucinations are common. For example, those affected hear voices talking about them or communicating with them. There are also imperative voices that give orders to those affected. Smell and taste hallucinations or tactile (touch) hallucinations are less common.
Delusions also very often occur in the context of a psychosis. For example, the sick person feels persecuted, threatened, bugged or observed. A so-called relationship delusion, in which the person concerned incorrectly refers to things happening in their environment, is also relatively common. An example of this is news on the radio that the psychotic patient suddenly refers to - he thinks he is being talked about here.
So-called ego disorders often occur in the context of a psychosis. Those affected feel alienated from themselves, have the impression that others can withdraw their thoughts or read / hear them. Thought disorders are also a typical symptom of psychosis. These are perceived by outsiders as confusion or severe concentration problems. The thinking of those affected appears to outsiders to be completely incoherent, disheveled and without internal logic. This is also evident in the language. It can happen that sentences are broken off in the middle. It is seemingly completely incoherently jumped from one topic to the next and the content of what is said is no longer comprehensible for outsiders.
Additional possible symptoms are - depending on the underlying disease - pronounced concentration disorders, reduced performance and severe memory disorders. Especially with psychoses that occur in the context of schizophrenia, there are also so-called negative symptoms with concentration disorders, thought disorders, social withdrawal, low affect and joylessness as well as reduced drive.
The symptoms of psychosis are extremely stressful and frightening for both the person affected and the relatives.
Also read the article: What is the difference between schizophrenia and psychosis?
Obsessive thoughts
Obsessive-compulsive thoughts are not a typical symptom of psychosis. Rather, they occur in the context of so-called obsessive-compulsive disorder. People with obsessive-compulsive disorder often experience obsessive-compulsive thoughts. These are thoughts that those affected actually do not want to think, but which repeatedly force themselves on them without them being able to do anything about it. Obsessive-compulsive thoughts are often of a violent nature and are very distressing for those affected. However, in contrast to psychotic patients, patients with obsessive-compulsive disorder have a preserved sense of reality.
Please also read our main page Obsessive-compulsive disorder
diagnosis
The diagnosis of psychosis does not initially require any medical apparatus, but is a purely clinical diagnosis and is made on the basis of the patient's behavior and symptoms. Once the diagnosis has been made, however, further diagnostics must be carried out in order to narrow down the possible causes of the psychosis.
In order to rule out the presence of an organic psychosis, it is first important to take a precise anamnesis. Since those affected can hardly have an adequate conversation even during a psychosis, the attending physician is often dependent on third-party anamnesis, i.e. asking close relatives / acquaintances / friends. When taking anamnesis, the question of previous illnesses, both somatic and psychological, is important. It is also very important to find out whether a psychotic episode has occurred before. Furthermore, possible drug use should be carefully questioned. The question of medication you take regularly is also important.
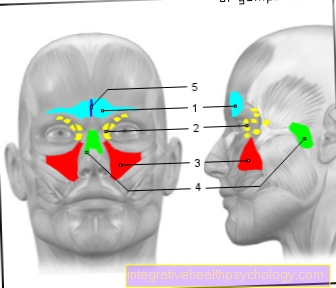
The anamnesis is followed by a blood sample. Here, too, physical illnesses can show up, which can be a possible trigger for the psychosis. In many cases it also makes sense to take an image of the head in order to be able to rule out space-consuming processes in the brain or, for example, diseases such as multiple sclerosis. For older patients - depending on the question - the faster available computed tomography (CT) can be used here, with the help of which, for example, spatial claims can be excluded relatively reliably. However, magnetic resonance imaging (MRI) is more likely to be performed for younger patients and with special questions. An electroencephalogram (EEG), i.e. an examination of the brain waves, may also be necessary. Which further examinations are necessary depends on the ongoing examination results.
Read about this too
- Electroencephalography
- CT of the head
- MRI of the head
Treatment / therapy
In the case of psychosis, it is important to start treatment quickly. Depending on the severity of the psychosis, treatment can be either outpatient or inpatient. Often, however, due to the severity of the symptoms, which endanger the patient's self, inpatient treatment is recommended.
