Symptoms in the leg with a herniated disc
introduction
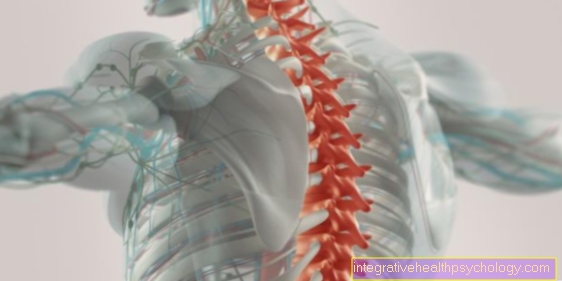
A herniated disc is a degenerative disease of the spine. Each disc consists of an outer fibrous ring and an inner gelatinous core. If the nucleus of the gel bulges slowly or suddenly outward due to degenerative changes and breaks through the fibrous ring, one speaks of a herniated disc (Prolapse).
A herniated disc is by far the most common in the lower lumbar spine, as this is where pressure forces and wear are greatest. Depending on the direction in which the core of the intervertebral disc bulges and which structures are compressed, typical symptoms occur.
In the case of a herniated disc in the lumbar spine, symptoms in the legs can occur in addition to severe back pain due to the compression of the associated nerve tracts. The reason for this is that the nerve fibers that supply the muscles of the legs with motor and the skin in a sensitive way emerge from the spinal cord at the level of the lumbar spine. Typical symptoms can include pain in the legs, numbness or tingling, or even paralysis.

Numbness and tingling in the leg
Sensory disturbances (sensory disturbances such as numbness or tingling) within an area of skin that is supplied by nerve fibers of a certain spinal column segment (dermatomes) are indicative of a herniated disc.
Similar to paralysis, sensory disturbances (tingling sensation) in the legs indicate a pronounced herniated disc, which should definitely be treated by a doctor in order to prevent permanent nerve damage.
Read more on the topic:
- Tingling sensation indicating a herniated disc
- Numbness indicating a herniated disc
and - Other causes of tingling in the legs
Paralysis in the leg
In the case of paralysis, a distinction is made between paresis (an incomplete reduction in strength) and plegia (complete paralysis).
If a herniated disc leads to compression of motor nerve fibers that enable muscle tension, this can lead to a reduction in strength and even paralysis of the legs. This is always a sign of a severe herniated disc and requires immediate medical attention. In such cases, surgery is often necessary to prevent permanent damage.
Only if there is really paralysis in the legs is it an absolute indication for surgery. However, extreme pain or numbness are only a relative indication for surgery.
If an operation is necessary, you will find further information on our website: OP of a herniated disc of the lumbar spine.
Also read: Symptoms of paralysis in the leg
The herniated disc in the lumbar spine can also trigger a so-called cauda equina syndrome, which should be recognized urgently and, if left untreated, can lead to permanent paraplegia. We therefore recommend our website for further information: Cauda equina syndrome - do I have paraplegia?
Appointment with a specialist for a herniated disc?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
A herniated disc is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
Therefore, treating a herniated disc requires a lot of experience.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
Pain in the leg
Back pain is a widespread disease and common "low back pain" (lumbago) is often behind the symptoms.
If the pain occurs suddenly and shooting in, this indicates a herniated disc. If there is pain in the legs at the same time, the suspicion is reinforced. Pain in the legs does not mean pulling in the thigh (as is the case with sciatica), but pain in the supply area of a certain nerve root.
The pain in the leg is often stronger than the pain in the back and radiates to the tip of the toe. Often the pain worsens when moving, sneezing or coughing, since the pressure conditions in the spinal canal change minimally.
Read more on the topic: Pain in the legs
Radicular pain
Radicular pain (from Radix = Root) start from one or more nerve roots in the area of the spine. They follow the course of the affected nerve and are felt in its individual supply area. The pain is often felt in the leg up to the tip of the foot.
In the case of a herniated disc, the nerve root can be irritated, so that the pain in the area supplied by the nerve (often the legs in the case of a herniated disc in the lumbar spine) is often felt more strongly than at the actual source of pain.
In some cases, the radicular pain is accompanied by other symptoms, such as tingling (Paresthesia) or paralysis (Paresis) accompanied.
In contrast to the rather unspecific pseudoradicular pain, radicular pain strongly suggests a herniated disc of the lumbar spine.
Next article might be helpful to you too: Disc herniation of L3 / L4
Pseudoradicular pain
Pseudoradicular pain is much more common than radicular pain and can often be confused with it. On closer inspection, however, it becomes apparent that pseudoradicular pain does not occur in the supply area of a particular nerve. The accompanying abnormal sensations also do not relate to a specific nerve area and symptoms of paralysis do not occur in connection with pseudoradicular pain.
For example, the cause of pseudoradicular pain can be in the small joints of the spine (Facet joints) or in the sacroiliac joint.
Pain right / left
Depending on the direction in which the gelatinous nucleus bulges, different structures are stimulated. If the gelatinous nucleus emerges backwards, it compresses the spinal cord and leads to the symptoms described.
