Pain in the calf - what are some indications that I have a thrombosis?
introduction
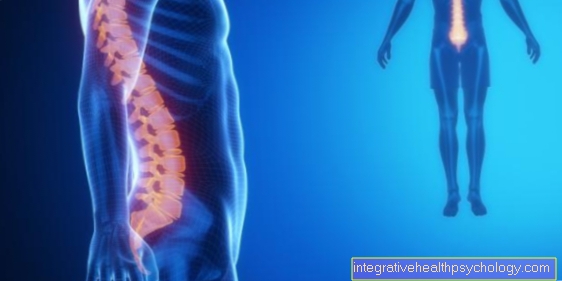
For deep vein thrombosis (Phlebothrombosis) a blood clot forms in the leg veins. This clot then closes the vein so that the blood cannot return to the heart at this point. Due to anatomical conditions, thrombosis occurs more often on the left leg. In addition to a rare hereditary variant, there are various risk factors that can promote the development of a thrombosis in the calf, such as immobilization, advanced age or pregnancy.

What are the symptoms of a calf thrombosis?
With a thrombosis - not just in the calf - there are 3 typical symptoms (Triad), which can be felt on the affected lower leg. However, this is only true in 10% of the cases. These include swelling of the calf, dull pain, and a blue-livid discoloration (cyanosis). The affected calf can also overheat. A feeling of heaviness in the leg and increased vein markings on the skin can also occur. If there is also shortness of breath, chest pain and dizziness, the emergency doctor should be informed urgently, as this can be a pulmonary embolism.
also read:
- Detect thrombosis
- Calf pain- Here are the causes
- Burning in the legs
swelling
The affected calf may swell. The increased calf circumference can be clearly noticeable compared to the other calf. If both calves are affected by a thrombosis, both legs can swell and the difference in circumference will no longer be as noticeable. The swelling occurs because the blood cannot continue to flow to the heart through the clot blocking the vein. A congestion occurs with fluid transfer from the vessel into the surrounding tissue. This is also known as edema. If edema develops, the skin on the affected leg can be pressed in, whereby the dent remains for a few seconds. It is best to test this on the front of the leg next to the shin.
Pain
The pain may be spasmodic or sore in the affected calf; but it can also be much stronger. In addition, there is tenderness along the affected vein where the clot is located. The compression of the calf can also be painful (so-called calf compression pain or "Meyer sign"). If you press on the sole of the foot, it can cause pain in the sole of the foot. Pain can also occur when pulling the foot towards the shin - i.e. when stretching the calf muscles.
Diagnosis of a calf thrombosis
The calf thrombosis can be noticeable in various ways. For example, a physical exam with calf compression pain (Meyer sign), Calf pain when pulling the toes towards the shin (Homans sign) or the pain on the sole of the foot when pressure is applied to the sole of the foot (Payr sign) Provide information on the presence of a calf thrombosis. However, these signs are not very reliable. Therefore, an ultrasound of the leg veins and a blood sample should be performed. Whether the blood draw or the ultrasound is done first depends on the likelihood of a calf thrombosis. This is determined by the Wells score, which classifies the probability of the presence of a venous thrombosis. This includes, for example, an anamnesis, whereby the question is asked whether a calf thrombosis has ever occurred. Immobilization (bed rest or paralysis) is also taken into account. Furthermore, each symptom on the leg gets a point (e.g. edema, circumference difference of> 3 cm compared to the opposite side, etc.). If the score is greater than or equal to 2, a calf thrombosis is likely and an ultrasound of the leg veins should be performed immediately.
Ultrasonic
The ultrasound of the veins - also known as compression sonography of the leg veins - is the method of choice when a thrombosis is suspected. The veins are followed by ultrasound from the pelvis to the feet and pressure is exerted on the veins, which cannot be compressed if there is a thrombosis. With this procedure, a thrombosis can be ruled out or diagnosed quickly and without radiation exposure. The only disadvantage of this method is that the examining doctor has to be familiar with the procedure or has to be trained in it - the compression sonography is therefore also dependent on the proficiency of the examiner.
Venography
Phlebography is an X-ray procedure in which the veins are displayed using contrast media. The contrast agent is injected into the superficial veins before the X-ray and is used to better visualize them. Thrombi can be reliably visualized if they are present. However, since this is a radiation procedure and there is a certain risk of side effects when injecting the contrast agent, sonography is preferred for diagnosing suspected calf thrombosis. However, if there is a suspicion of an occlusion of a vessel in the pelvic area, phlebography is indicated, since it can also assess the supply of surrounding organs in the pelvis.
