Spondylodiscitis
Definition of spondylodiscitis
Spondylodiscitis is a combined bacterial inflammation of a vertebral body (spondylitis) and the adjacent intervertebral disc (discitis).
A distinction is made between specific spondylodiscitis and non-specific spondylodiscitis.
- Specific spondylodiscitis is inflammation (infection) with the tubercle bacterium. It is a disease that has become rare (skeletal tuberculosis). The disease process is mostly insidious and less acute (sudden) than in the non-specific form. The bacteria are settled via the bloodstream (hematogenous).
- Nonspecific spondylodiscitis is an inflammation that can be caused by all pus pathogens. The most common pathogen is the bacterium Staphylococcus aureus. Due to the far more frequent occurrence, the following article concentrates on the presentation of unspecific spondylodiscitis.

Appointment with a back specialist?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The spine is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
The treatment of the spine (e.g. herniated disc, facet syndrome, foramen stenosis, etc.) therefore requires a lot of experience.
I focus on a wide variety of diseases of the spine.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
Spondylodiscitis disease development
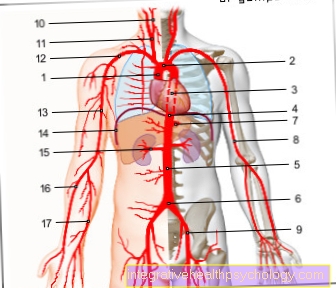
In spondylodiscitis caused by the bloodstream, the inflammation begins in the end plates of the vertebral bodies. From there it spreads to the intervertebral disc. The speed with which such a spread occurs depends on the number of bacteria responsible for the infection and the general immune system (immune system) of the patient. According to the common arterial blood supply, two neighboring vertebral bodies are more often affected by inflammation at the same time.
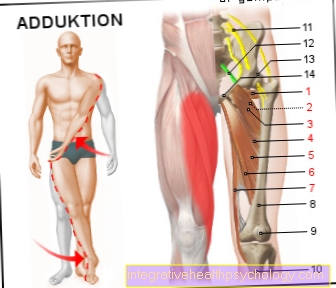
If the inflammation is severe, the infection can spread further. If the spinal canal is reached (Epidural abscess) are these Spinal cord and an ascending infection also puts the brain at risk (meningitis, Encephalistis). In the field of Lumbar spine the inflammation can spread along the Psoas muscle (Hip flexors) continue into the thigh (subsidence abscess).
Symptoms of spondylodiscitis
The signs of spondylodiscitis are often easy to confirm with hindsight, but often very unspecific and vague when they first appear. Typical is a severe pounding painwhich is noticeable precisely above the inflamed vertebrae. Even lightly tapping the affected area triggers extreme pain. Tension pain when the skin above the inflammation is only touched is rarer, but this can also be the case. The pain is classic dull and piercing and also very strong at night.
In addition to this triggerable pain, many patients complain Back pain in general. Even minimal movements - especially bending forward - are very painful. Also so-called axial loads such as those triggered when climbing stairs, for example, increase the symptoms. This results in a pattern that is typical for patients with spondylodiscitis stiff posture.
If the inflammation also affects the spinal cord or if a part of the diseased vertebral body shifts there, it can also cause neurological symptoms how Paralysis, Sensory disturbances or Paresthesia come. In addition, very general symptoms are found in chronic spondylodiscitis diseases: Those affected may suffer from fever, night sweats or weight loss without being able to explain the cause.
If the disease is finally well advanced, another symptom is quite clear, which then even enables a visual diagnosis: In severe spondylodiscitis with large destruction of the vertebral body, a so-called occurs Gibbus to observe; a very acute-angled hump that makes the patient walk and stand bent forward.
Cause of spondylodiscitis

The most common causes of nonspecific vertebral body and disc inflammation / spondylodiscitis are (1. + 2.) The settlement of bacteria in the vertebral body and the intervertebral disc via the bloodstream as part of blood poisoning (bacteremia, sepsis) and (3.) which was caused by the doctor himself (iatrogenic) Inflammation from a spinal surgery.
