Rectal cancer
definition
Rectal cancer is the cancer of the rectum. Since it cannot be clearly distinguished from colon carcinoma, the cancer of the large intestine, in its development, the two clinical pictures are often summarized as colorectal carcinoma. Colorectal cancer is the 3rd most common cancer in men and the 2nd most common cancer in women. It occurs above all from the age of 50 and its development is associated with some lifestyle factors. The symptoms of the disease, such as blood in the stool and changes in bowel habits, are not very characteristic. If it is recognized early, the cancer has a very good prognosis. Since up to 6% of the healthy normal population develop colorectal cancer after their 40th year of life, there are structured preventive programs in Germany.
Read more on the topic: Colon cancer screening
Therapy of rectal cancer
The therapy of rectal cancer depends on its stage. A basic component of the therapy is the complete surgical removal of the tumor, this can also include the removal of metastases. The surgical procedure depends, among other things, on the location of the tumor. The accompanying chemotherapy and radiation therapy depends on the tumor stage and depends on the TNM classification (see above). In rectal cancer in stages II and III, radiation, possibly combined with chemotherapy (radiochemotherapy) before and chemotherapy after the operation, is recommended. This reduces the likelihood that the tumor will recur after the end of the therapy, improves the chances of survival and can lead to a gentler surgical therapy, ideally with preservation of the sphincter. If rectal cancer is an incurable tumor due to its spread or involvement of other organs, some measures can be taken to alleviate the symptoms. A stent, i.e. a tubular implant, can be used to ensure patency of the rectum. Alternatively, the mass of the tumor can be reduced using a laser. In order to prolong the survival time in the case of metastases, polychemotherapy (chemotherapy with several different active substances) can be carried out after weighing the risks. Individual liver and lung metastases can also be surgically removed to improve quality of life.
Read more on the topic: Colon cancer therapy
OP

The aim of surgical therapy for rectal cancer is to remove as much as necessary and as little as possible in order to get the tumor tissue out of the body as well as possible and, if possible, to maintain the function of the sphincter muscle. If a sphincter-preserving procedure can be performed, what is known as an anterior rectal resection is usually performed. The affected part of the rectum (= rectum) is removed (= resection) and the stumps are connected to each other again. In addition, the mesorectum, i.e. the anchoring of the rectum through the peritoneum in which vessels, nerves and lymphatic tracts run, is removed. If the rectal cancer is too deep in the rectum, it is not possible to preserve the sphincter muscle. In this case, the so-called "abdominoperineal rectal extirpation" is the treatment of choice. The rectum is removed from the abdominal cavity (= abdomen) as far as possible. The stump is then sewn into the abdominal wall. This creates an artificial anus. The remaining part of the rectum and the sphincter muscle are then removed from the pelvic floor (= perineum). The limit for maintaining the sphincter muscle is around 5cm above the anus.Nowadays, in 85% of cases, it is possible to operate on rectal cancer to preserve the sphincter. Very small, well-differentiated tumors that do not migrate into the lymphatic vessels can be removed endoscopically.
Read more on the topic: Colon Removal - Is Life Without It?
Irradiation
Radiation is recommended for rectal cancer in stage II and III before surgical therapy. The aim is to improve the operability of the tumor, reduce the likelihood of tumor recurrence and improve the survival rate. Either short-term radiation for one week, followed by the operation in the week after, or long-term radiochemotherapy, which combines radiation for 4-6 weeks with chemotherapy. In this case, the operation is performed 3-4 weeks after the chemoradiotherapy has ended. The choice of therapy depends on the surgeon's judgment of the primary operability of the tumor.
Metastases
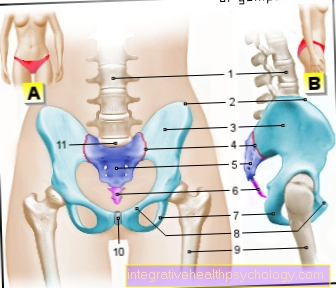
Many patients have already had the tumor spread to other parts of the body by the time they are diagnosed with rectal cancer. Depending on the location of the tumor, settlements can develop in the lymph nodes around the abdominal artery (para-aortic), lymph nodes in the pelvic wall and in the groin. The first organs affected by blood spread are the liver and, in deep-seated rectal cancer, the lungs. Subsequently, other organs can also be affected by the tumor, but this is less common.
Read more on the topic: Metastases in colon cancer
Concomitant symptoms
The symptoms of colorectal cancer are not very characteristic. Patients report, for example, blood in the stool. However, these can also occur in the course of other diseases, such as a hemorrhoidal disease. Often, patients with colorectal cancer also suffer from hemorrhoids. Conversely, the absence of bleeding does not rule out carcinoma. Sudden changes in bowel habits after the age of 40 can also indicate a malignant disease in the intestine. In addition, there can be foul-smelling winds and involuntary defecation in the flatus. In addition, patients report reduced performance and fatigue as well as weight loss and abdominal pain. Chronic bleeding from the tumor can also lead to anemia. In extreme cases, large tumors can lead to an intestinal obstruction and the associated symptoms.
Read more on the topic: Colon Cancer Symptoms
causes
20-30% of colorectal cancers occur in families. This means that a person who has a first-degree relative (especially parents) with colorectal cancer is 2-3 times more likely to develop it in their lifetime. In addition, some lifestyle factors play an important role. Especially overweight people (BMI> 25) who do not move regularly, smoke cigarettes and drink a lot of alcohol have an increased risk of developing colorectal cancer. In addition, a low-fiber, high-fat diet and a high consumption of red meat have an additional negative effect. Most colorectal cancers occur after the age of 50. The risk of developing such a disease increases with age. People with inflammatory bowel disease are also at increased risk of developing colorectal cancer. If there are a few cases of the disease in the family and the patients were noticeably young at the time of diagnosis, it makes sense to consider a genetic cause of the colorectal cancer. The genetic causes include Lynch syndrome, also called HNPCC (= hereditary non-polyposis colorectal cancer), FAP (familial adenomatous polyposis coli) or MAP (MYH associated polyposis). Patients with such genetic cancers are recommended to have closer preventive examinations in order to be able to identify and treat the development of malignant changes in good time.
diagnosis

