Deafness - impaired sensation
Definition

A sensitivity disturbance is a temporary irritation or permanent damage to the nerve. This leads to misdirected sensations in the event of external irritation of the body of the person concerned.
Just as there can be a wide variety of causes for the sensitivity disorder to develop, there are a large number of forms of the sensitivity disorder. That is why the diagnoses and thus the treatment options are very diverse.
Unfortunately, there is no prophylaxis (prevention) against sensory disorders that is guaranteed to prevent deafness.
A sensitivity disturbance leads to a changed perception of external stimuli. This disorder is caused by a change in the nerves.
Forms of sensitivity disorder
There are seven different stimuli:
- Sense of touch
- Temperature sensation
- Vibration sensation
- Sensation of pain
- Sensation of movement
- Sense of position
- Feeling of strength
If there is now a sensitivity disorder, these stimuli are either uncomfortable or even painful (so-called Dysesthesia), stronger (at the Hyperesthesia) or weaker (for the Hypesthesia) than otherwise perceived. A complete sensory disturbance is also possible, so that the stimulus cannot be perceived at all (anesthesia).
Another form of sensitivity disorder is the Paraesthesia in which the sensation is present but has not been triggered by a corresponding stimulus. In general, this is known from the harmless case when your arm or leg has "fallen asleep", so you can feel "ants running" over the area, although nothing is walking along it.
You may feel numb as the disease progresses. This means that the skin does not transmit any mechanical stimuli or pain sensations. For example, the face, individual limbs or the auricle may be affected.
Learn more at: Numbness in the ear - what's behind it?
Sensitivity disorders that last longer than a "leg / arm that fell asleep" should generally be taken very seriously, as they can have far-reaching consequences. If the person concerned is in anesthesia, i.e. a lack of pain sensation, it can happen that an accidental injury is not noticed and therefore cannot be adequately cared for. Bleeding to death, infection of the wound and so in the long term "mutilation" are possible consequences.
causes
A sensory disorder is triggered by a functional disorder of the nerves, so the cause of this disorder must also be sought in the area of nerve function.
In migraines, there is often a temporary irritation of the nerves. Further limitations of the regular nerve function can be circulatory disorders (for example, as a slight variant of the "asleep arm"), the infestation by viruses (for example herpes viruses) or treatment with drugs that lead to permanent nerve damage.
Possible causes of circulatory disorders that can then lead to nerve damage include the following:
- Burns
- stroke
- diabetes
- Tumors (especially in the brain and spinal cord)
- neurological diseases (e.g. Parkinson's or multiple sclerosis)
General illnesses that can lead to sensitivity disorders are:
- Herniated disc ->
Read also unset topic: Is numbness a sign of a herniated disc? - Circulatory disorders
- Pinched nerve
- Alcohol abuse
Find out all about the topic here: The sensory disturbances.
Diagnosis and course
Holds a Sensory disturbance a medical examination must be carried out urgently. This is the only way to determine whether it is a temporary nerve irritation or a serious illness that needs treatment.
The responsible specialist is called neurologist and first interviewed the patient in the so-called Anamnesis interview according to the exact sensations and observations. In this way, he can find out since when the symptoms have been present and whether possible causes are already known. Previous illnesses, previous operations, family illnesses and regular medication are also asked about.
In addition, a physical examinationsg performed and a blood sample examined in the laboratory. In addition, the neurological examination (reflexes, temperature sensation, pain sensation, etc.) is carried out.
In addition, further examinations can help to determine:
- Magnetic resonance imaging,
- Computed Tomography,
- Cerebral fluid examination
- Allergy test
treatment
A sensitivity disorder will be consistent with her root cause treated.
If a nerve is pinched, it has to go through massage, gymnastic exercises or surgery to get relief from symptoms.
If there is dysesthesia or hyperesthesia, it may be advisable to use pain relievers Medication to reduce the normal stimuli perceived as pain.
Treatment is possible with Antidepressantswhich often help to improve symptoms.
If there is a stroke, it must be done immediately intensive care intervened. Otherwise, permanent damage or even death can result.
Is the sensitivity disorder called side effect If a drug is observed, the drug in question must be discontinued under medical supervision.
When bacteria become a infection have caused irritation of the nerves with the following impairment of sensitivity, the person concerned must as soon as possible antibiotic be treated.
It can also be harder Alcohol abuse lead to sensory disorders. Here is a withdrawal treatment, as well as an accompanying intake of Vitamin B1 recommended to avoid the progressive destruction of Nerve fibers to stop.
At Diabetics Regular monitoring of blood sugar levels is necessary so that they are kept within a healthy range. In addition, the ingestion of Alpha lipoic acid helpful.
In most cases it is not possible to go for a permanent one if there are persistent sensory disturbances Taking medication to renounce
prevention
A real one prevention Unfortunately there is no against sensory disorders. Generally one can say that a balanced nutrition and the adequate supply of Vitamins and Minerals contributes to keeping the nerves healthy.
Much Move, avoidance of stress and well-fitting clothes / shoes can also reduce the risk of nerve disorders.
Physiotherapeutic Treatments can also help prevent sensory disorders in the long term.
