Symptoms of lumbar spine syndrome
introduction
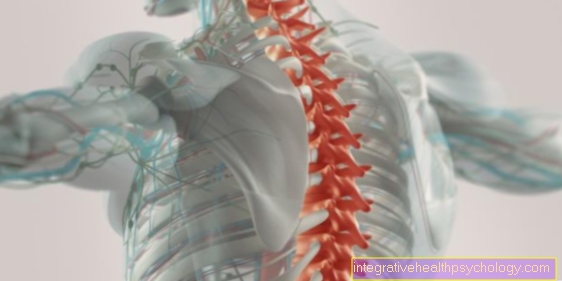
The lumbar spine syndrome is a clinical picture whose symptom complex primarily describes the back pain in the lumbar spine (lumbar spine) as the main symptom. Since it is a so-called lumbar spine "syndrome", it describes different symptoms that result from different causes. In the lumbar spine syndrome, for example, one can suffer from back pain in the lumbar spine and, on the other hand, complain about abdominal pain or pain radiating to the lower extremities.

Common symptoms of lumbar spine syndrome
The most common symptoms of lumbar spine syndrome are:
- Back pain
- Abnormal sensations such as numbness or tingling
- Tension
- Stomach pain or digestive problems
- Radiating pain
- Motor failures
The symptoms of a lumbar spine syndrome can also be divided into radicular symptoms, i.e. symptoms emanating from the nerve roots, and pseudoradicular symptoms, whereby the latter does not originate from the roots themselves and therefore usually no radiating pain or motor failures occur.
Appointment with a back specialist?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The spine is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
The treatment of the spine (e.g. herniated disc, facet syndrome, foramen stenosis, etc.) therefore requires a lot of experience.
I focus on a wide variety of diseases of the spine.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
Pain in a lumbar spine syndrome
Lumbar spine pain is a very common phenomenon in the population. It is estimated that around 80% of adults have suffered from it once or several times in their life. It is one of the most common reasons for incapacity for work and significantly increases the number of days absent due to illness. Men and women are affected equally often.
The pain is felt differently by many patients - everything is described from sharp, stabbing, suddenly occurring pain that makes movements impossible to chronic, rather dull pain sensations. The beginning of the pain can also look very different. In one case, the trigger can be a wrong movement or trauma and the pain can begin acute. Otherwise, permanent poor posture or age-related changes in the spine can cause a gradual onset. Acute pain is defined to last up to 4 weeks, subacute pain varies over a period of 4-12 weeks, and chronic pain is defined as pain that lasts longer than 12 weeks.
Back pain
The pain characteristics vary depending on where the pain originated: for example, bony and muscular structures can trigger back pain, but also ligaments, tendons or nerve irritation. With regard to the nerves, the lumbar spine syndrome can be classified into radicular and pseudoradicular pain make. Generally speaking, the localization of pain in a lumbar spine syndrome is related to the lower back area, i.e. the lumbar spine, and results from blockages, irritation or tension.
Radiating pain
Rarely does the pain radiate into the legs. The nature of the pain can vary between dull, pulling, non-stabbing and very strong intensities. Depending on the trigger, the pain can be sudden and short-lived, but it can also become chronic. The time course of the pain depends on the cause. The intensity of the pain can be negatively influenced by strain on the lumbar spine. An increase in pressure through violent coughing, sneezing or pressing can also increase the pain.
stomach pain
Many patients are not aware of the fact that abdominal and back pain can be related. However, especially when a lumbar spine syndrome is present, it is possible that abdominal pain may occur in addition to the characteristic back pain.
The reason for this can be, for example, that patients suffering from a lumbar spine syndrome adopt a relieving position in order to minimize the pain and relieve the back. In addition to tension in the back, this also results in problems in the muscular apparatus on the stomach and trunk. The muscles can be shortened or stretched unphysiologically due to the incorrect posture and then cause pain. So this means that back pain can often cause stomach pain.
In addition to the superficial, purely muscular abdominal pain, it is also important to consider abdominal pain with an organic cause. Due to the poor posture, various organs in the abdomen are narrowed or warped, so that the pain originates from the irritated organs. The radiation of the pain can then, depending on the position of the organ, be on the stomach, but also on the back.
Clearly defined clinical pictures such as the herniated disc and scoliosis, a disease in which the spine is deformed, can cause this phenomenon.
If the pain is particularly localized in the lower abdominal area, one should also always think of a so-called "vertebral sliding" of the lumbar vertebrae. The slipping change in position of the vertebral bodies has a great influence on the muscle and ligament structures of the spine. The pain is often projected into the abdominal region via the muscular system.
The causality chain of the pain can also be reversed, i.e. that pain emanating from the stomach radiates into the back. Then the suspicion can be wrongly raised that you are suffering from a lumbar spine syndrome, although the back pain is of an organic nature. An example of this is inflammation of the pancreas, which is located in the abdomen relatively close to the spine. Pain due to a condition called pancreatitis (Inflammation of the pancreas) can therefore pull in the back. For example, irritable bowel syndrome can cause the triad of symptoms: nausea, back pain and stomach pain. As soon as back pain and abdominal pain occur at the same time, in addition to the diagnosis for a lumbar spine syndrome, not only the back but also the abdomen should always be examined.