Blood test
Especially if a calf thrombosis is unlikely, but still cannot be ruled out with certainty, a blood sample with a subsequent blood test is necessary. It can lead to an increase in ESR (Sedimentation rate) and may lead to an increase in white blood cells (Leukocytosis). The so-called D-dimers are also determined. D-dimers are breakdown products that are formed when a blood clot forms. A normal value almost completely rules out thrombosis. However, an increase in the value can not only occur in the case of a thrombosis, but also have other causes, such as in the case of a tumor or after an operation. A compression ultrasound of the veins should therefore always be performed if the D-dimer value is increased.
Coagulation diagnostics
In coagulation diagnostics - also known as thrombophilia diagnostics - a check is made after the indication is made whether the coagulation is working properly or whether certain proteins are too much or too little. Previous thromboses or familial thromboses, for example, are considered indications. The basic diagnostics then include the determination of the activity of protein S and C as well as antithrombin, all three of which serve to inhibit coagulation and, with reduced activity, cannot adequately counteract the formation of clots. The APC resistance is also determined. This results in resistance of the coagulation factor V to activated protein C. This means that protein C cannot inhibit factor V and there is increased clot formation and a tendency to thrombosis. In addition, the coagulation speed is checked using Quick and aPTT. If there are abnormalities in the blood test, further data will be checked.
You may also be interested in this topic: Protein C deficiency
How do you recognize a calf thrombosis during pregnancy?
Even during pregnancy, the signs of a calf thrombosis are pain in the calf, restricted mobility, swelling and reddening of the affected leg. If you have symptoms of this type, you should definitely consult a doctor, as there is an increased risk of thrombosis, especially during pregnancy. The doctor can use an ultrasound of the leg vessels to rule out or reliably determine a calf thrombosis.
Also read: Thrombosis in Pregnancy
What do you do if a calf thrombosis is diagnosed?
If a calf thrombosis is detected, immediate treatment should be initiated. On the one hand, the calves should be compressed using a wrap bandage, and later using compression stockings. The calf compression should be performed for 3 months. In addition, if possible, the patient should exercise to prevent the clot from progressing.
Another immediate measure is drug therapy. Anticoagulant medication is administered for at least five days after the thrombosis has been diagnosed. Mainly low molecular weight heparin or fondaparinux are given. Surgical procedures are generally not performed in the case of a calf thrombosis, unless there are pronounced symptoms and the medication does not improve.
Immediate therapy is followed by preventive therapy with anticoagulants, which can be taken in tablet form (oral therapy).How long the anticoagulant is continued depends on risk factors and concomitant illnesses as well as previous illnesses, especially with regard to previous thromboses. Thus, the treatment varies between 3-6 months.
Causes of a calf thrombosis
How a thrombosis develops is described by the so-called Virchow's triad. On the one hand, the change in the vessel walls (for example due to inflammation) is crucial. On the other hand, the slowing down of the blood flow speed (for example due to immobilization or external pressure on the legs) is one of the causes that favor the formation of thrombosis. A third possible cause is a change in the composition of the blood (for example due to genetic diseases or medication).
Whether a calf thrombosis occurs also depends on certain risk factors that can ultimately lead to Virchow's triad. The risk is increased in the case of a prolonged lack of exercise or immobilization of the legs, as is the case after an operation or on a long-haul flight. The flow speed of the blood decreases, whereby the blood sinks into the legs and the formation of thrombi is more likely.
Even if you are overweight (Obesity) With a BMI of over 30, the development of a thrombosis is more likely, as this can damage the vessel walls. In cancer - especially of the stomach, pancreas, lungs, lymphomas - the formation of clot-activating tumor proteins also increases the risk of thrombosis. Estrogen therapy - for contraception with the pill or during menopause - can increase the risk of thrombosis in the calf, especially in combination with nicotine (smoking). In the so-called antiphospholipid syndrome, an autoimmune disease leads to an increased tendency to thrombosis. Antiphospholipids are antibodies that bind to phospholipids and then reduce the function of anticoagulant proteins. This then leads to increased thrombus formation.
Furthermore, the risk of thrombosis during pregnancy and the puerperium is increased due to the hormonal change. An inherited increased tendency to thrombosis (Thrombophilia) consist. In this case, there are too many proteins involved in the coagulation process or too few proteins that inhibit coagulation. The defect can vary in severity.
More information on this topic: Causes of Thrombosis
Duration of a thrombosis
Normally, with appropriate treatment, a thrombosis does not change after about 2 weeks and an enlargement or complication such as the ascent of the thrombosis into the pelvic veins can be excluded. As a rule, therapy with blood thinners or anticoagulants lasts at least 3 months for a first-time calf thrombosis. If the thrombosis is severe, the therapy can be extended to 6 months. In general, however, the following applies: If the thrombosis recurs, the anticoagulation should be extended to one year. If an inherited or acquired tendency to thrombosis is determined, longer or even lifelong treatment should be expected.












.jpg)