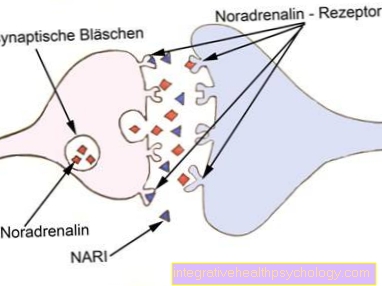
Medicines, the so-called antipsychotics or neuroleptics, are considered the first choice for treating psychoses. The group of these drugs includes numerous different active ingredients which, however, almost all intervene to a greater or lesser extent in the dopamine metabolism in the brain and thereby lead, above all, to the rapid containment of delusions and hallucinations. In most cases, antipsychotics should initially continue to be taken even after the symptoms have subsided, as they significantly reduce the likelihood of the psychosis recurring. How long the medication should be taken must be decided on an individual basis. Especially with psychoses recurrent A (recurring) course such as schizophrenia, it is often necessary to take the medication for a long time.
A distinction is made between typical and atypical antipsychotics. Nowadays, atypical antipsychotics such as risperidone, quetiapine, clozapine, olanzapine and aripiprazole are increasingly used. Typical antipsychotics like haloperidol are nowadays mainly used in the acute phase. Which antipsychotic to use, however, must be decided individually. Psychotherapeutic procedures only play a subordinate role in the acute phase of the psychosis, but they can help in the course. Patients who have been through psychosis can also take part in psychoeducational groups. Here they are informed about the topic of psychosis and how to deal with it and come together with like-minded people. In the case of organic psychoses, the treatment of the causative illness comes first.
Zyprexa
Zyprexa is a drug belonging to the group of antipsychotics. It contains the active ingredient olanzapine and is one of the atypical neuroleptics. It is mainly used to treat psychoses that occur in the context of paranoid schizophrenia. It is also used to treat bipolar disorder. In addition, olanzapine can be used as a second drug in depression for so-called augmentation therapy. The theory here is that the increase in a second drug, here olanzapine, has an additional mood-enhancing effect.
The most common and common side effects of olanzapine are weight gain, tiredness, dry mouth, dizziness, nausea / vomiting, constipation, insomnia and restlessness, increased blood counts, edema (water retention), unusual movements (Dyskinesias), Rash, joint pain, and sexual dysfunction.
Duration
The duration of a psychosis is very different and depends, among other things, on the triggering cause. In addition, the time at which treatment is started plays an important role. The faster a drug therapy is initiated, the better a psychosis can be contained. Psychoses can last a few days, but if left untreated, they can last several months or longer.
You might also be interested in: Can schizophrenia be cured?
forecast
Patients who experience psychosis for the first time in their life have a relatively good chance that such an episode will not recur. The course / prognosis depends largely on the cause.
If it is a drug-induced psychosis and has appeared for the first time, consequent avoidance of drugs can lead to full recovery. Repeated drug use in patients who have suffered drug-induced psychosis significantly increases the risk of recurrence of psychotic episodes.
In patients who had an initial psychosis as part of schizophrenia, the chance that the disease will heal without consequences is about 1/3. In the second third of the patients, there is a course in which phases of symptomlessness alternate with psychotic phases. About a third of the patients develop a chronic course with permanent symptoms. In chronic forms, in addition to the symptoms of psychosis, there are also cognitive disorders as well as disorders of concentration, feelings and drive. In severe cases, this can make early retirement necessary.
Differentiation of the clinical picture
What is drug psychosis
A drug psychosis is referred to in technical jargon as drug-induced or substance-induced psychosis. It is a psychotic episode triggered by the use of one or more psychotropic substances. Examples of possible psychogenic substances are alcohol, cannabis, amphetamines, cocaine, LSD or crystal meth (metamphetamines).
