Spinal anesthesia
General
This form of anesthesia is the introduction of an anesthetic (substance that makes the region in question numb) into the area between the spinal bones and the spinal cord. the so-called liquor space or spinal canal.
This type of anesthesia is used when performing a major procedure and when performing operations where local anesthesia is insufficient or not possible.
Examples of this can be: Operations in the hip area, in the groin region, in the lower abdomen (for example, the caesarean section) and patients with lung problems to bypass the anesthesia.
Spinal anesthesia must not be performed in the case of diseases of the spinal cord, severe spinal deformities, inflammation in the area of the spine or the surrounding tissue, allergies to the anesthetic, in uncooperative patients or in the absence of the patient's declaration of consent for this type of intervention.
You might also be interested in this topic: Conduction anesthesia

anatomy
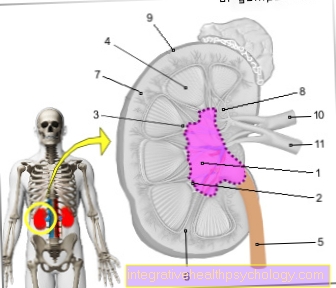
The spinal cord is bony surrounded by the spine. The spine itself consists of 24 individual bones. A single vertebral bone consists of the vertebral body, the spinous processes and the vertebral arches, which together with the vertebral body form a round opening through which the spinal cord runs.
The spinal cord is surrounded by multiple meninges.
As the first skin that you feel like a kind Envelopment of the spinal cord can imagine, the soft meninges also come Pia mater called. Followed by the Spider skin ( = Arachnoid) and as the outermost skin, which in turn rests on the inside of the arched, round opening of the vertebral bone, the hard meninges, also Dura mater called.
Between the soft meninges and the spider skin there is a liquid filled cavitythat one CSF or also Subarachnoid space is called.
In this Space circulates the brain water or CSF fluid. The anesthetic is used in this area Injected numbing of the nerves and thus acts directly on the spinal cord and its adjacent spinal nerves.
The limited suppression of all feelings in a certain area, without having to burden the entire organism with general anesthesia.
Preparation / implementation
In front any spinal anesthesia becomes the patient of a Anesthetist enlightened. This explains to the patient in advance what exactly happens during such an intervention, clarifies possible complications and asks about important aspects such as Intolerance to medication, Allergies, Taking medication and serious diseases that stand in the way of spinal cord anesthesia.
Shortly before the actual intervention, the Spinal anesthesia carried out.
In a sitting and bent forward position or in lying and bent posture the anesthetic is introduced.
To Avoiding infection the skin area is disinfected and the surrounding area of the patient is covered in a sterile manner.
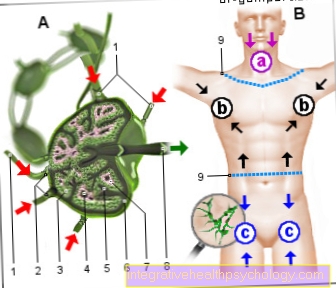
The area is approximately open for the puncture Height of the 3rd to 4th lumbar vertebrae (LWK) or 4th and 5th LWK prefers.
The spot can be found by walking with both hands slightly below the waist to the back summarizes. At the level of the spine is roughly the right place for the spinal cord puncture.
The area in the lower loin above the buttocks is due to the anatomical peculiarity the vertebral bone is particularly well suited to get into the spinal space relatively easily.
One makes use of the fact that the spinous processes in this area while the patient makes a cat hump diverge well can.
after the correct position of the patient taken, sterile conditions and the puncture site has been located, you go with a long wafer-thin needle through the skin, between the spinous processes in the spinal canal.
This spinal needle is hollow inside. After the puncture, the first thing to do is to check the correct fit of the needle. This can be confirmed by a few drops of clear liquid (the liquor) from the back opening of the needle. The anesthetic is now introduced.
There is also the Possibility to bring the drug or a thin catheter into the Subarachnoid space along the needle to allow permanent drug delivery.
