Painkillers for kidney diseases

introduction
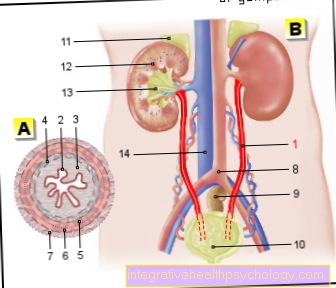
With diseases of the kidney, besides special symptoms of decreased kidney function, other problems also occur. A major problem with diseases of the kidney is the correct selection of important drugs. Almost all drugs are metabolized in the human body and then have to be excreted again. The substances can be excreted via two main systems: Active substances that are particularly soluble in water can be transported in the urine and excreted via the kidneys. Substances that are more soluble in fat are metabolized in the liver and excreted in the stool. The various ways of elimination also play an important role when taking painkillers, since in the case of diseases of the kidney, as few painkillers as possible should be used that are eliminated via the kidney.
These pain relievers are beneficial for kidney disease
-
Non-opioid analgesics (pain relievers)
-
Paracetamol
-
Metamizol (Novalgin®, Novaminsulfon)
-
Flupirtin (no longer permitted in Germany since 2018)
-
-
Opioids
-
Tramadol
-
Tilidine
-
Hydromorphone
-
Piritramide
-
These pain relievers are not good for kidney disease
-
NSAIDs
-
Diclofenac
-
Ibuprofen
-
Indomethacin
-
ASA (acetylsalicylic acid)
-
Naproxen
-
Celecoxib, etoricoxib, parecoxib
-
-
Opioids
-
Oxycodone
-
NSAIDs
The NSAIDs (non-steroidal anti-inflammatory drugs) also NSAID (non-steroidal anti-inflammatory drugs) are a group of drugs that have anti-inflammatory, analgesic and fever-lowering effects. Classic active ingredients in this group are diclofenac, ibuprofen, indomethacin, ASA (acetylsalicylic acid = aspirin) and naproxen. There are also some agents that work more specifically, including celecoxib, etoricoxib, and parecoxib. All non-steroidal anti-inflammatory drugs are eliminated primarily through the kidneys. Therefore, in the case of renal insufficiency (kidney weakness), the substances can accumulate in the body, because the active ingredients cannot be excreted as quickly. For this reason, a dose adjustment with a reduced dose of the pain reliever is necessary in the case of poor kidney function. It would be even better to avoid NSAIDs completely and use other pain relievers instead. Since non-steroidal anti-inflammatory drugs are excreted via the kidneys, they can also damage the kidneys if they are taken for a long time and thus cause temporary or chronic kidney damage themselves. Anyone who already has borderline kidney function before taking painkillers is therefore better advised to take painkillers other than NSAIDs. Non-steroidal anti-inflammatory drugs can also cause digestive tract discomfort. It is particularly common for them to cause ulcers in the stomach or duodenum. Therefore, NSAIDs should be given in combination with proton pump inhibitors (stomach protection).
Novalgin®
Metamizol (also Novaminsulfon or commercially available as Novalgin®) is a pain reliever and antipyretic substance. The exact mode of action of Novalgin® is not yet fully understood, but a mechanism of action through the inhibition of prostaglandins (a substance that accelerates inflammatory reactions) and an effect on pain processing in the brain is suspected. With regard to diseases of the kidney, Novalgin® is preferable to non-steroidal anti-inflammatory drugs in most cases. For example, if the kidney function is only slightly impaired, there is no need to adjust the dose, as no risk to the damaged kidney is to be expected. Most pain relievers that do not have a bad effect on the kidney will damage the liver with prolonged use. But in the case of Novalgin®, even with mild to moderate liver damage, no special precautionary measures and lower dosages need to be observed. In general, Novalgin® is considered to be a pain reliever with few side effects. A rare but serious side effect can be a blood formation disorder, which leads to what is known as agranulocytosis (a significant reduction in the number of granulocytes, a subgroup of white blood cells that are required for the immune system).
Here it goes to: Side effects of Nolvagin®
Morphine
Morphine belongs to the group of so-called opioids. These are strong painkillers that are available in a wide variety of strengths and groups of effects. In the case of diseases of the kidneys, the intake of morphines is basically possible. However, if the kidney function is severely impaired, higher concentrations of the active ingredient may be present in the body over a longer period of time. This is probably due to the fact that the excretion products of the morphine cannot be excreted as quickly in poor kidney function as is the case in a healthy kidney. Morphine and the products of morphine converted by the metabolism can be detected primarily in the liver, kidneys and gastrointestinal tract. Even if there can be a higher concentration of morphine and its breakdown products in the kidneys, it is not known that morphine damages the kidney in normal doses. Therefore, even with diseases of the kidneys, one does not have to fear that the kidney function could deteriorate through the normal administration of the morphine preparations. However, due to the reduced excretion with particularly low kidney function, dose adjustments may be necessary, as otherwise the active substance may accumulate too much in the body. This has similar effects as an overdose. This leads to decreased respiratory drive, dizziness, disorders of consciousness, an increase in heart rate and a decrease in blood pressure.
