Symptoms of heart failure
introduction
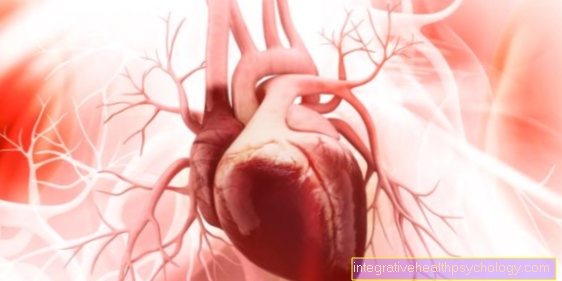
The symptoms of cardiac insufficiency (heart failure or heart failure) differ depending on whether the disease affects only the right, only the left or both halves of the heart. If the muscles of the left ventricle are weak, the main symptoms are, for example, shortness of breath (dyspnea) and poor performance.

Typical symptoms of heart failure
Typical symptoms of heart failure include:
- Exhaustion, decreased performance
- Weight gain without increased food intake
- Water in the legs (leg edema)
- Water in the abdomen (ascites)
- Shortness of breath (dyspnoea)
- Urinating at night (nocturia)
- Acceleration of the heartbeat (tachycardia)
- Left chest pain
- Cough if you have heart failure
Water in the legs
A common symptom of a chronic, long-term heart failure is the accumulation of water in the legs, also known as leg edema.
These occur because the blood accumulates in front of the heart when the heart is unable to pump sufficiently quickly and strongly. This causes fluid to leak into the tissue, which is especially noticeable in the legs due to the force of gravity. Those affected often complain of heavy legs and a pulling sensation, as the skin on the legs is tensed and stretched by the accumulation of fluid. The water in the legs is often accompanied by increased urination at night as the body tries to get rid of the fluid.
Also read our topic:
- Swollen legs
water in the lungs
With advanced heart failure, water can accumulate in the lungs. This is also known as pulmonary edema and is caused by the rise in blood pressure as part of the weak heart.
At a certain point the lungs can no longer withstand the pressure of the vessels and water accumulates. The water in the lungs usually manifests itself as severe shortness of breath, together with a rattling noise when breathing and coughing fits. As this can have serious effects, a doctor should be consulted as soon as possible. Depending on its severity, the water in the lungs is treated with the administration of oxygen, the straightening of the upper body and dehydrating medication, i.e. diuretics.
More information on this topic:
- Signs of water in the lungs
Shortness of breath
In many people who suffer from a weak heart, this shows up, among other things, through various breathing difficulties.
This includes the general feeling that it is difficult to breathe and that there is increasing difficulty in breathing. Many also have coughing attacks, which occur mainly at night and are associated with shortness of breath. This is also known as cardiac asthma and is favored at night by the fact that the lungs are under more pressure when lying down. Furthermore, breathing difficulties usually increase with physical exertion and it is more difficult, for example, to climb stairs. If breathing becomes more and more difficult, a doctor should be consulted as soon as possible in order to detect any accumulation of water in the lungs at an early stage.
- Difficulty breathing due to a weak heart
Water in the stomach
Heart failure can cause the blood to build up in front of the heart because it can no longer be pumped adequately through the heart. This collects fluid that can also escape into the connective tissue of the abdomen. This accumulation of water in the abdomen is also known as ascites and leads to a feeling of excessive bloating. Pain rarely occurs when there is water in the abdomen, but usually a feeling of discomfort.
Since the liver is usually under increased pressure when the blood backs up, the water in the abdomen can be associated with jaundice, for example. In addition to treating the heart failure itself, diuretics, i.e. water-boosting drugs, can help with ascites.
You might also be interested in this topic:
- Congested liver
Nocturnal urination
Many people with heart failure also urinate frequently at night.
This is also known as nocturia once the affected person uses the bathroom at least twice a night. The reason for this is the accumulation of water in the body, especially in the legs, due to the inadequate pumping function of the heart. At night, an attempt is made to flush out the liquid again. For those affected, this means that sleep is no longer relaxing. This will intensify the already existing reduction in performance. In addition, the shortened sleep leads to headaches and concentration problems for many.
Accelerated heartbeat
If the heart is weak, the heartbeat can accelerate. This can be seen as a kind of compensation for the heart as it is no longer able to pump enough blood at the normal rate of the heartbeat.
In many cases, the accelerated heartbeat is also a cardiac arrhythmia that arises from an incorrect supply of the nerves that are responsible for the heart's function. This can lead to an increase in the speed of the heartbeat. This is sometimes expressed by a palpable palpitations, which in many cases can be felt at night. However, many do not notice the change in heartbeat either, and this is only determined during a medical examination.
This topic might interest you:
- Therapy of palpitations
- Heart failure and high blood pressure
Left chest pain
If pain occurs in the left chest as part of a weak heart, this is in the vast majority of cases an acute situation.