This catheter usually comes with prolonged surgical interventions for use or can also be used for pain therapy after the operation.
Duration of action
The anesthesia procedures close to the spinal cord include on the one hand spinal anesthesia and on the other hand epidural anesthesia (PDA). With both, a targeted elimination of pain and sensitivity in certain parts of the body is achieved.
However, a big difference between the procedures is their duration of action. While single doses are injected into the liquor space in spinal anesthesia, in epidural anesthesia a catheter is typically inserted in front of the skin of the spinal cord, through which painkillers or local anesthetics can be administered continuously or at intervals.
Read more on the topic:
- Lidocaine
- Xylocaine
- Procaine
The effect of the spinal anesthesia starts immediately after the administration of the local anesthetic and, depending on the pharmaceuticals administered, will last for about 1.5 to 6 hours. The PDA, on the other hand, only gradually develops its effect after about 15 minutes, due to the position of the catheter outside the CSF space. With good care, however, the catheter can advantageously be left in its position for a period of a few days, so that pain can be eliminated by re-injections with the PDA over a longer period of time.
indication

The spinal cord puncture is a frequently used measure in anesthesia to monitor pain during surgery.
The advantage over general anesthesia is that the patient is awake and responsive and only no longer feels any pain in the area concerned.
Spinal anesthesia is gentler on the cardiovascular system and offers the opportunity to treat people with serious secondary diseases.
These secondary diseases can be, for example: a weakened heart or severe lung diseases such as chronic obstructive pulmonary disease (COPD for short).
The procedure is easy to carry out, a complete elimination of pain is achieved and the rapid onset of action is an advantage.
This procedure is most commonly used for surgical interventions in the lower abdomen.
This area includes gynecological operations (e.g. removal of the uterus), urological interventions such as kidney operations and also operations in the area of the groin and the lower extremity, that is, for example with artificial hip and knee replacements but also with hernias mostly the method of choice.
In obstetrics, spinal anesthesia is preferred to respiratory anesthesia. Because the expectant mother is conscious, complications such as the risk of aspiration (swallowing) can be avoided. Another side effect is of course that a short contact between mother and newborn is made possible.
Spinal anesthesia has the advantage over general anesthesia that substances that can trigger hyperthermia in the body do not have to be used.
Other consequences such as the risk of thrombosis, embolism, allergies to hypnotics (drugs used during anesthesia) or immobility can be minimized. All in all, this has a positive effect on the condition of the patient, who can get back on their feet more quickly after the operation, usually just by choosing the anesthetic method.
Another advantage of spinal anesthesia is the good control of the field, which can numb different areas depending on the height of the spine.
From this it follows that only individual extremities can be anesthetized without, for example, including the area of the abdomen.
Conversely, only the lower abdomen can be anesthetized, so that feeling and mobility in the legs are retained. This effect is particularly positive for the later mobilization of the operated person.
Complications
Depending on the level of anesthesia Occasionally there may be discomfort after the operation or rarely during the operation.
Medication can lead to a Decrease in the activity of the cardiovascular system come, in this context there may be a reduction in the Blood pressure and des Heartbeat come.
Remedy this situation Medicines to stabilize and strengthen the circulation and fluids, which help to stabilize the circulation.
With a Spinal anesthesia at lung level it can lead to a corresponding reduction in respiratory function, which in turn leads to a decreased depth of breath with inadequate oxygen uptake as well Carbon dioxide release goes hand in hand.
Here can through Giving oxygen through a nasogastric tube be helped with further bad breathing situation ventilation must be considered.
Rarely develops through the Puncture of the spinal canal a negative pressure that a headache can trigger.
It helps here flat lying position take in order to reduce the tension on the puncture site and the meninges as such, possible ingestion pain reliever medication and copious intake of fluids can improve the symptoms.
If the spinal cord is injured during the Puncture of the spinal canal it can lead to failures that are associated with numbness or muscle paralysis.
These symptoms can declining and self-limiting be.