Read more about the here Side effects of morphine
Aspirin®
Aspirin® contains the active ingredient acetylsalicylic acid (ASA for short) and is a pain medication, which also prevents the cross-linking of blood platelets and can therefore also be used to thin the blood. In the meantime, people have abandoned the use of Aspirin® as a pain reliever. Instead, it plays an important role in diseases of the cardiovascular system such as coronary artery disease as well as in the prevention of strokes, acute occlusions of arteries and heart attacks. In contrast to non-steroidal anti-inflammatory drugs, aspirin can also be used as a pain reliever in cases of kidney disease. The substance may only no longer be used if the kidneys are moderately weak (renal insufficiency). The guideline value from which there is a contraindication for taking Aspirin® in the case of renal insufficiency is a GFR (glomerular filtration rate = value for the excretory function of the kidneys) of less than 30 ml / min.
Paracetamol
Paracetamol is a pain reliever that also has an antipyretic and pain reliever effect. It can be used as a pain reliever in both adults and children (in a dosage adapted to their age and weight). The exact mechanism of action of paracetamol has not been clarified, but it is assumed that the effects mainly develop in the spinal cord and in the brain itself. Since paracetamol is largely metabolized and excreted via the liver, there is nothing to fear in most cases of kidney disease. For example, people with kidney disease can usually take the same dose of paracetamol at the same time intervals (ideally at least 6 hours) as people with healthy kidneys. Only in the case of severe kidney insufficiency (kidney weakness) with a glomerular filtration rate (GFR = value for kidney function) of less than 10 ml / min should a lower dose of paracetamol be taken, as otherwise the substance will accumulate in the body and thus increase Symptoms of poisoning can occur. In this case, the interval between two paracetamol intake times should be at least 8 hours. While healthy adults can take up to 4g paracetamol per day, a maximum of 2g paracetamol should be taken daily for diseases of the kidney.
What other drugs increase kidney damage?
Besides the liver, the kidneys are the most important place where drugs and toxins can be eliminated from the body. Therefore, a large number of drugs at high dosages or long-term use can lead to kidney disease. In particular, people who already have kidney disease have to make many restrictions on their medication. In the case of kidney disease, many drugs cannot be broken down quickly enough so that the active ingredients can be taken in lower doses; one speaks of a kidney-adapted dose of the medication (adapted to the kidney function). In addition to pain relievers, many stimulants such as nicotine can also increase kidney damage. Some antibiotics, such as the aminoglycoside group, can cause severe kidney damage if doses are too high. Medicines that work against viruses (for example the substance acyclovir) can also increase damage to the kidneys. Another group that can lead to increased damage to the kidneys are the cytostatics. These are active ingredients that prevent the growth and multiplication of cells and are often used in the field of cancer.
What can I do to minimize pain medication damage to the liver?
Many pain relievers do not work well in kidney disease. This is mainly because these drugs are eliminated through the kidneys. Other pain relievers are often used to prevent damage to the already diseased kidneys, for example from non-steroidal anti-inflammatory drugs such as ibuprofen and diclofenac. In the case of kidney disease, pain relievers that are best used are those that are not excreted via the kidneys but rather via the liver. The classic example of such a pain reliever is paracetamol. Long-term use of paracetamol in high doses can also damage the liver, as it can now be overburdened by the metabolism and excretion of the active ingredients. In this case, it is important to find a good compromise between drugs that are more likely to be excreted by the kidney and those that are processed by the liver. Depending on which organ is more severely affected, painkillers that are more heavy on the liver or kidneys can be used. With regular monitoring of the liver and kidney values, both organs can often be spared a little. For example, you can take ibuprofen and paracetamol alternately and thus neither overload either of the two organs. In addition, reducing the daily dose of the medication can relieve the strain on the liver and kidneys. If the pain medication in the reduced dose is not sufficient, stronger pain relievers such as morphine can be used. These do not attack the liver and kidneys as much. In addition, they can be given, for example, in the form of a pain plaster, which continuously releases its active ingredient over a period of one week. This avoids sudden high concentrations of the active substance (as can occur, for example, after taking a tablet).
also read: Pain relievers for liver diseases








.jpg)