Therapy of a lumbar spine syndrome
introduction
What many patients do not know is that even in the acute phase of a herniated disc of the lumbar spine, physiotherapeutic applications can bring about significant symptom relief.
Physiotherapeutic treatment for a slipped disc of the lumbar spine is primarily based on the patient's current symptoms and the phase of the disease. During the acute phase of the lumbar spine syndrome, the physiotherapist's main focus should be on rapid pain relief. The characteristic pain associated with a herniated disc is caused by the fact that the damaged disc structure exerts pressure on the nerve root emerging from the intervertebral hole of the spine. In the context of physiotherapy, an attempt is first made to reduce this pressure through targeted positioning, mobilization techniques and manual therapy techniques.
You might also be interested in: Lumbar spine syndrome symptoms and exercises after a herniated disc of the lumbar spine

Therapy of a lumbar spine syndrome
The patient lies on his back, the legs are placed on a foam cube, the hip and knee joints should have an approximately 90 ° angle.
The angle of the legs can also be varied individually, depending on the most comfortable position. With a lumbar spine syndrome, some patients prefer a slightly flatter position in which they can wear a blanket or something similar. place under the lower legs. The lying surface should be rather hard. The goal is through this delordosed (the hollow back balancing) Positioning to relieve the lumbar spine and the intervertebral holes (Neuroforamen) to expand for the distressed nerve roots. This positioning can be supplemented well with a local application of heat by placing a flat warm pack, a hot water bottle or a warm towel under the lumbar spine without naturally reaching a new hollow back position. This positioning is very suitable for self-treatment at home in the acute pain phase of the lumbar spine syndrome.
Appointment with a back specialist?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The spine is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
The treatment of the spine (e.g. herniated disc, facet syndrome, foramen stenosis, etc.) therefore requires a lot of experience.
I focus on a wide variety of diseases of the spine.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
The sling table
An even more effective positioning position for a lumbar spine syndrome, which in principle uses the same effect as the step bed positioning, is the pelvic-leg suspension in the so-called sling table.Sling table treatment is primarily offered by physiotherapy practices or physiotherapy departments in clinics. In this special device, the pelvis and legs are fixed in special belt systems and aligned in the position described above. The loop construction simulates a certain "weightlessness" and the relief for the intervertebral disc structures often brings a considerable improvement in the symptoms.
Traction treatment
Another effective physiotherapeutic treatment method for the herniated disc (Prolapse) is the traction treatment (Stretching treatment). A pull is carried out in the longitudinal direction of the spine manually (by the physiotherapist / physiotherapist) or in the sling table using an additional weight. With this dosed pull one tries to pull the vertebral bodies apart minimally and to relieve the affected intervertebral discs and nerve roots. However, this therapy of the lumbar spine syndrome should only be carried out by a qualified therapist who can adjust the intensity of the traction to the respective situation.
Physical therapy
Of the physical therapy measures of the lumbar spine syndrome, heat applications promise (Thermotherapy) in the acute phase a symptom relief, as the action of a mud pack or other warming media relaxes the often painfully cramped muscles. Massage therapy is often not recommended in the acute phase of a herniated disc, as intensive grip techniques can cause additional irritation of the affected nerve structures. Furthermore, the possibilities of traditional Chinese medicine (TCM) can of course be exhausted. The best-known sub-area of TCM is certainly acupuncture, but moxa therapy (burning off medicinal herbs on acupuncture points) or foot reflex zone therapy can also be used successfully.
Physiotherapy treatment of a herniated disc in the cervical spine in the acute phase is very similar to physiotherapy for the cervical spine syndrome.
Muscle training
In the subacute (the strongest, immobilizing pain is overcome) phase of the lumbar spine syndrome / herniated disc, one of the most important aspects of physiotherapy treatment is targeted training of the core muscles (abdominal and back muscles). The therapy methods mentioned above and also the medical treatment are primarily symptom-oriented.
A long-lasting and preventive therapeutic effect, on the other hand, can only be achieved through well-carried out muscle building training and by learning about back-friendly everyday behavior. While in recent years great emphasis has been placed on training the back and abdominal muscles, a trend reversal has recently emerged. Newer concepts neglect the aspect of abdominal muscle training more and more and clearly focus on training the back muscles. It also makes sense to practice the rotational movements of the spine after a herniated disc (at a certain time interval). However, more complex exercises, such as the rotational component of the spine, should only be carried out under professional guidance in a physiotherapeutic practice or a fitness studio with physiotherapeutic supervision, since incorrect training can cause more damage than good. Training with free weights (dumbbells) is also coming back to the fore.
