thrombosis
Synonyms in a broader sense
- Deep vein thrombosis (DVT)
- Phlebothrombosis
- venous thrombosis
- Pelvic vein thrombosis
- Venous thrombosis
- Blood clots
- Leg vein thrombosis
- Lower leg thrombosis
- Economy class syndrome
- Tourist class syndrome
- Aircraft thrombosis
English: deep venous thrombosis

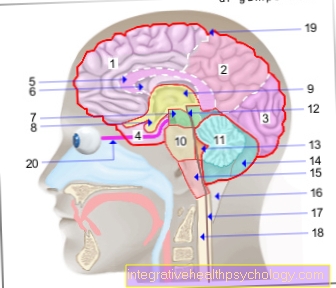
Definition of thrombosis
Under one thrombosis means the clotting of the blood (clot formation) in the blood vessel system, which leads to a blood clot (thrombus) With constipation of the blood vessel. As a result, the blood circulation is disturbed and blood congestion before the closure is the result. Thrombosis comes from the Greek word “thrombosis”, which means “curdling”.
Read more about the topic here: Blood clotting
Cause and origin
The from Rudolf Virchow The triad described in 1856 (Virchow's triad) for the development of a thrombosis are still unrestricted today.
In his triad he described three main causes for the development:
1. Slowing down the blood flow
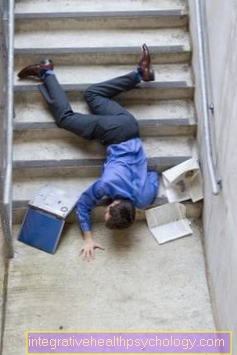
A slowdown or standstill in blood flow occurs naturally when there is a lack of exercise or a blockage of blood paths, e.g. by bending the knee joints for a long time during long-distance flights (long-distance thrombosis, travel thrombosis).
Insufficient blood circulation also occurs after surgical interventions. The postoperative bed rest results in insufficient activation of the muscle pumps in the calf muscles. When walking, the calf muscles tense and thus empty the venous vessels, thus preventing the formation of thrombosis.
The postoperative bed rest leads to an increased blood arrest - the risk for one thrombosis increases.
The operation of the artificial knee joint is considered to be a high risk patient for a thrombosis, artificial hip joint, Prostate surgery and operations on the lung.
2. Change in the composition of the blood
The composition of the blood changes daily with the increase in fluid. The proportion of fluid to blood cells is approx. 50:50. A lack of fluids leads to a shift in the ratio in favor of the blood cells (e.g. due to profuse sweating or insufficient fluid gain). This thickens the blood. The Risk of thrombosis increases.
After surgery, the body reacts to blood loss with an increased tendency to clot in order to limit blood loss. The consequence is that the Tendency to thrombosis also increases.
3. Change / damage to the vessel wall
Changes / damage to the vascular wall occur particularly in the arterial vascular system. As part of the aging process, increasing vascular calcification (arteriosclerosis) occurs. If this vascular calcification breaks out, a thrombosis immediately forms over the vascular defect. In the area of the coronary arteries, the area behind the thrombosis is no longer supplied with blood and a heart attack occurs. But inflammation of the vascular wall can also lead to inflammation.
localization