The pain is not a typical symptom of a chronic, i.e. long-term heart failure. On the contrary, they usually signal that the heart is acutely overloaded and that action must therefore be taken quickly. Acute heart failure can also manifest itself through changes in cardiac activity, such as palpitations, as well as acute shortness of breath and cold sweat. If you have any questions, you should therefore not hesitate to consult a doctor.
Also read:
- Heartache- How dangerous is that?
Heart failure complications
Cardiac arrhythmias
Heart failure is often associated with cardiac arrhythmias.
The reason for this lies in the structure and function of the heart: the rhythm and the speed of the heartbeat are determined by certain nerves that lie directly on the heart. If the heart is weak, there is a change in the blood supply to the body and thus to the heart itself. As a result, the nerves that set the rhythm of the heart can also be undersupplied, which can lead to cardiac arrhythmias. This can e.g. express themselves through an accelerated heartbeat, but also through an irregular heart rhythm. Since you do not necessarily notice this yourself, it is advisable to consult a doctor for clarification if you have other symptoms that indicate cardiac insufficiency.
Also read: Life expectancy with heart failure
Sudden cardiac death
Sudden cardiac death is the unexpected death of a person from heart failure.
It can occur in connection with many diseases and is therefore also a possible complication in the presence of cardiac insufficiency. The number of people who die of sudden cardiac death due to heart failure has decreased significantly in recent years. It is believed that the improvement in drug treatment for heart failure is responsible for this. Sudden cardiac death usually occurs without any previous symptoms. Those affected suddenly fall over and their pulse can no longer be felt. In such a situation, an emergency doctor must be alerted as soon as possible. Occasionally, a brief faint occurs beforehand.
Mechanism of left heart failure
The left half of the heart pumps blood into what is known as the body's circulation, i.e. it supplies the entire organs of the body with blood and thus with the vital oxygen that is required for all necessary processes. The symptoms of heart failure result from the lack of oxygen in the various organs.
The fact that the brain is not supplied with enough blood can lead to decreased performance and poor concentration.
In more severe cases of left-sided heart failure, dizziness, lightheadedness, or even clouding of consciousness can sometimes occur.
Due to the permanent lack of oxygen in the tissues, mucous membranes can turn blue; this is known as "cyanosis".
In addition, one can often notice that hands and feet are unusually cool and the sweat also appears rather cold.
Because the left heart is no longer able to continue pumping the blood sufficiently when the left heart is weak, it accumulates in the veins that deliver the blood to this half of the heart. Because these come from the lungs, these pulmonary veins can become excessively filled with blood. If the pressure in these vessels becomes too high, blood is pressed out of them into the tissue, so to speak. This leads to the accumulation of water in the lungs.
This results in severe shortness of breath, which can be felt as restlessness, dry cough and / or exhaustion. When listening to the lungs, you can hear seething breathing noises. It is noticeable that many patients with weakness of the left heart sit with their torso very upright to breathe easier. Even when sleeping, many people use several pillows or a high bed to get better air through the sitting position.
Especially at night, those affected often experience attack-like shortness of breath, which is also known as cardiac asthma.
Read more on the topic:
- Heart failure
Right heart failure
If the muscles of the right heart in particular are affected by the weakness, other symptoms result.
The right half of the heart absorbs the deoxygenated blood from all organs and pumps it further into the lungs, where it is supposed to be enriched with oxygen again.
Because the right heart of those affected is too weak to continue pumping the blood, it collects in the supplying veins.
This accumulation can lead to a backlog of fluid in the tissue.
This is particularly noticeable in the lower legs, especially in the area of the ankles (in this region the water is most likely to remain due to gravity), the fluid accumulates and swells (Leg edema). These swellings are associated with an increased risk that the skin of the affected areas will dry out due to the increased tissue pressure.
This can cause eczema to develop (Congestion eczema), which in the course of the process can become real wounds, which then heal with difficulty due to the reduced blood flow and should therefore not be underestimated.
But some internal organs can also accumulate water due to the backlog of blood and consequently swell.
The liver is often affected, which can lead to pain under the right costal arch, and the digestive organs, which are noticeable as loss of appetite, a feeling of fullness and loss of function.
In addition, water can accumulate in the abdomen, this is known as Ascites.
Many patients complain of an increased need to urinate during the night (Nocturia). This is because, on the one hand, the blood flow to the kidneys increases when lying down and, on the other hand, the fluid that has accumulated in the tissues during the day can now drain away and has to be excreted.
If both halves of the heart are equally affected, one speaks of one global heart failure.
This is the most severe form of heart failure as it causes symptoms in both the right and left ventricles. Those affected have a very limited quality of life and often have cardiac arrhythmias that can sometimes be life-threatening. You must be treated.
The heart failure will depend on the severity of the New York Health Association divided into 4 groups (NYHA I to IV):
The NYHA I group includes patients who do not yet show any limitations. So you are still resilient and have no other symptoms.
In stage NYHA II there are already slight deficits in physical performance. While everything is normal at rest and under low stress, heavy exertion (e.g. climbing stairs or exercising) can lead to shortness of breath, angina pectoris (a feeling of tightness in the area behind the breastbone) or cardiac arrhythmias.