Simpler, but still effective exercises can, however, be carried out at home even without extensive specialist knowledge and equipment. For example, exercises in the quadruped position are very well suited to efficiently strengthen the entire back muscles. It is primarily important to ensure that you are in a good starting position. The entire spine should be muscularly stabilized in order to avoid evasive movements.
Manual therapy
Another important clinical picture, which very often leads to an acute lumbar spine syndrome, is the "blockage" of one or more vertebral joints. A blockage, known in medical parlance as segmental articular dysfunction, describes a temporary movement disorder of a joint. Classically, patients with an acute blockage of a vertebral joint report a sudden, lumbago-like back pain, which leads to the immediate abandonment of any activity. Movements are hardly or not at all possible. The cause of such blockages is often a jerky lifting of heavy objects, but sometimes simply an unfavorable movement in a stooped position. In a very short time, the surrounding lumbar spine muscles tense up enormously, as an expression of the fact that the body is trying to immobilize the pain-causing movement segment (the blocked vertebral joint). However, blockages can also be less dramatic. The patients then complain of unspecific back pain or have the feeling that they are “somehow crooked”.
Therapeutic treatment methods aim to restore the physiological (natural) joint play and to free the blocked vertebral body from its predicament.
The most commonly used treatment techniques to achieve this goal are manipulation techniques and mobilization techniques. Both techniques are part of manual therapy. With the manipulation techniques, targeted, fast impulses are placed in the area of the blockage. In the population, this technique is understood as the classic “straightening”.
The mobilization techniques are muscle energy techniques that work without rapid impulses and use the patient's own muscle strength to free the blocked vertebral joint.
“Adjusting a blocked spine” is reserved for doctors with special additional training (chiropractic / manual therapy) in Germany. Mobilization techniques are carried out by doctors and physiotherapists who are trained in manual therapy, due to the lower risk of complications. Both techniques are equally well suited to releasing a blockage when used properly.
Read more on the topic: Adjust vertebrae
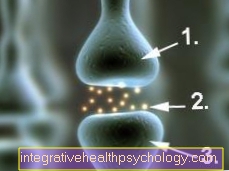
acupuncture
Back problems, as they often occur in the lumbar spine syndrome, often arise from tension in the muscles, incorrect loading of the spine or due to pathological changes in the small vertebral joints. In addition to conservative therapy (e.g. the administration of pain reliever and muscle-relaxing medication), acupuncture is another, non-surgical way to alleviate the symptoms. Special needles are inserted into certain acupuncture points (meridians) by a doctor or alternative practitioner trained in natural history. They remain there for about 20 to a maximum of 30 minutes. The patient feels a slight tingling sensation or sensation of warmth during the treatment. The aim of acupuncture is to activate and stimulate the flow of energy, the blood circulation in the affected body regions and the body's self-healing powers. Symptoms are often improved after just a few sessions.
NSM neurostimulation represents a new treatment method. Fine probes, similar to acupuncture needles, are inserted into the diseased tissue. An electric field is now applied between these, which is generated by a special stimulation device. This is intended to neutralize substances that trigger pain and inflammation, while at the same time directing important cells for wound healing to the site of damage. The treatment is completely painless for the patient and, according to previous knowledge, can have an anti-inflammatory and regenerative effect.
Read more about this: Acupuncture for back pain
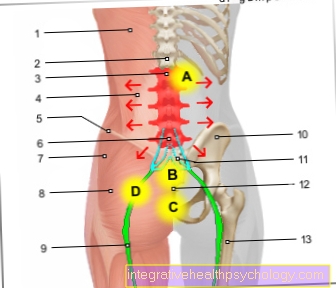
- Broad back muscle -
M. latissimus dorsi - Twelfth thoracic vertebra -
Vertebra thoracica XII - First lumbar vertebra -
Vertebra lumbalis I - Broad back muscle -
M. latissimus dorsi - Iliac crest -
Iliac crest - Fifth lumbar vertebra -
Vertebra lumbalis V - Gluteus Middle -
M. gluteus medius - Gluteus Muscle -
Gluteus maximus muscle - Sciatic nerve -
Sciatic nerve - Iliac scoop -
Ala ossis ilii - Lumbar sacrum nerve plexus -
Lumbosacral plexus - Tailbone -
Os coccygis - Femoral shaft -
Corpus femoris
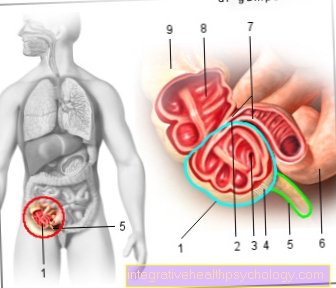
A. - pancreas
B. - Uterus
C. - urinary bladder
D. - Sciatic nerve
You can find an overview of all Dr-Gumpert images at: medical illustrations


















.jpg)