You might also be interested in this topic: What to do against stomach ache?
Neurological symptoms of lumbar spine syndrome
The spine is the bony armor of the spinal cord from which the nerve fibers originate, which organize themselves in bundles and then emerge as nerves and supply the individual areas of the body. If there are changes in the spine, even if it is only a brief tension in a muscle or swelling due to inflammation, this can irritate the nerves in their courses. The patient can then feel this through tingling, numbness, paralysis or pain, for example.
Of course, neurological symptoms such as an unfavorable sleeping position can also occur within a safe framework. In principle, sensory disorders that do not exist for a short time should always be clarified by a doctor. For example, you may have problems urinating or having difficulty holding urine or stool. These are clear warnings that should be taken to a hospital quickly for further diagnostic tests as early as possible.
Paresthesia
In addition to back pain, patients with a lumbar spine syndrome often suffer from abnormal sensations such as numbness or tingling sensations in the back and extremities. In most cases, back pain is accompanied by a relieving posture, which in turn provokes tension in the back muscles and restriction of movement.
As already mentioned, the radiation of pain is not particularly characteristic, as the pain is largely localized to the lumbar spine. Exceptions or variations are described in the following sections “Abdominal Pain”, “Radicular” and “Pseudoradicular”.
In general, the lumbar spine is very prone to injuries or discomfort compared to the other parts of the spine. This is due to the fact that the lumbar vertebrae are exposed to a great deal of pressure due to their location at the end of the spine. After all, the lumbar spine has to bear the weight of our entire torso. A herniated disc is therefore a typical clinical picture and occurs primarily in the lumbar vertebra area.
Read more about discomfort on our website: Does a tingling sensation indicate a herniated disc?
Radicular symptoms
Radicular pain is also described as projected pain and is based on the injury / pressure of nerve roots in the lumbar spine. This can be caused by a herniated disc in the lumbar spine.
The pain is therefore localized on the one hand on the back, but on the other hand it also radiates into the supply area of the damaged nerve. The radiation from the back can take place down to the lower leg. Among other things, this is a differentiation criterion for pseudoradicular pain, the character of which is usually limited to the thigh and cannot be clearly assigned to the supply area of a nerve in the lumbar spine.
Read more on this topic at: Symptoms of a herniated disc of the lumbar spine or Symptoms in the leg of a herniated disc in the lumbar spine
Also important for understanding these two types of pain is the fact that radicular pain is caused by the lesion of a nerve or its root. Because of this nervous component, one also speaks of neuropathic pain. As the name "radicular" suggests, in most cases the pain is caused by irritation of the nerve root (root = "radix“) Triggered.
This nerve irritation can be caused by a herniated disc in the lumbar spine. The prolapsed disc presses on the nerve root of a nerve emerging from the spinal canal at this point in the spine. This is accompanied by severe, stabbing pain.
The radicular pain in a so-called "nerve root syndrome", which falls into the symptom complex of the lumbar spine syndrome, can then pull the entire leg along the corresponding nerve course. Our thickest nerve, the sciatic nerve or sciatic nerve, is often affected.
In addition to the referred pain, depending on the degree of lesion of the nerve, sensory disturbances in the form of tingling or numbness can also occur. In the worst case, it can even lead to sensitive and motor failures. The reflexes can also be reduced or even fail completely due to a lumbar spine syndrome with radicular pain. Depending on the damaged nerve, those affected can also have problems with digestion or urination. Radicular pain also has a tendency to become chronic pain. Standing for a long time, but also strong coughing and straining, usually intensifies the radicular pain through increased pressure on the nerve root. Many patients experience a slight reduction in pain when they lie down or adopt a relieving posture, as this relieves the intervertebral discs. If you suffer from a lumbar spine syndrome with radicular pain, you can ultimately be very limited in your mobility and even the smallest everyday activities.
Read more on this topic at: Pseudoradicular pain
Pseudoradicular symptoms
In contrast to radicular pain, the radiation character of pseudoradicular pain is limited to the thigh at most. A main differentiation criterion is that the pseudoradicular pain is not caused by a nerve root lesion, but is only based on the irritation of the nervous structures. The nerve does not have to be damaged, but can cause temporary pain due to thermal, mechanical or electrical irritation. The pseudoradicular pain is therefore less of a pure nerve pain. The pain trigger is the irritation of the nerve and the resulting increased pain transmission and processing in the CNS. One speaks in comparison to the "neuropathic"And radicular pain here rather from a"nociceptive"Pain, because the pain receptors, so-called"Nociceptors“Be more excited.
The reason for pseudoradicular pain is often unclear, so "idiopathic". A possible cause of a lumbar spine syndrome with pseudoradicular pain, however, is irritation of the facet joint (Intervertebral joints) or other joints in the spine or hip area. Since the pain character of the two types of pain is very similar except for the type of radiation, the "pseudoradicular" pain can also be called "pretense“Interpreting a radicular pain.
Another important difference is that pseudoradicular pain does not lead to motor failures, but only to pain and possibly skin sensation disorders. The prognosis for pseudoradicular pain is better, as the pain can subside as soon as the pain-inducing stimulus disappears.