Spinal nerves
Synonyms
Medical: Nervi spinales
Spinal nerves, CNS, spinal cord, brain, nerve cell
English: spinal cord
Explanation
Humans have 31 pairs of spinal nerves (spinal cord nerves) that pass through the intervertebral holes between the individual vertebrae, namely (almost) analogous to the division of the spinal cord on each side:
- 8 cervical nerves, (nervi cervicales)
- 12 thoracic nerves (Nervi thoracales)
- 5 lumbar nerves (lumbar nerves)
- 5 sacral nerves (Nervi sacrales) and
- 1 coccyx nerve.
This even structure can give the impression of segmentation, which is why one often speaks of "spinal cord segments".

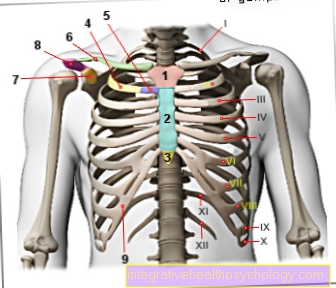
Figure spinal nerves
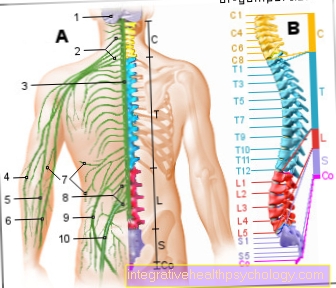
Spinal nerves
= Spinal nerves = segmental nerves
- Cerebrum + cerebellum -
Telencephalon + cerebellum - Arm nerve plexus -
Brachial plexus - Spinal cord - Medulla spinalis
- Spoke nerve - Radial nerve
- Median arm nerve -
Median nerve - Ellen's nerve - Ulnar nerve
- Cutaneous nerves -
Cutaneous nerve - Lumbar cruciate ligament braid -
Lumbosacral plexus - Femoral nerve -
Femoral nerve - Sciatic nerve -
Sciatic nerve
Segment nerves:
C1 - C8 - 8 cervical nerves (yellow) -
Nervi cervicales
T1 - T12 - 12 chest nerves (blue) -
Nervi thoracici
L1 - L5 - 5 lumbar nerves (red) -
Lumbar nerves
S1 - S5 - 5 sacral nerves (purple) -
Nervi sacrales
Co - 1 coccyx nerve (magenta) -
Coccyge nerve
Spinal segments (black)
and spinal cord segments (colorful):
C - neck area (cervical)
T - chest area (thoracic)
L - lumbar region (lumbar)
S - sacrum area (sacral)
Co - coccyx area (coccygeal)
You can find an overview of all Dr-Gumpert images at: medical illustrations
The spinal nerves
This term "spinal cord segments" has a purely practical meaning; it is used, among other things, to describe a certain level of the spinal cord; for example, the navel is located "at the level of Th 10", which means something like at the level between the 10th and 11th thoracic vertebrae (Th for thoracic segment).
Generally lies
- the 1st chest segment the 7th cervical vertebrae,
- the 1st lumbar segment the 10th thoracic vertebrae,
- the 1st sacrum segment opposite the 1st lumbar vertebra.
Humans have between 31 and 33 spinal nerves. Although it has only seven cervical vertebrae, eight pairs of spinal nerve roots, also known as cervical roots (cervix = neck), extend from the cervical cord:
This is explained by the fact that the spinal root belonging to the first cervical segment, abbreviated to C 1, leaves the spinal cord between the bony skull and the first cervical vertebra (atlas).
In the area of the cervical spine, the spinal roots are named after the vertebra below them.
The root belonging to the eighth segment of the cervical spine leaves the spinal cord between the seventh cervical vertebra and the first thoracic vertebra.
Therefore, from here on, all other spinal roots leaving the spinal cord are named after the vertebra above them (for example, root L 4 leaves the spinal cord between the fourth and fifth lumbar vertebrae), and the number of segments of the spinal cord corresponds to the number of vertebrae.
From the thoracic spine onwards, the number of spinal nerves corresponds to that of the vertebral bodies; accordingly twelve in the thoracic spine, five in the lumbar spine and further caudally (below) in the sacrum area another five spinal nerves. In the lowest area of the spine, on the coccyx, another one to three spinal nerves emerge variably.
Knowledge of this is important for the doctor in order to be able to better locate disease processes in the spinal cord based on clinical symptoms:
For example, an intervertebral disc that presses on the L4 root causes a very specific pattern of failures (clinical symptoms), a so-called root syndrome.