There are people who are more vulnerable (more vulnerable) are more likely to develop psychosis than others. In these people in particular, drug use can trigger psychosis. Drug psychosis is treated with drugs in the same way as other types of psychosis. However, complete abstinence is also essential in the treatment of such psychoses. In many cases, this can prevent the psychosis from recurring, but not always. The symptoms of drug psychosis are similar to those of other forms of psychosis. Hallucinations, delusions, anxiety, thought disorders, ego disorders and concentration disorders occur.
Also read our article Drug psychosis
What is the difference between psychosis and schizophrenia?
Psychosis is a term that is actually no longer used in this form today. In psychiatric jargon, it is more of a psychotic disorder or a psychotic episode. A psychosis describes a state in which the person concerned perceives reality inadequately. He suffers from hallucinations and delusions and can no longer distinguish the real from the unreal. Such a psychosis can - as already described above - have numerous possible causes.
Schizophrenia, in turn, is one of the possible causes of psychosis. Schizophrenia is a mental illness whose main symptoms are psychotic disorder and all of its symptoms. Patients with an acute psychotic flare-up of schizophrenia thus suffer from delusions and hallucinations. Thought disorders and ego disorders are also typical. In addition, there are often so-called negative symptoms in schizophrenia. These include symptoms such as reduced affect, reduced drive, loss of social contacts and apathy. The third pillar of symptoms in schizophrenia are cognitive disorders. Distinct concentration and memory disorders are common. Psychosis is more likely to be seen as a symptom (which consists of other symptoms) that can have various causes, while schizophrenia is a serious mental illness that is very often associated with psychotic symptoms.
Read more about this on the main page Schizophrenia or What is Schizophrenic Psychosis?
How is it related to Obsessive Compulsive Disorder?
A psychotic disorder has basically nothing in common with an obsessive-compulsive disorder. These two diseases are two different entities of mental disorders. Obsessive-compulsive disorder is associated with compulsions and obsessions. The obsessive thoughts unintentionally force themselves on the person concerned and have to be thought over and over again. In contrast to psychosis, however, the person affected knows the actual nonsense of these thoughts, the reference to reality is preserved. Nonetheless, obsessive-compulsive disorder is an extremely distressing condition that often requires treatment.
What is the difference between a psychosis and a neurosis?
The term neurosis does not really exist in psychiatric medicine in this sense any more. This used to describe a general psychological behavior disorder that could be accompanied by a wide variety of symptoms. The person concerned cannot control these behavior disorders sufficiently, but is aware of them. The relation to reality remains unchanged. In the case of psychosis, on the other hand, the person affected has lost touch with reality and can no longer distinguish between delusional content and reality. Psychosis and neurosis are thus two different mental disorders.
When can I be admitted to a psychosis?
In the technical jargon, compulsory admission is referred to as accommodation according to the Mentally Ill Act, often also referred to as PsychKG. In Germany, as a rule, a person cannot be brought into a facility or detained there against his or her will, as this is considered a deprivation of liberty. Therefore, to accommodate a person according to PsychKG, there must be serious reasons, which are listed in the legal text:
- The person concerned must be mentally ill.
- There must be a significant risk to the person from himself or
- There must be a significant risk to the legal interests of others from the person.
In the psychiatric area, for the sake of simplicity, it is usually referred to as being at risk for oneself or others.
Patients with an acute psychotic disorder may be able to show the reasons mentioned for admission according to PsychKG. On the one hand, there is a mental illness; on the other hand, the psychosis may endanger yourself or others. Examples of this would be the following: The sick person hears voices telling them to jump out of the window. Here there is an acute suicidality and therefore a risk to oneself. Another scenario is that the person concerned hears voices giving orders that the person concerned do serious violence to other people.These are only exemplary examples to explain in which situations placement (compulsory admission) can be necessary and justified.
In order to enforce such a placement, the public order office or the fire brigade must be called - depending on the state and time of day. Furthermore, a medical certificate must be drawn up that explains the reasons for the planned placement. This must be served on the local court. A judicial hearing must then take place within 24 hours. Until then, the sick person may be placed in a psychiatric facility against their will. Forced medication is also possible within this time, if absolutely necessary, as is the use of restraint measures. After these 24 hours, a judge must decide whether further placement of the patient is legal or whether the placement measures must be ended.