This is how a stroke is diagnosed
introduction
If a stroke is suspected (e.g. through the clinical FAST test), immediate, emergency diagnostics must be carried out to confirm it - the subsequent therapy depends on the cause of the stroke.
For this purpose, a CT is primarily done for imaging, if more precise results are required, an MRI can also be used. The CT or MRT can then be used to differentiate whether the cause is a cerebral haemorrhage or a vascular occlusion. Further examinations are usually carried out to clarify the cause of a vascular blockage.
Diagnostic steps of a stroke
The first suspicion of a stroke is made by a characteristic clinic, i.e. on the basis of certain symptoms that can be ascertained using the FAST test.
You might also be interested in: These are typical signs of a stroke!
Once the suspicion arises, an investigation must be carried out as soon as possible to determine whether the cause of the stroke is a cerebral hemorrhage or an occlusion of cerebral vessels. This is important because in both cases the respective emergency therapy differs significantly.
Also read:
- Causes of a stroke
- Stroke therapy
Computed tomography (CT) is primarily suitable for this; if this is not sufficient, magnetic resonance tomography (MRT) can also be performed. The CT can be expanded or supplemented by vascular imaging (CT angiography) or blood flow measurement (CT perfusion). In this way, it can be narrowed down which vessel is closed and which brain area is affected by the reduced blood flow to what extent.
For more information, we recommend our website to: MRI for a stroke
1. FAST test for initial assessment
The FAST test is a way of making a quick initial diagnosis of a stroke.
FAST stands for face (face), arms (arms), speech (language) and time (time) and combines all major symptoms of a possible stroke: a drooping corner of the mouth (one-sided paralyzed facial muscles) in the face, one-sided paralysis of the arm ( this can no longer be fully raised) and a slurred language or even the inability to speak. The T for time stands as a reminder that in the event of a possible stroke, every minute counts and further diagnostics must be carried out immediately with rapid initiation of therapy.
For more information, we recommend our website to: These are the signs of a stroke!
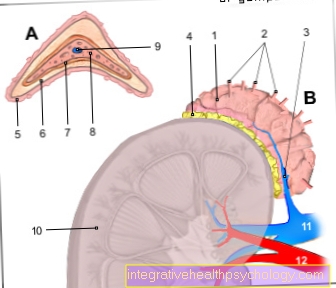
2. CT of the head to clarify the cause
When doing a CT scan of the head, the brain is shown in thin layers using X-rays. With the help of these layers, information can be given about what the cause of the stroke was - whether a cerebral hemorrhage or a blood clot in the vessel prevented the blood supply to a certain area of the brain.
Another option is a CT angiography, i.e. a special vascular representation of the brain in the CT and a CT perfusion, which is a special blood flow measurement of the brain. For this purpose, a contrast agent is given over the veins so that the cerebral vessels can be better visualized and circulatory disorders can be better detected.
The CT examination is carried out to quickly clarify the cause, since the therapeutic options for a stroke differ depending on the cause. We therefore recommend our site to:
- Causes of a stroke
- Stroke therapy
If you would like more information on computed tomography, please read: CT imaging
2. MRI of the head to clarify the cause
An MRI of the head is also a pictorial representation of the head or the brain in thin layers, but unlike CT, no X-rays are used here. The image is created with the help of a strong magnetic field and electromagnetic waves. The MRI enables a fairly accurate representation of the stroke and this also earlier than a CT, which is why it is also used for early diagnosis or for more precise clarification. A disadvantage here is that performing an MRI takes significantly longer than performing a CT and that an MRI is also significantly more expensive. This is the reason why the MRI is therefore usually not used directly as the first examination method for emergency diagnosis in the event of a stroke. If the beginning of the stroke is unclear. or cannot be named by the person concerned, MRI is usually preferred, since emergency therapy can no longer be initiated anyway.
More about this topic can be found: MRI for a stroke
3. Initiation of therapy
Once the cause of the stroke is known, therapy can be started. This differs depending on the cause.
Read more about this at: Stroke therapy
Further diagnostics for stroke prophylaxis
After the stroke has been treated and the patient is no longer in danger, the cause is further clarified. This is important to prevent another stroke. Because, contrary to what was thought, a stroke does not always come from the brain itself, but mostly from cardiac arrhythmias or a narrowing of the neck vessels.
Examination of the neck vessels
An ultrasound examination of the cervical vessels (Carotid Doppler, FKDS = color-coded Doppler sonography) as part of a stroke diagnosis is useful because the cerebral blood flow occurs through the cervical vessels. The blood is ejected from the heart via the neck vessels into the blood vessels supplying the brain.
If, in the course of life, there is increased calcium deposits in the area of the cervical vessels and thus increasing occlusion of the cervical vessels, the blood flow to the brain also decreases. From a certain degree of occlusion of the jugular veins, the adequate blood supply to the brain is no longer guaranteed, so that a stroke can occur.
Read more on this topic at: Calcified carotid artery - what are the causes and risks
Examination of the heart - EKG
Carrying out an ECG as part of stroke diagnosis is also useful, as certain cardiac arrhythmias increase the risk of a stroke. If there is primarily atrial fibrillation in the heart, the risk is significantly increased that blood clots (so-called thrombi) will form in the area of the right atrium. These blood clots can loosen and then get from the heart via the neck vessels into the vessels supplying the brain and block them. The occlusion of vessels supplying the brain then leads to a stroke. If there is atrial fibrillation, it is absolutely necessary to take blood-thinning medication that prevents the formation of such blood clots.
Read more on this topic at:
- Atrial fibrillation - you should know that!
- EKG changes in atrial fibrillation
Examination of the heart - echocardiography
In addition to an EKG, a swallow echo can also be performed. For this purpose, a special ultrasound device (sonography device) is inserted into the esophagus through the mouth and an ultrasound of the heart is performed from there. The heart can be represented in its individual structures, as can the adjacent vessels. This means that blood clots in the heart, preferably in the right atrium or auricle, can also be shown and proven. If a stroke has occurred or if a stroke is suspected, the detection of such thrombi is a clear indication of a stroke due to a blockage of a brain vessel by a blood clot.
Further information on this topic can be found at: Echocardiography
Examination of the brain - EEG
The EEG (electroencephalogram) is a measurement of the electrical activity of nerve cells in the brain, also known as brain wave measurement. An EEG can sometimes be used to make statements about the function of the various brain regions, which can be useful in the context of a possible stroke. If a stroke is suspected or if a stroke has occurred, the EEG can be used to assess the area and extent of the brain damage. In addition, disturbances in the EEG can indicate whether, for example, there is a tendency for epileptic seizures after a stroke or not.
For more information, see: electroencephalogram
You might also be interested in: Diagnosis of epilepsy
Further questions
Can you diagnose a stroke in the blood?
Whether a stroke has occurred cannot be seen directly in the blood count. However, if a stroke is suspected or if a stroke has already been diagnosed, it can be useful to determine not only the red and white blood cells but also the number of platelets (thrombocyte count) and the blood coagulation values.
If, for example, there is a pathological disorder in the coagulation system, the blood platelets tend to clump together, which can cause the sometimes life-threatening blood clots to form and, for example, block the cerebral vessels. Furthermore, evidence of inflammation or infections should be observed in the blood, as this can promote increased blood clotting.
Read more on this topic at: Bleeding disorder



















.jpg)