- Any bacterial inflammation in a patient's body can theoretically lead to bacterial seedling. Common causes are gastrointestinal infections (bacterial enteritis), Bladder infections (Vesiculitis, cystitis) and lung infections (pulmonary infections).
Spondylodiscitis causative agent
First and foremost, the unspecific spondylodiscitis by the Staphylococcus aureus bacterium caused. The spread of excitation can either be on the inner (endogenous) or outer (exogenous) Way.
In which endogenous way get the bacteria from infection in the body, beyond the Vertebral body, into the bloodstream and from there to the affected parts of the Spine (hematogenous). The pathogens can be transmitted both through the venous ("leading to the heart") and arterial ("leading away from the heart") blood circulation. In addition, inflammation can also come from infected lymph fluid to be triggered (lymphogenic).
Endogenous spread of excitation is not uncommon in patients with a weak immune system of the immune system in the context of e.g. Diabetes mellitus, more chronic Alcohol and drug abuse, Tumor diseases or previous, chronic inflammation.
There is also the exogenous way. Here lies the Focus of infection in the affected vertebral body or the Intervertebral disc itself. Impurities or non-sterile work operations near the spine or Injections smuggle the pathogens directly into the body. In some cases (10-15%), exogenous infections are one MRSA pathogen (Methicillin Resistant Staphylococcus Aureus), which due to its insensitivity (resistance) towards many Antibiotics, has become a major problem in many hospitals.
In addition to the Staphylococci Staphylococcus aureus (36%) gram negative bacterialike in that Intestines occurring Escheria coli (23%) or Pseudomonas aeruginosa (5%) non-specific spondylodiscitis. Furthermore, in 19% of the cases Streptococci, how Streptococcus sanguis verifiable.
Fungi and parasites are extremely rare as a pathogen to be determined, and therefore not mentioned by name!
The clinical picture of specific spondylodiscitis is caused by pathogens tuberculosis, mostly that Mycobacterium tuberculosis, caused. The infection occurs always via the endogenous route. HIV positive Patients with tuberculosis have a particularly high risk of developing specific spondylodiscitis.
- Open injuries leading to local infection can lead to bacterial colonization.
- For spinal surgery (Operations) bacteria can enter the Intervertebral disc or enter the vertebral body, e.g. as part of a disc operation, stiffening operation (Spinal fusion), discography and much more Since such an infection can never be completely ruled out, even if all hygiene regulations are adhered to, a thorough explanation of the risk of infection of the operation is given in advance of a planned spinal surgery, together with a description of the possible consequences that could result from such an infection. Fortunately, such infections are rare.
alcoholism, Diabetes mellitus, Tumor diseases are important comorbidities of a patient that cause the formation of a Spondylodiscitis can favor.

MRI spine
- The embedded pus can be recognized by the bright appearance of the vertebral body
- Discitis. The adjacent intervertebral discs are also affected by the infection.
- Representation of a healthy vertebral body
- Ileopsoas muscle; No subsidence abscess to be seen yet
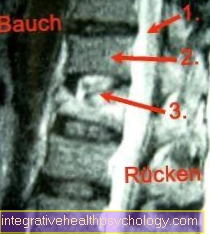
MRI of the spine on the side
- Spinal canal
- Healthy vertebral bodies
- Spondylodiscitis. The collapse of the vertebral body in the event of severe infection can be recognized
Diagnosis of spondylodiscitis

Crucial indications for the existence of a Spondylodiscitis In addition to the complaints described, the medical history (anamnese) deliver.In particular, it should be asked whether infections have recently occurred in other organs of the body and how these have been treated. It is also of particular interest whether a spinal surgery was performed recently or a long time ago.
The standardized examination of an inflammatory process in the area of the spine includes a blood test with determination of the inflammation values (see above). Are the complaints (Back pain and possibly fever) in accordance with the determination of increased inflammation values, then there is a well-founded suspicion of a vertebral body infection.
