Reactive arthritis
Synonyms
Reiter syndrome
Engl. = reactive arthritis
definition
The reactive arthritis is one of the rheumatological clinical pictures (rheumatism) and falls under the category of Spondyloarthropathies. Specifically, one understands by one reactive arthritis a inflammatory disease of the joints with sterile synovial fluidwhich after a bacterial gastrointestinal or urogenital infection occurs.
Gastrointestinal infections affect the stomach or intestines, urogenital kidneys or urinary tract.
Sterile or aseptic synovial fluid means that no pathogens are found in the joint. In reactive arthritis, however, the detection of certain pathogen parts, mostly nucleic acids (DNA or RNA), is sometimes possible.
frequency
A reactive arthritis develop after certain gastrointestinal or urogenital infections caused by bacteria two to three percent Of the patients. The incidence of reactive arthritis is 30 to 40 per 100,000 inhabitants.
A gender cluster does not exist Men and women are the same often affected by reactive arthritis, however, there is a higher incidence of the disease in younger people.
causes
The cause of reactive arthritis is one genetic predisposition; an increased susceptibility to this disease is thus established in the genes. This can be seen from the evidence of certain factors in the blood of the sick. These factors are HLA-B27, the human leukocyte antigen type B 27. These antigens are MHC class I proteins, which are on the surface of almost all cells and play an important role in immune system play of the body.
In addition, when reactive arthritis develops, there is a triggering infection that manifests itself either in the urinary tract or in the gastrointestinal tract.
Count on the urinary tract Gonorrhea such as non-gonorrheic urethritis to. Gonorrhea develops after one Gonococcal infection, one non-gonorrhic urethritis is through Chlamydia and Mycoplasma (Ureaplasma urealyticum) caused.
Gastrointestinal infectionsAfter which reactive arthritis may occur include, among others Infections with Yersinia, Salmonella, Shigella or Campylobacter jejuni.
Some of these bacterial infections persist in the body and cause reactive arthritis if they are genetically predisposed.
The exact relationship between infection and reactive arthritis is not clear, but it does exist two guesses in this regard. The first hypothesis is that if you develop reactive arthritis, there will be a Cross reactivity between bacterial components and these similar human cell structures. This means that the immune system has been sensitized to the pathogen components after the bacterial infection and subsequently confuses human cell components - which are structurally similar to these - with the bacterial ones. As a result, an immune reaction directed against these human structures is triggered, which in turn manifests itself as reactive arthritis.
A second hypothesis on the pathogenesis of reactive arthritis includes the theoretical consideration that pathogen components remain in synovial cells and thereby also trigger an immune reaction in the body, which manifests itself as reactive arthritis.
Symptoms
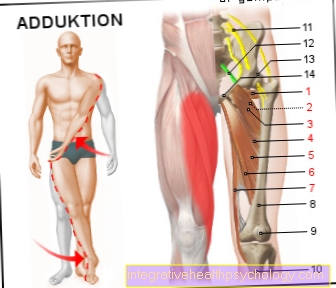
The clinical picture of reactive arthritis usually occurs two to six weeks after the infection on. The arthritis as Inflammation of the joints is mainly localized on the legs (Knee, ankle joints), less often to the Finger and toe joints. In the majority of cases, reactive arthritis presents an asymmetrical picture, which means that the same joints on both sides are not affected in parallel, for example only one knee joint. Often only one joint is affected (Monarthritis).
The inflammation manifests itself in the form of Pain, swelling, Redness, overheat such as Restriction of mobility. Joint stiffness occurs mainly in the morning and is then called Morning stiffness designated.
Sometimes unspecific complaints can accompany the arthritis picture, for example fever, Exhaustion and general feeling of illness. Furthermore you can Inflammation of the tendon attachments or Tendon sheaths (Enthesopathy, tendovaginitis), Inflammation of the sacroiliac jointSIJ (sacroiliac joint) (Sacroiliitis) or also Involvement of internal organs (heart, kidney) are added.
30% of reactive arthritis sufferers have other symptoms, which taken together Reiter syndrome form. These include:
- Reactive arthritis
- Urethritis = Inflammation of the urethra
- Conjunctivitis / Iritis = Conjunctivitis / iris inflammation (am eye)
- Reiter dermatosis = Skin changes on the genital mucosa (Balanitis circinata), on the palms and soles of the feet (Keratoma blennorrhagicum) or all over the body (like psoriasis), Aphthous ulcers of the oral mucosa
If the first three symptoms exist, one speaks of a Reiter triad, if the dermatosis is added, this is called the Reiter tetrad.
diagnosis
Reactive arthritis is first diagnosed with the help of the anamnesis and the clinical symptoms. This is supplemented by the laboratory, which Inflammation values (CRP, BSG) and HLA-B27 includes. In addition, if reactive arthritis is suspected, the initial one can be tried Infection using PCR (Polymerase chain reaction), Culture (Cultivation of the pathogen) or serology (Antibody detection), although this has mostly healed at the time of diagnosis and a positive result can no longer be achieved.
Using imaging techniques (roentgen, CT, MRI, Ultrasonic) other causes can be excluded.
therapy
The Treatment of reactive arthritis includes on the one hand the Infection remediation with positive pathogen detection, on the other hand one symptomatic therapy. The pathogen control takes place depending on the type of bacteria antibiotic (Antibiotic therapy)
The symptomatic treatment of reactive arthritis is suspended physical therapy (for example cold therapy), Pain management (NSAIDs) and if the NSAIDs are insufficiently effective Immunosuppressants (Glucocorticoids , Sulfasalazine) together.
forecast
In 80% of the cases, the reactive arthritis heals after one year. The fewer symptoms there are, the more favorable the prognosis. Recurrences of reactive arthritis can occur after stress or renewed infections and affect 20 to 70% of the sick.