The colorectal cancer is ideally recognized in the course of a preventive examination. This is recommended in Germany from the age of 50. A colonoscopy is usually done. This offers the possibility of recognizing abnormalities in the intestine directly, removing them and then examining the tissue. If the examination remains without abnormal results, a check-up is recommended after 10 years. Alternatively, the patient can be offered an annual examination of the stool for blood that is not visible to the naked eye (= occult). If this is positive, however, a colonoscopy is also necessary for further clarification. If the examination of the ablated tissue reveals that it is a malignant tumor, some further diagnostic measures are initiated in order to record the spread of the tumor as precisely as possible. These include, in addition to a complete colonoscopy, an ultrasound examination of the abdomen and an X-ray examination of the chest. A CT or MRI examination is also performed. In the case of rectal cancer, an examination with a rigid device, a rectoscope, is carried out to assess the height of the tumor. In addition, a blood test is carried out in which, among other things, the tumor marker CEA is determined to monitor the progress.
What does TNM mean?
TNM is a classification system for cancer which tries to describe the tumor and its spread as precisely as possible with its three letters. The T describes the tumor and its local spread. Since tumors also spread through the lymphatic system and blood in the body, it is not enough to just describe the tumor. Therefore, the N describes the involvement of the lymph nodes by tumor tissue. The M describes the settlement of the tumor in other organs, i.e. its metastases. After weighing these three factors, the tumor can then be assigned to a stage, according to which further therapy is based.
Read more on the topic: What does TNM mean?
What does neoadjuvant therapy mean?
Neoadjuvant therapy is a therapy that is used before the operation of tumors. This can be chemotherapy or radiation, which is intended to reduce the size of the tumor before the operation in order to improve the initial situation for the operation. This ideally ensures that inoperable tumors can still be operated on or that the operation itself has to be less extensive.
Guidelines
In Germany, the German Cancer Society, the German Cancer Aid and the Working Group of the Scientific Medical Societies in Germany (AWMF) are issuing standardized guidelines that set out the recommended procedure for diagnosis, therapy and follow-up treatment of cancer, including colorectal cancer, based on the latest studies, describe. In addition to clear guidelines for doctors, the AMWF also issues guidelines that are specifically aimed at patients and want to explain the diagnostic and therapeutic approach in an understandable manner. The current guidelines are freely available on the AMWF website and are valid until June 2018. There are various international specialist societies that, like the AMWF, issue their own guidelines based on current scientific knowledge. Such societies are for example the European Society for Medical Oncology or the National Comprehensive Cancer Network.
Follow-up treatment of rectal cancer

Follow-up treatment depends on the stage of the tumor. In addition to taking a medical history, recording current complaints and the physical examination, some examination techniques are an integral part of the follow-up care for rectal cancer. These include the determination of the tumor marker CEA, colonoscopy, ultrasound examination of the liver, X-ray examination of the chest and computed tomography of the pelvis. Since the probability of developing a second tumor is highest in the first two years, the follow-up examinations are particularly important during this period. In addition, health-promoting measures, in particular regular physical exercise and a healthy diet, are recommended to the patient to promote health.
Chances of recovery / prognosis
The chances of recovery and the prognosis of rectal cancer depend on many factors. In addition to the tumor stage, individual factors are also important. In 10-30% of cases, the tumor will recur after successful treatment for colorectal cancer. The highest risk of developing a second tumor is in the first 2 years, while after 5 years the risk of a relapse is very low. Surgery mortality is 2-4%.
Read more on the topic: Colon Cancer - What Is My Prognosis?
Life rate / chance of survival
The survival rate of rectal cancer is dependent on individual factors such as the general health of the patient or other concomitant diseases on the stage of the cancer. In medicine, the survival rate is often described as the 5-year survival rate. While statistically patients in stage I have a 5-year survival rate of 95%, the rate drops in stage II to 85% and in stage III to 55%. In stage IV the 5-year survival rate is only 5%.








.jpg)