The X-ray image the suspicious spinal column is also one of the first diagnostic measures Spondylodiscitis. In very advanced cases of infection, there may be changes in the normal radiographic image of the vertebral bodies (shading, lightening). The height of the intervertebral discs may be reduced. In very advanced cases of spondylodiscitis, destruction of the vertebral body (osteolysis) or an inflammation-related collapse of the vertebral body can be observed. These are very late signs of severe vertebral infection. In many cases the x-ray can be completely normal.
In order to prevent such a degree of vertebral body destruction through timely therapeutic countermeasures, early confirmation of the diagnosis is of crucial importance. Magnetic resonance tomography (MRT, NMR especially of the lumbar spine) represent typical changes of a vertebral body and intervertebral disc infection by the formed pus (Pus) can be detected as an accumulation of fluid. It is also possible to assess the strength and spread of the infection. Therefore, if there is a well-founded suspicion of a vertebral body infection, a MRI examination of the respective region (cervical spine, thoracic spine, lumbar spine) should be carried out at an early stage.
Therapy of spondylodiscitis
The key to successful treatment of spondylodiscitis is consistent Immobilization the patient's spine. So-called orthotics, which are put on like a corset, fix vertebral bodies and intervertebral discs. An alternative to this is plaster of paris. With both immobilization positions, the patient is allowed to stand up and move around as much as he can. If the spine is not completely immobilized with these aids, only one option remains: absolute bed rest. The patient is then not allowed to get up for at least 6 weeks in order to keep his back as still as possible.
The second cornerstone of therapy is the gift of Antibiotics, which is an indispensable part of every spondylodiscitis treatment. In addition to these two measures, a operative therapy spondylodiscitis should be considered. In certain cases, which are explained in more detail below, an operation supplements and completes the chosen treatment path. In addition, it should not be neglected that it is efficient and satisfactory for the patient Pain therapy. Especially with long periods of rest and therapy, the person affected should at no time have to suffer more pain than necessary.
Antibiosis
The Choosing the right antibiotic is crucially crucial for the patient's recovery, as only one targeted therapy is possible.
Therefore, the causative agent of unspecific spondylodiscitis, as well as its sensitivity to antibiotics and possible resistance. The easiest and fastest way to detect pathogens is through the Creation of blood cultures. A Removal of the affected tissue (biopsy) or one Sampling through a minor operation under anesthesia are other options. Compared to the blood cultures, pathogens can be eliminated by these methods more accurate and safer determine. However, they cost a lot more time and effort.
Read more about this topic here: biopsy
However, there is quick action needed and the patient's condition no longer allows the pathogen to be detected intravenous antibiotics administered, which acts broadly against the most common causes of spondylodiscitis: Staphylococcus aureus and Escheria coli.
If the pathogen has now been determined, an targeted antibiotic therapy by infusion (,Drip'). The first choice is usually one Combination therapy, i.e. the simultaneous administration of different antibiotics. Be combined Clindamycin (1800 mg per day) plus Ceftriaxone (2g per day), which alternatively by Ciprofloxacin (800 g per day) can be replaced.
By administering the drug into the vein (intravenous) becomes a greater effectiveness achieved because the antibiotic does not Gastrointestinal tract has to happen and is metabolized there. In addition, some antibiotics can only be used directly blood be included.
The course and the causative agents of the spondylodiscitis vary considerably, so it is currently still no consistent guidelines on duration the therapy gives. As a rule, antibiotics are administered intravenously and over a period of about 2-4 weeks. If the general condition and the blood values (inflammation parameters) of the patient improve, a oral therapy in the form of tablets or capsules to be switched. Depending on the course of the spondylodiscitis, these must up to 3 months be taken. The duration of therapy can even be extended for high-risk patients.