If a hematoma forms in the spinal canal, it must be surgically removed. This Complications are very rare.
Side effects and risks
As with all medical procedures, spinal anesthesia can lead to complications and side effects. The application of the spinal or epidural anesthesia can unexpectedly fail and thus possibly lead to pain or not work properly.
In addition, due to the deactivation of the corresponding nerves, the vessels in the lower half of the body widen, which can lead to a significant drop in blood pressure. This situation can be remedied by medication that stabilizes and strengthens the circulation, as well as the administration of fluids, which help to stabilize the circulation.
Read more on the topic: Medicines for low blood pressure
A spinal cord anesthesia at the level of the lungs can lead to a corresponding reduction in respiratory function, which in turn is associated with a reduced breathing depth with insufficient oxygen uptake and carbon dioxide emission. This can be helped by administering oxygen via a nasogastric tube; if the breathing situation continues to be poor, ventilation must be considered.
A typical side effect is the so-called post-spinal headache, which, depending on the procedure, can affect more or fewer patients a few days after the procedure. Here it helps to take a flat lying position to reduce the tension on the puncture site and the meninges as such, possible use of pain reliever medication and plenty of fluids can improve the symptoms.
A risk feared by many patients - spinal cord injury - occurs extremely rarely. Injury to the spinal cord during the puncture of the spinal canal can lead to failures associated with numbness or muscle paralysis, these symptoms can be regressive and self-limiting. Infections or bruises at the puncture site are also rare, as are the systemic effects of the local anesthetic, i.e. those affecting the whole body. If a hematoma forms in the spinal canal, it must be surgically removed.
Read more on the topic: Complications in anesthesia
Ultimately, however, when considering all possible risks, it must be noted that through continuous monitoring by the anesthetist and thorough care of the puncture site, most side effects can be quickly identified and treated, or even prevented from the outset. This makes spinal anesthesia a very safe and beneficial anesthetic method overall.
Headache after spinal anesthesia
Unfortunately, one of the typical side effects of spinal anesthesia is the so-called post-spinal or post-puncture headache. The unpleasant complication is presumably caused by a loss of brain water (Liquor) caused by a leak in the skin of the spinal cord that arose during the spinal cord anesthesia.
Since not as much liquor can be reproduced as is lost, there is negative pressure in the liquor space in which our brain and spinal cord swim. This results in the typical headaches, which improve when lying down and intensify when you are upright. Bed rest and adequate hydration are recommended for the treatment of postspinal headache. The symptoms usually improve within a few days.
If this is not the case, it can be assumed that the leak has not closed by itself. In this case, a so-called blood patch made from a few milliliters of autologous blood can be inserted into the puncture site. The blood that clots here closes the liquor leak so that the headache will soon subside.
How painful is spinal anesthesia?
How painful the application of anesthesia close to the spinal cord will be depends to a large extent on the experience of the anesthetist performing the procedure. In addition, the patient's anatomy plays a major role. This can lead to unpredictable difficulties that complicate the procedure and make it more painful. In most cases, however, patients find spinal anesthesia surprisingly less painful. This is thanks to a local anesthetic performed before the actual puncture, which numbs the skin and its underlying layers. The prick of the actual puncture needle is only felt as a dull pressure.
Read more on the topic: Local anesthesia - the local anesthetic
Can you give birth under spinal anesthesia?
Nowadays, spinal cord anesthesia are used in a large number of operations and interventions in a wide variety of specialist areas - including in obstetrics. In the meantime, spinal anesthesia has actually established itself as a standard procedure for caesarean sections, as it can avoid complications of general anesthesia for the child and mother. The epidural anesthesia is also used to eliminate pain in obstetrics - but here primarily to enable painless vaginal delivery. However, it should be borne in mind that the duration of birth under epidural anesthesia is significantly longer. In addition, the epidural anesthesia needs some time to develop its effect and is more time-consuming in the system, which is why spinal anesthesia is usually used for urgent deliveries.
Read more on the topic: Epidural anesthesia at birth