Often, however, it does not exit straight back, but a little laterally to the left or right. Depending on whether the irritated structures (nerve roots, spinal nerves) are on the left or right side, failures occur on the respective side. These can manifest themselves in the form of pain, sensory disorders (tingling, numbness) or motor restrictions.
Loss of sensitivity of the dermatomes
A dermatome is an area of skin that is sensitively innervated by a specific spinal nerve (spinal cord nerve), which means that the skin sensation at this point is taken over by this specific spinal nerve.
If the spinal fibers are compressed in a herniated disc, sensitive failures occur in the segments they supply. If sensitive failures are limited to a specific dermatome, the localization of the herniated disc can be derived from this.
Disc herniations are common in the L4 / 5 (lumbar vertebrae 5) or L5 / S1 area, which lead to limited sensation of touching the inside of the lower leg and the foot.
Read more on the topic: Dermatome
Leg buckles
A herniated disc can damage one or more nerve roots and cause various symptoms in the leg.
If the L5 nerve root is affected, those affected can bend their knees when climbing stairs, for example.
Even with S1 syndrome, the leg can sag.
The two aforementioned nerve roots supply different muscles of the buttocks. These muscles, especially the gluteus medius muscle, which is supplied by the L5 nerve root, provide the pelvis with support when walking. If the muscles fail, gait difficulties arise.
Tingling in the legs
A common symptom of a herniated disc in the lower spine is sensory disorders in the leg and foot. Many sick people suffer from sensory disorders such as tingling or pins and needles. This is a subjective discomfort that is perceived by those affected as extremely unpleasant and annoying.
Read more about the symptom here: Does a tingling sensation indicate a herniated disc?
L5 syndrome
L5 syndrome is a root compression syndrome in which the nerve root on the 5th lumbar vertebra is irritated or injured. It is a common syndrome due to the localization typical of a herniated disc.
The L5 nerve root, which runs between the fifth lumbar vertebra and the first sacral vertebra, is damaged. There is either a protrusion of the intervertebral disc or even an exit of the gelatinous nucleus from the fibrous ring, which compresses the nerve root.
L5 syndrome can cause the following characteristic complaints in the leg:
Sensitive disorders
- This includes pain that can range from the back of the thigh to the outer knee, the front and sides of the lower leg, to the dorsum of the foot and to the big toes.
- In addition to pain, there may be sensory disorders such as tingling, pins and needles or numbness in the affected area.
Motor disorders
In addition, motor nerve fibers of the L5 nerve root can be damaged. The consequences are paralysis. These become noticeable in the affected person as a restriction in the hip joint and weak foot. Muscles such as the gluteus medius, extensor hallucis longus, and tibialis anterior muscles can be affected. It is not possible to lift the feet and toes and the patients have a noticeable, restricted gait pattern. The sick are unable to go into a hoe walk.
Read more on this topic at:
- L5 syndrome
S1 syndrome
A root compression syndrome that irritates or damages the S1 nerve root is known as S1 syndrome. A herniated disc at the level of the fifth lumbar vertebrae and the first sacral vertebrae can damage both the L5 and S1 nerve roots. Both or one of the two structures can be damaged. Both a simple protrusion of the intervertebral disc and an emergence of the gelatinous nucleus from the fibrous ring of the intervertebral disc can be the cause of a herniated disc with S1 syndrome.
Typical symptoms are pain
- in the lower back
- in the buttock region,
- in the back of the thigh
- in the lower leg,
- in the heel
- as well as on the lateral edge of the foot up to the little toe.
The pain can suddenly shoot in and radiate. The areas mentioned can also be affected by abnormal sensations. Tingling, pins and needles and numbness are common. In addition, certain muscles can be paralyzed. Buttocks muscles (gluteus maximus muscles), calf muscles (trizeps surae muscles), and biceps femoris muscles on the back of the thigh can be affected. Sufferers have difficulty moving their hips and cannot lower their feet.
Toe walking is weakened or impossible.
Find out more about the topic on the main page: S1 syndrome.
Pain in the buttocks and legs
Pain in the buttocks and legs are common complaints in our society.
A herniated disc in the L5 and S1 vertebral bodies is a possible cause of pain in the buttocks and legs. In this case, the pain mainly occurs in stressful situations.
In addition, muscle tension in the buttocks area comes into question, which occurs particularly in people who sit a lot, for example when doing an office job.
In addition, narrowing the spinal canal can lead to pain in the affected areas.
Pain in leg and foot
Pain in the leg and foot occurs in both L5 syndrome and S1 syndrome. The pain localizations differ depending on the damaged nerve root. The pain often occurs during physical exertion and can be shooting in and radiating.
L5 syndrome causes pain
- in the back and side thighs,
- on the outside of the knee,
- on the front, lateral lower leg,
- as well as on the back of the foot and big toe.
The pain associated with S1 syndrome is typically affecting
- the outside and back of the thigh and lower leg,
- the side of the foot
- and the little toe.