If the doctor sees this pattern, he can deduce that it must be the intervertebral disc between the fourth and fifth lumbar vertebrae.
A segment therefore corresponds to a certain section of the spinal column that supplies the fibers for a certain spinal nerve (a certain spinal root), even if this spinal nerve is later divided into individual nerves - although these parts do not necessarily have to be close together.
You can find more information about this under our topic: Spinal Cord
Structure, function and tasks
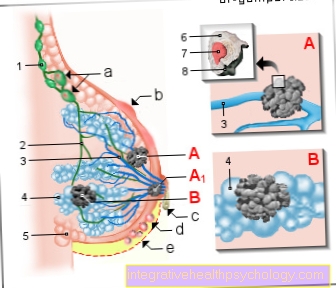
Spinal cord nerves are also known as spinal nerves in technical terms. They are not part of the central, but rather the peripheral nervous system and arise from the union of the anterior and posterior roots of the spinal cord.
The spinal nerves are used to forward information from the spinal cord [coming from the central nervous system (CNS)] to organs, muscles and all other parts of the body, or they transport information from these areas of the body to the spinal cord, from where it is sent on to the CNS.
They can therefore be roughly divided into two groups: The nerves that carry information from the spinal cord to further peripheral are called efferent; They start from the anterior horn of the spinal cord and, for example, pass on the "order" for the movement of a muscle that has arisen in the central nervous system. Information on the regulation of organ functions, such as an increase or decrease in bowel activity or increased or decreased secretion of digestive juices, is also passed on via efferent nerves. The second type of fiber, which is carried by a spinal nerve, conducts information in the opposite direction, i.e. from the periphery towards the spinal cord, entering the posterior horn; they are called afferent. They are used, for example, to pass on sensitive perceptions such as touch, temperature, pain and sense of position in the direction of the central nervous system. Sensitive perceptions of organs, for example the stomach filling, are also directed to the center.
The nerve exits through the intervertebral hole and divides into different branches:
- in a front branch to supply the skin and muscles of the front of the body (ramus anterior / ventralis),
- in a rear branch to supply the skin and muscles of the back of the body (ramus posterior / dorsalis),
- into a "connecting" branch (ramus communicans) that carries vegetative information and
- into a small, sensitive branch to supply the pain-sensitive membranes of the spinal cord (Ramus meningeus).
The spinal nerve itself, which is only about an inch long before it divides into several nerves, contains both the afferent and the efferent nerve parts and carries the four qualities described above, which are briefly summarized here: Somato-efferent (information that lead, for example, to muscle movement), somato-afferent (information about sensitive perceptions about the skin), viszero-efferent (information that influences organ activity) and viszero-afferent (information about the state of the organs).
The spinal nerve thus also contains nerve parts that regulate the autonomic (vegetative) nervous system - the sympathetic and the parasympathetic. Information is transported here that regulates, among other things, vegetative body functions such as sweat secretion, heart rate, bowel activity or pupil size.
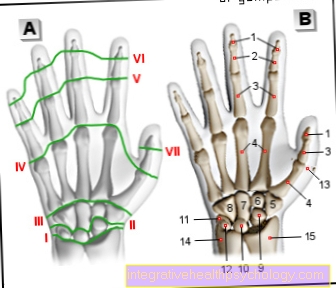
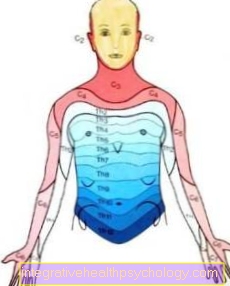
Basically, each pair of spinal nerves supplies a specific body segment with sensitivity. The innervation of the skin, especially on the trunk, is strip-shaped, these strips are called dermatomes. The pair of spinal nerves exiting under the fifth thoracic vertebra (Th 5) supplies a strip of skin that runs in the area of the nipples. The pair of spinal nerves that emerge below the tenth thoracic vertebra (Th 12) is responsible for the sensitive innervation of a strip of skin that includes the navel. The innervation of the dermatomes, however, is always overlapping, i.e. the dermatome Th 10 is also innervated by the spinal nerve segment Th 9 in the upper area and by the Th 11 segment in the lower area. This has the great advantage that if the spinal nerve segment Th 10 fails, there is no complete numbness in the affected dermatome.
