Thoracic outlet syndrome
definition

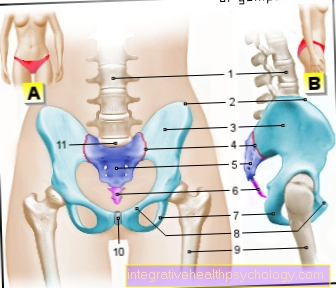
Thoracic outlet syndrome is an umbrella term for a number of diseases, all of which cause vascular and nerve compression in the upper chest area. The thoracic outlet syndrome is often also called bottleneck syndrome of the upper thoracic opening or shoulder girdle compression syndrome. The thoracic outlet syndrome leads to acute, temporary or chronic, long-term crushing of the vascular nerve bundle that runs in this area. Affected anatomical structures are the brachial plexus nerve bundle and the clavicle vein and artery.
causes
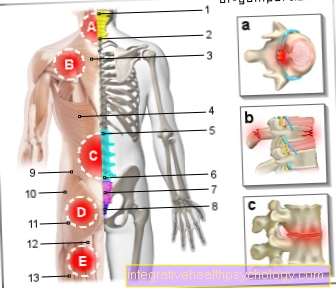
The Thoracic outlet syndrome has a whole host of different causes. These differ depending on where the vascular nerve bundle is pinched. The subgroups of the thoracic outlet syndrome then each have the appropriate name for the bottleneck. The vascular nerve bundle runs as a unit from the neck towards the arms to supply them. This bundle has to overcome three bottlenecks that pose a risk of entrapment.
The first bottleneck is the so-called Scalene gap educated. This gap is on the side of the neck and is formed by two muscles. A narrowing at this point can be caused by a significant increase in the muscles and an additional rib in this area, which is then called the cervical rib. The associated bottleneck syndrome will Scale syndrome called.
The second constriction through which the neurovascular bundle runs is located behind the collarbone. The bundle runs between the back of the collarbone and the front of the ribs located there. If, due to a broken collarbone or a rib fracture, excessive new bone formation occurs at this point, it will callus called, the bottleneck there is also narrower. The associated disease will Costoclavicular Syndrome called.
The third large subgroup of thoracic outlet syndrome is hyperabduction syndrome. It arises at the third constriction and is caused by an excessively trained and therefore too large pectoral muscle (M. pectoralis minor).
Symptoms
Thoracic outlet syndrome causes numerous symptoms because not only are nerves compressed, as is the case with the classic carpal tunnel syndrome, but arteries and veins are also narrowed. Which symptom of the thoracic outlet syndrome is in the foreground depends primarily on which of the three structures is most compressed.
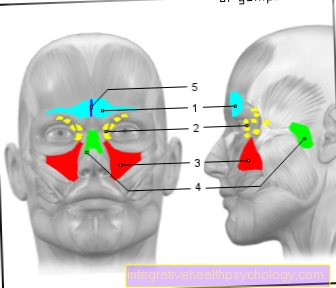
A major symptom of Thoracic Outlet Syndrome are above all Pain on exercise. These can affect the shoulder as well as the entire arm, mainly extending to the side of the ulna. By squeezing the nerves, not only pain but also discomfort in the hand can occur. As a maximum form, such a bruising can lead to a lack of emotional perception. Furthermore, abnormal sensations of the hands, which are perceived as "ant walking" or "falling asleep", can occur, especially at night. In addition to abnormal sensations, the fingers can get cold and there can be increased sweat production in the affected area. In severe cases, weakness and regression of the thumb muscles can ultimately result.
The constant pressure damage to the nerves can lead to a disorder of fine motor skills in the course of the thoracic outlet syndrome, making it difficult for the affected patient to write on a computer keyboard or play the piano. All of these symptoms are associated with damage to the nerves. If, in the case of thoracic outlet syndrome, the clavicle artery in particular is compressed and the blood flow to the arm is hindered, other symptoms are in the foreground. This compression works mostly with one Feeling cold, one possible Weak pulse up to a lack of pulse. But also rapid fatigue when working with the hands or when working overhead, such as painting the ceiling or combing, can be an indication of a thoracic outlet syndrome.
Blood pressure
If, as part of the thoracic outlet syndrome, it is primarily the arterial vessel that is compressed, blood pressure on the affected arm may be lower than on the healthy side. However, if the thoracic outlet syndrome only results in compression of the nerves or veins, then the blood pressure in the affected arm does not change.
diagnosis
The patient's symptoms are an initial indication of the diagnosis. These symptoms can usually be used to make an initial suspected diagnosis. In addition, an X-ray of the chest and possibly the cervical spine is made. A bony structure responsible for the symptoms, such as a cervical rib, can be found or excluded on this X-ray. Since the nerves of the arm can also be affected in the thoracic outlet syndrome, damage can be confirmed or excluded by measuring the nerve conduction velocity. The nerve conduction velocity is measured primarily in the area of the ulnar nerve (ellen nerve) and the median nerve (central nerve). In addition, there are some manual tests as part of the diagnosis of thoracic outlet syndrome, which can provide important information for confirming the diagnosis. In addition, other imaging methods can be used to identify constrictions and possible causes.
test
As part of the diagnosis of thoracic outlet syndrome, there are some test examinations that can cause the symptoms or worsening of the symptoms. Among other things, the so-called Adson test for use. The patient turns his head in the direction of the affected arm up to his limit of motion or pain. At the same time, the radial pulse is felt on the wrist. In the case of a pathological narrowing, this becomes significantly weaker in the test. Another test is the so-called Roos test, in which the patient raises his arms at an angle, so he puts his "hands up" and tries to close both fists. This test can provoke or intensify pain.