Long-term antibiosis put additional strain on the body. Numerous side effects can occur. Often suffer kidney and liver under the constant administration of medication. Therefore, it is important that with long-term antibiotic therapy Liver and kidney values checked become.
Surgery for spondylodiscitis
The surgical treatment option for spondylodiscitis is the Opening of the inflamed area to inspect and assess the existing damage by the surgeon. The so-called ventral access chosen, so the exposure of the vertebral bodies coming from the abdomen. The patient lies on his back during this operation. At the beginning, the surgeon takes samples of the inflamed area, which are then examined for the type of pathogen and the effectiveness of various antibiotics.
It follows the surgical clean up of inflammation, that is, a generous removal of infected tissue and necrotic parts. After this as Debridement In this step, the wound is rinsed thoroughly and often treated directly with an antibiotic.
This work step then follows - as soon as the surgeon is sure that the inflammation situation has improved - a so-called Spinal fusion, so one Blocking of several vertebral bodies, on. This serves to stabilize and stiffen the spine and is usually done using a system of metal screws and rods. More rarely, healthy bones from the patient are taken elsewhere and moved for stabilization. However, individual details of the operation and the technique used differed significantly depending on the hospital and surgeon. A doctor will inform the patient of more precise details if such an intervention is planned. For example, some doctors treat everything directly in a single operation, while others do the so-called two-stage procedure and perform a second operation after a (minor) first operation and an appropriate break. For those affected, this procedure has the advantage that they only have to undergo smaller, shorter interventions and can recover between the two operations. On the other hand, a two-stage procedure of course always means another operation with another anesthetic and all the risks that an intervention entails. The decision for a one- or two-stage procedure must therefore be carefully considered and carefully considered in each case.
Read more on the topic: Spinal fusion
After the operation, the stabilization causes a complete Removal of mobility in the fixed segmentOn the one hand, this protects against subsequent vertebral body fractures and, on the other hand, leads to faster, more reliable healing of the spondylodiscitis. Operated patients are allowed to move to their normal extent relatively soon, whereby the loss of mobility caused by the operation is in most cases well tolerated and does not represent too great a limitation.
Reasons to operate on a patient with spondylodiscitis are the presence neurological failures (for example paralysis, paralysis or sensory disorders), the Failure of non-surgical therapy or one extensive bone destructionwhich already leads to a distinct hump. Even patients whose pain cannot be relieved even with optimal therapy should be treated surgically. On the other hand, very old, frail patients or those who are very weak should not be operated on. Since every intervention is associated with risks, these patient groups should rather be treated without an operation.
The greatest risk of surgery for spondylodiscitis is paraplegia caused by the surgeon. However, this complication is very rare, especially with the ventral access explained above.
Duration of treatment
On average, it takes 2 months to half a year from the first symptom to the final diagnosis by a doctor. Once the correct diagnosis is found, they close Immobilization and antibiotic therapy for several weeks on. The antibiotic is usually given directly into the vein over a period of 2-4 weeks (intravenous therapy). A sign of the success of the therapy is a drop in the inflammation values in the blood, which must be checked regularly. After the inflammation values have normalized, the antibiotic can be switched from intravenous to oral administration - usually in tablet form. These tablets should then be used again for at least one 4-6 weeks be taken. In severe cases, a period of up to 3 months may be necessary. All treatments and control examinations therefore often extend over a period of over a year for an individual patient until a final cure can be spoken of.
Prognosis of spondylodiscitis

The prognosis for the healing of a spondylodiscitis depends on various factors and therefore cannot be given a general description. The following are important:
- Extent of infection at diagnosis
- Bacterial species
- Conservative / Operative Therapy
- Overall physical condition of the patient / previous illnesses
Despite optimal acute therapy, it cannot be completely ruled out that the infection may not flare up after years.
The prognosis for spondylodiscitis in children is favorable. Operations are almost never necessary.
Treacherous in children are the hidden symptoms of spondylodiscitis, such as uncharacteristic back or abdominal pain and abnormal gait, which often delay a correct diagnosis.