It becomes more difficult in the area of the arms and legs: The segmental structure arose much earlier in the history of the development of vertebrates than humans and, strictly speaking, relates to the "quadruped" position. So it happens that a pair of spinal nerves that leave the spinal cord on each side of the body between the sixth and seventh cervical vertebrae, i.e. belongs to cervical segment 6 (abbreviated to C 6), supplies (innervates) the skin of the thumb, for example, and not the skin over the sixth cervical vertebra lies.
The supply of the muscles is a bit more complex than that of the skin: A muscle area supplied by a spinal nerve (myotome) does not have to be directly under the supplied skin area (dermatome), it can be somewhere else. In addition, a muscle is always supplied by the spinal nerves of several segments. If, for example, the spinal cord or an emerging spinal nerve root is damaged at a certain level, the entire muscle will not fail (be paralyzed) - the supply ensures that it is only weakened (= paretic). The reflexes are usually only weakened, not completely extinguished.
Some of the spinal nerves form so-called plexuses, i.e. nerve plexuses. Here several spinal nerves mix and move further peripherally. Therefore this strictly striped and segmental innervation for sensitive perceptions does not apply to all areas of the body; Such plexus formation occurs particularly on the arms and legs. The innervation of the muscles is also mostly not carried by a single spinal nerve segment. The individual segments have their so-called identification muscles (for example the biceps muscle - musculus biceps brachii - is primarily supplied by the spinal nerve segment C 5 and C 6 (fifth and sixth spinal nerves in the area of the cervical spine).
This property is used in the diagnosis and height localization of a herniated disc (prolapse), since a weakening (paresis) of the corresponding muscle provides a strong indication of the affected segment.
The most important plexuses are the brachial plexus, the arm nerve plexus, and the lumbosacral plexus for the lumbar and leg area.
Diseases

The most common form of impairment of spinal nerves is involvement in the sense of a root syndrome, which means that in the context of various diseases one (or more) nerve roots are affected in whatever way and then failures occur according to their own conduction qualities. In relation to a specific body section (corresponding to a segment), these are primarily:
- Pain
- Abnormal sensations such as tingling (= paresthesia)
- Sensory disturbances up to numbness
- Muscle weakness (paralysis) and weakened reflexes
There are many causes for irritation of a spinal nerve root (spinal cord nerve root), especially in connection with degenerative changes in the spine such as herniated disc or spinal stenosis, where a root is ultimately compressed and thereby irritated. The permanent irritation of a nerve root in the area of the spine can lead to an inflammation of the nerve roots, which manifests itself in the symptoms mentioned above.
This is usually the case in the lower segments (lumbar area) or in the neck segments. Diseases that affect a spinal root or a spinal nerve (spinal cord nerves) DIRECTLY, i.e. not in the sense of a compression syndrome, are more of an inflammatory nature and mostly caused by "neurotropic" (i.e. "nerve-loving") pathogens.
In addition, there is usually a participation of the peripheral nervous system in the sense of a radiculopathy / neuropathy (i.e. pathological occurrence without inflammation) in the case of poisoning (e.g. lead) or metabolic disorders (e.g. diabetes mellitus), but these usually do not cause any clear symptoms.
And finally there are nerve irritation syndromes that nobody knows the cause of (idiopathic).
A spinal nerve root (spinal cord root) can be irritated by:
1. Space-consuming processes such as a
- Herniated disc: the worn disc presses on the root
- Abscess: the settlement and local reproduction of bacteria that continue to grow in a "pus cavity" presses on the root
- Hematoma: Bleeding also takes up space
- Tumors: Tumors of the spinal cord itself or metastases from other tumors in the spine can press on the nerves
2. Inflammatory causes (radiculitis), a distinction is made here:
- Pathogen-related inflammation
- e.g. in the context of neuroborreliosis (borreliosis) caused by the bacterium Borrelia burgdorferi or
- Shingles (zoster), in which the varicella-zoster virus attacks the sensitive ganglion cells and spreads along the associated spinal (or facial) nerves and causes pain
- autoimmune inflammation
- e.g. Guillain-Barré syndrome with symmetrical paralysis rising from the legs (up to respiratory paralysis) with destruction of the isolating myelin sheaths due to the formation of antibodies directed against nerve components (autoantibodies).