Patients in the NYHA III group do not have any complaints at rest, but they do have very little physical exertion such as walking on a straight plane.
NYHA IV-classifieds show the symptoms of angina pectoris, cardiac arrhythmias and shortness of breath even when completely at rest and are therefore bedridden.
diagnosis
The weak heart (Heart failure) is a widespread disease in industrialized nations.
It is therefore not surprising that to date a whole range of clinical tests have been developed to diagnose heart failure. Even the physical examination can give clear indications of the presence of the disease.
Particularly noticeable are blood congestion in the neck veins and water retention in the legs (Edema) and heart murmurs when listening with the stethoscope.
If abnormalities were discovered here or during the patient consultation, further tests can be carried out. The most important thing here is to identify the cause of the heart failure.
To avoid coronary artery disease (CHD), which can be viewed as a preliminary stage of a heart attack, for example, a stress ECG can be performed. For this purpose, an EKG is written while the patient drives on an ergometer with increasing resistance. Another test for CHD can be done using an MRI scan of the heart or cardiac angiography.
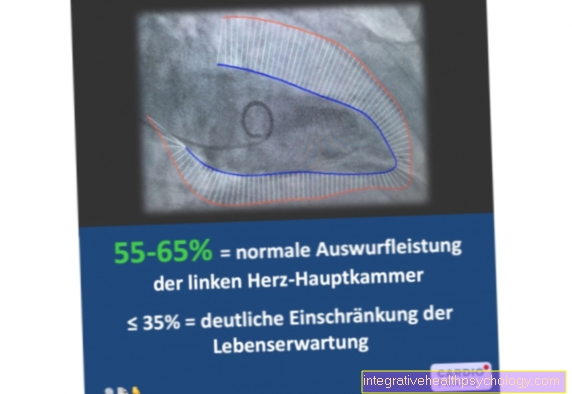
The standard heart examinations also include the heart echo (Echocardiography). This is basically nothing other than an ultrasound examination of the heart, in which the functionality of the heart muscle and the heart valves can be assessed very well.
Finally, laboratory diagnostics can also be used as a test for the severity of heart failure, or for its complications and causes. For this purpose, a test for the hormone BNP has been available for some years, which can be increased in heart failure and thus provides information about the stress on the heart.
Read more on the topic:
- EKG for heart failure
- These tests are done if you have heart failure
Heart failure and alcohol
As an integral part of western society, alcohol is an indispensable part of our everyday lives. The negative health effects on our body cannot be denied.
The heart muscle can also be affected by alcohol consumption. Most of the time, such toxic myocardial diseases, such as those that can arise from heavy drug and drug consumption, are the result of very intensive and regular alcohol consumption and are therefore rather rare. In general, however, many studies indicate that not drinking too much alcohol is not a cause of heart disease such as heart failure.
Some American studies even came to the conclusion that moderate alcohol consumption should even have a protective effect on the heart. However, these studies are far from undisputed and have been heavily criticized by many doctors for various reasons.
Apart from that, a critical look at your own alcohol consumption is definitely recommended in many ways. The recommendations of American Heart Association can be used. This recommends women not to consume more than 12 grams of alcohol per day (like a glass of wine, beer or schnapps), or 24 grams of alcohol a day for men (so two glasses of wine, beer or schnapps). In addition, even with a low risk of heart failure, alcohol still causes great damage to other organ systems such as the liver and should therefore only be consumed in small amounts, if at all.
Read more on this topic:
- Consequences of alcohol
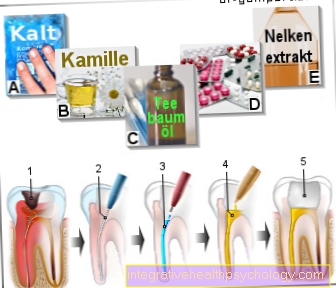
Treatment of heart failure
The treatment of heart failure is extensive and lengthy; the disease can only be cured with a heart transplant. The first step in treatment is always to eliminate its causes, whereby a lifestyle change is particularly important for the success of the therapy. For this, on the one hand, the blood pressure should be reduced to normal values (below 140/90) (please refer: Lower high blood pressure) and reduce body weight. In addition, physical activity is particularly recommended. Limiting the amount you drink daily and the amount of table salt you consume with your food can also be helpful.
Drug therapy for cardiac insufficiency involves a whole range of drugs that act directly or indirectly on the heart muscle and are intended to relieve it. The so-called beta blockers and ACE inhibitors are the most widespread. Dehydrating drugs (diuretics), which ensure that excess fluid is excreted with the urine, also relieve the heart muscle.
Finally, as a final option for treating heart failure or avoiding serious consequences, various surgical procedures are available depending on the cause of the heart failure. The implantation of a cardiac pacemaker, which is mainly used in the case of conduction disorders of the heart, is particularly widespread.
Read more on the topic:
- Therapy for heart failure












.jpg)