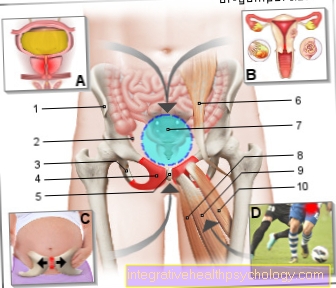
Dermatomes
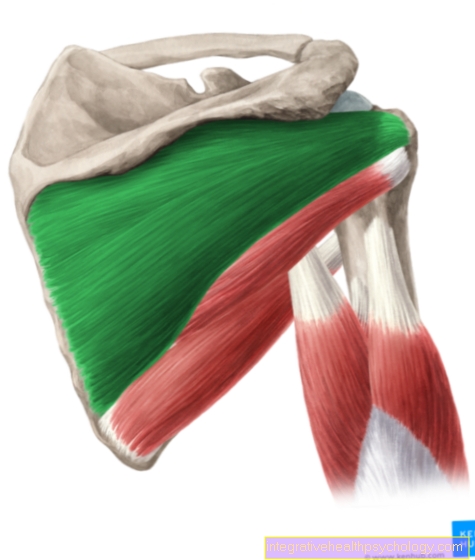
A dermatome is an area of skin that is supplied and controlled solely by the nerve fibers of a particular spinal cord root (spinal nerve root).
The term “dermatome” comes from the Greek and is made up of the two words skin and section. In medicine, knowledge of the dermatomes is very important, especially when there is a loss of sensitivity.
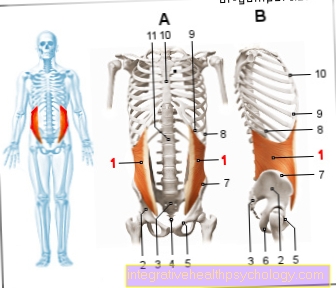
Classification of dermatomes:
An embryo has three so-called cotyledons (Ectoderm, Mesoderm, Endoderm), from which the various types of tissue develop in the course of maturation.
In the area of the trunk, the "primordial vertebrae" form from the mesoderm on the side of the neural tube (Somites).
The subcutaneous tissue and the skin are ultimately formed from the posterior-posterior portion of these somites. This results in a 1: 1 assignment of a spinal nerve to a specific skin area. For this reason, the corresponding dermatomes are also named after the nerves that supply them.
In the area of the cervical vertebrae there are eight spinal nerves, which are designated as C1 to C8, and this is also how the associated dermatomes are named.
However, with one exception: Dermatome C1 does not exist because the spinal nerve fiber of the first cervical vertebra has only motor and no sensory functions.
The trunk vertebrae have twelve spinal nerves and also twelve dermatomes, which are called Th1 to Th12.
Lumbar and sacral vertebrae each have five spinal nerves, so that the dermatomes are called L1 to L5 and S1 to S5.
These assignments are already established in the unborn child and remain in place in the adult. It is easier to classify the association of the spinal nerve and dermatome if one imagines the person bent over (i.e. in his most original, animal-oriented position) so that arms and legs are at 90 degrees. Point the angle from your back towards the ground. The body can then be divided into strips from which the dermatomes can be read. It starts with the dermatome C2 on the head and ends with the dermatome S5 on the back of the buttocks.
also read: Numbness of the head and scalp, numbness of the arm
Sensitivity in the dermatomes
The Dermatomes are not separated from each other by clear lines on the body, but a partial one occurs overlap. It is assumed that this overlap is more pronounced in the sensation of touch stimuli than in the sensation of pain or temperature.
So it is often the case with patients that the failure of one Spinal nerve remains unnoticed for the time being, as the adjacent spinal nerves continue to supply the affected dermatome. If two adjacent segments fail, the Sensory disturbance but mostly clearly noticeable.
In addition to the dermatomes, there are also so-called on the skin Autonomous areas. These are supply areas of certain nerves remote from the body center that are not spinal nerves.
Transmission from internal organs
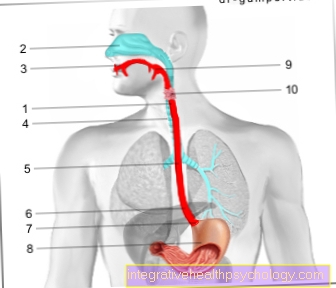
Just like the skin, so are the internal organs partly supplied by the spinal nerves. This is how it works brain sometimes not to assign received signals of a perception exactly to the place of origin. So it happens with one Heart attack also to the typical painful radiation in the left arm (dermatome Th1-Th5). If the liver or the biliary tract causes pain in the dermatomes Th6 - Th9 (right). In this way, almost every organ gets involved Skin area assign.
In some cases, the pain is not limited to just one dermatome, but spreads to adjacent areas or even affects an entire half of the body (Generalization). This process is called referred pain and can be an important feature in making a diagnosis.
Herniated disc as a cause of numbness
The dermatomes are of particular importance in the diagnosis of Herniated discs.
The jelly-like core of the intervertebral disc has slipped out here and presses on a spinal nerve fiber so that it is in the associated segments and Dermatomes malfunctions and failures occur.
By localizing the exact sensitive failure in a particular one Dermatome the exact amount of the herniated disc can be assigned.
Usually it lies Herniated disc in the L4 / 5 area so that there is a reduced sensation of touch on the inside of the lower leg and the foot. Is the In contrast, the herniated disc is in the L5 / S1 area, so it comes to sensitivity disorders on the outside of the foot and on the sole of the foot.