For more information on Guillain-Barré Syndrome, see our topic: Guillain-Barré Syndrome
- e.g. Guillain-Barré syndrome with symmetrical paralysis rising from the legs (up to respiratory paralysis) with destruction of the isolating myelin sheaths due to the formation of antibodies directed against nerve components (autoantibodies).
Read more on the topic: Nerve root inflammation
inflammation
A direct inflammation of the spinal nerve (Spinal nerve) is no independently described Clinical picture, however, inflammation of a nerve root in the spinal cord area may occur. The spinal nerve arises from the union of both nerve roots, the anterior and posterior roots; lies a inflammation such Nerve root before, is also the appropriate one Spinal nerve affected. When a nerve root becomes inflamed, one speaks of one Radiculitis, if several nerve roots are affected, it is called polyradiculitis. Usually, the associated spinal nerve is also affected in the inflammatory process, so that in radiculitis, the inflammation of the roots, a neuritis, the Nerve inflammation, join.
Often is first yet not clear, what a process causes discomfort in the area of the nerve root, so one worded more generally from one Radiculopathy speaks; the cause does not have to be inflammation, but also degenerative processes on the spine, Compression syndromes, infectious Causes or a disc prolapse come into question.
Possible symptoms of inflammation of the nerve root are Pain and Sensory disturbances. It is always with Broadcasts to be counted in the area which is supplied by the corresponding root or the subsequent spinal nerve. Nerve root irritation in the area of the tenth thoracic spinal nerve can lead to discomfort in the area of the abdominal wall at the level of the navel. If the fifth lumbar spinal nerve is affected, this typically leads to pain or abnormal sensations that shoot into the leg and radiate into the big toe. Frequently take pain in the context of a root lesion Cough, sneeze or Press to.
Another symptom of radiculitis can be one Decrease in the function of the muscle which is supplied by the corresponding nerve root. For example, if the fifth cervical nerve root had a root lesion, the strength of the biceps muscle (biceps brachii muscle) could be weakened. A complete paralysis would however Not occur because the biceps muscle is also supplied by parts of the sixth cervical spinal nerve. Also Disorders of the reflexes and the Sweat secretion are in the affected segment or muscle possible symptoms a radiculitis.
Therapy is entirely dependent on the cause. At mechanical causes is an operational one Elimination the trigger a possibility. It is about infectious agents, is often one medicinal (especially antibiotic) therapy necessary. Radiculitis can cause such a disease, for example Borrelia burgdorferi be the tick-borne trigger of the Lyme disease.
Also known as "Shingles" designated disease caused by the Varicella zoster virus (VZV) is triggered. It only affects people who already have one in their lifetime Chickenpox infection because the virus that triggered it is the same as the lifelong in the so-called Spinal ganglia in the body lingers and in phases of a immunodeficiency the Herpes zoster can trigger. In most cases, the aforementioned spinal ganglion is primarily affected, and since the nerve root is in the immediate vicinity, the virus spreads through this to the periphery. Typical of herpes are zoster one-sided complaints, how Pain and Paresthesia in the affected spinal nerve segment, as well as a one-sided one that is also strictly limited to this area Blistering. Sensitivity disorders in the affected segment are also not uncommon. However, if the immune system is overwhelmed, as it is under a HIV infection may be the case, the virus is only limited in check so that it can spread multiple segments and up both halves of the body can spread.
Symptoms of a lesion
Is there a Lesion one Spinal nerves or one of the both lying just in front of this nerve Nerve roots before it can cause symptoms that one Reference to the place the lesion can give. It is primarily characteristic that only when infected of a spinal nerve the complaints on one specific body area are limited, as each spinal nerve supplies a specific segment. This is particularly easy to assign to the fuselage, as the segments here are called so-called stripes Dermatomes are arranged. In the field of extremities there is a mixing of the various spinal nerve fibers in Nerve plexuses (plexus)so that the assignment to a segment is no longer that simple, but follows clear rules.
Typical symptoms of a spinal nerve or nerve root lesion can be Pain, discomfort (Paresthesia), Sensory disorders, disorders of muscle function or Disturbances in the secretion of sweat be in the area that the affected spinal nerve supplies. For example, if there is a Shingles (Herpes zoster), which is located in the area of the nerve root that supports the tenth thoracic spinal nerve (Th 10) passes over, the patient could be over shooting Pain, discomfort and possibly also sensitivity disorders on the belly at the level of the navel complain that a few days later one could typically be strictly limited to one side and at the level of the navel vesicular rash demonstrate.