MRI
MRI also plays an important role in the diagnosis of thoracic outlet syndrome. Here, too, as in the context of X-ray diagnostics, possible bone changes can be shown. In addition, changes in the soft tissue can be shown by MRI, which may cause constrictions. Vessels and vessel changes such as enlargements or constrictions can also be displayed here. This procedure is then known as MR angiography. Contrast media containing gadoline is used here.
Angiography
Even the "normal" Angiography can be used to visualize vascular changes in the context of the thoracic outlet syndrome. A catheter is advanced in the direction of the clavicular artery through a vascular access in the groin in order to expose the desired area. In "normal" angiography, in contrast to MR angiography, a contrast medium containing iodine is used. Another difference is in the extent of the Radiation exposure. Standard angiography is performed using X-rays. In angiography by means of MRT, however, the images are generated using a magnetic field. As part of the examination using angiography, the affected arm is brought into a "provocation position" in order to induce possible narrowing of the vessels.
Read more about the topic here Angiography
Appointment with ?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
In order to be able to treat successfully in orthopedics, a thorough examination, diagnosis and a medical history are required.
In our very economic world in particular, there is too little time to thoroughly grasp the complex diseases of orthopedics and thus initiate targeted treatment.
I don't want to join the ranks of "quick knife pullers".
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You will find me:
- Lumedis - orthopedic surgeons
Kaiserstrasse 14
60311 Frankfurt am Main
You can make an appointment here.
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
For more information about myself, see Lumedis - Orthopedists.
therapy
There are two treatment options for thoracic outlet syndrome. On the one hand there is the conservative, non-operative variant and on the other hand the possibility of an operation. The conservative option consists of physiotherapy exercises the affected area and the use of medication. In the bottleneck syndrome, painkillers from the group of non-steroidal anti-inflammatory drugs (NSAIDs) such as diclofenac or ibuprofen are mainly used. They are intended to relieve the pain that is present and at the same time have a positive influence on any inflammation that may be present. Muscle relaxing medication can also be used if you suspect that the bottleneck is caused by a possible overload or tension in a muscle. The application of cold or heat may also help relieve symptoms.
Which doctor treats this?
Typically, patients with thoracic outlet syndrome are referred by their general practitioner to a neurologist, orthopedic surgeon, or vascular surgeon. The vascular surgeon is the specialist who, at the latest when conservative treatment fails, is an expert in thoracic outlet syndrome to advise and carry out surgical therapy. It is important that the person concerned is prescribed early physiotherapy treatment.
physical therapy
Mild symptoms of thoracic outlet syndrome are usually treated first with physiotherapy. This treatment leads to a relief of the symptoms in about 60% of the sick.
Exercises
There are some exercises you can do to strengthen your shoulders and neck muscles as part of a thoracic outlet syndrome. Basically, you should have experienced physiotherapists show you individually suitable exercises and practice them first under the supervision of the physiotherapist.
-
The patient stands with his arms hanging down. He is holding a weight in his hands (e.g. 1 kg, a water bottle is also possible). The patient shrugs his shoulders forwards and upwards about 10 times and then lets the muscles relax. Then he shrugs his shoulders backwards and upwards, about 10 times, and lets the muscles relax. Finally he shrugs his shoulders upwards / upwards for 10 pulls and relaxes the muscles.
-
The patient stands upright and extends his arms sideways at shoulder height. He is holding a 1 kilogram weight in both hands and the palms are facing down. The exercise consists of lifting your arms sideways until the backs of your hands touch above your head while keeping your arms straight. The exercise is also repeated ten times.
-
The patient stands straight with his arms sideways and flexes his neck to the left, trying to rest his left ear against his left shoulder. The shoulder is not raised. Do the same on the right side and each side for ten attempts in total.
-
The patient lies on their back with their arms to one side. A rolled up blanket or pillow is placed between the shoulder blades, but no pillow under the head. In this exercise, the patient takes a slow deep breath and raises his arms. The whole thing is repeated five to twenty times.
The muscles should be relaxed between all exercises and whenever you feel like doing it. You can take as many breaks as you want from these exercises.
surgery
Surgery is indicated for thoracic outlet syndrome when conservative treatment methods fail. This means that you have to operate if pure physical therapy is no longer sufficient to effectively relieve the symptoms. Then the constricting structure is surgically removed, often the cervical rib and first rib. Occasionally the pectoralis minor muscle is surgically cut to stop the constriction.
In particular, persistent pain, severe nocturnal pain, as well as changes in the clavicular artery or vascular occlusions require surgical therapy. Furthermore, nerve damage should be treated surgically in order to repair it.
Rehab
Rehabilitation is usually not necessary after surgery for thoracic outlet syndrome.
What is the prognosis?
With conservative treatment with physiotherapy, the prognosis for thoracic outlet syndrome is usually very good. If this treatment is unsuccessful, the sick are operated on. About 40 to 80% of the operated patients achieve an improvement in their symptoms. This means that some of the sick people have permanent symptoms.