The deep veins in the legs (2/3 of all thromboses)> pelvic veins are most frequently affected.
Veins are particularly often affected because of the slow blood flow. Thrombosis of the veins is also called phlebothrombosis.
Other locations are the atrium of the heart, especially if there is atrial fibrillation.
Thrombosis can also occur in the eye.
Read more about this at: Thrombosis in the eye.
Causes / Risk Factors
There are many risk factors that increase the risk of thrombosis. It is precisely the combination of different risk factors that increases the risk.
As safe risk factors be valid:
- Operations (esp. artificial hip joint and artificial knee joint)
- Obesity
- Smoke
- Gender (women> men)
- Sedentary lifestyle (long-distance flights = economy class syndrome)
- Childbirth
- Varicose veins (Varicosis)
- Blood disorders (leukemia)
- Heart disease (esp. Atrial fibrillation)
- Medicines (esp. Oral contraceptives ("pill”))
- Tumor diseases (e.g. Prostate cancer or Pancreatic cancer)
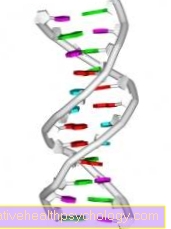
- Hereditary diseases:
The APC resistance ("Factor V Leiden mutation") is the most common hereditary disease that is associated with a risk of thrombosis. The risk of thrombosis is 7-100 times higher (depending on heredity).
Antithrombin III deficiency (AT III) mostly affects younger patients
Protein C and Protein S deficiency: If these anticoagulant factors are reduced due to a congenital deficiency, thrombosis can already occur in adolescence.
Hyperhomocysteinemia is an inherited impaired degradation ability of homocysteine with greatly increased homocysteine levels in the blood. Consequences include an increased risk of thrombosis.
All of the hereditary diseases mentioned can be diagnosed through blood tests. - Liver diseases with insufficient formation of coagulation factors (e.g. Cirrhosis of the liver)
Also read: Thrombosis while taking the pill and Thrombosis causes
Frequency / occurrence
In Germany approx. 200,000 thromboses per year registered. Women are predominantly affected.
Symptoms / complaints
There are no clear indications or signs to prove the presence of a thrombosis. The symptoms can vary widely, so that a thrombosis can also be asymptomatic (1/3 of all cases).
Symptoms that occur frequently are:
- aching calf pain
- Increase in discomfort when standing, decrease when lying down
- increased vein markings of the surface veins (bypass circuit), especially the front edge of the tibia = Pratt warning veins
- overheat
- tight, shiny skin
- Calf pressure pain (Lowenberg sign)
- Calf pain when walking (Hohmann sign)
- Sole pain when pressure is applied to the inner sole of the foot (Payr sign)
- fever
- Increase in inflammation in the blood
diagnosis
There are two ways to safely diagnose thrombosis. In addition to the symptoms that indicate a thrombosis, there are device-supported options for:
- Doppler sonography (ultrasound)
- Contrast agent display of the venous system (phlebography)
With Doppler sonography (ultrasound / sonography) the flow velocity in the vascular system can be shown. If there is a venous thrombosis, an interruption in blood flow is detected.
The ultrasound examination has no side effects.
Read more on the topic: Doppler sonography
The contrast medium display of the venous system is the safest method to detect a thrombosis.
In this method, the patient is given contrast agent into a vein in the back of the foot. Interruptions in the vascular system can be shown under X-ray control.
The risks of the examination are allergic reactions and the low radiation exposure of the examination.
Since the contrast agent contains iodine, this examination should not be carried out in the case of known iodine allergies or hyperthyroidism.
The so-called D-dimer is available for blood tests / laboratory values.
D-dimers are formed when thrombosis is broken down and can be detected in the blood. If this value is increased, this indicates a thrombosis. The D-dimer is always increased after operations and often in tumor diseases.
Read more on the topic: Detect thrombosis
Recognize a thrombosis
A thrombosis is a blood clot in the vascular system that clogs the blood vessel and prevents the blood flow.
The blood eventually builds up in the affected part of the body, causing it to become a swelling, to dull, sore muscles and the affected part of the body turns blue or red.
With the help of these typical symptoms, affected persons can already recognize a thrombosis themselves.
Other symptoms that can indicate a thrombosis are a feeling of tension, a feeling of heaviness, overheating or increased vein markings on the affected part of the body. An increase in the discomfort while standing and a decrease in discomfort while lying down are also characteristic. If a thrombosis is suspected, a doctor should always be consulted. This can be done using various examination methods, such as Laboratory controls and one Doppler sonography, a special ultrasound examination of the veins, detect thromboses with a high degree of certainty and finally initiate treatment.
Therapy of thrombosis

Therapy goals are:
- to prevent the thrombosis from growing
- to avoid a clot spread (embolism)
- To restore the original blood flow.
The form of therapy initiated depends on the location, size and duration of the existence of the thrombosis.
The blood clot is transformed into a scar in a short time. Therefore, thrombosis therapy should be initiated within the first 10 days in order to be able to preserve the original vessel.
The following therapy options are available:
- drug dissolution of the clot (thrombolysis)
- surgical removal of the clot (throbectomy)
- Bridging by surgical bypass circuit (bypass)
As therapeutics stands Heparin (nowadays mostly low molecular weight heparins with fewer complications) and for the later phase Marcumar available (provided there are no contraindications) as well as drugs that dissolve thrombosis.
Heparin prevents the thrombus from growing and reduces the risk of one Pulmonary embolism.
Thrombosis-dissolving drugs (fibrinolytics) have the risk that bleeding can occur when used.
Therefore, lysis therapy must not be used after strong operations high blood pressure, Pregnancy or older age.
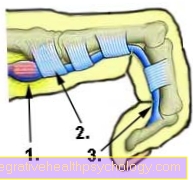
Stockings (compression stockings)

In addition to drug therapy with heparin and rivaroxaban, physical measures such as the use of compression stockings are used to treat thrombosis.
Compression stockings are specially and individually adapted stockings that are worn on the part of the body affected by the thrombosis. Compression stockings exert external pressure on the affected, blocked blood vessel, which facilitates the outflow of blood. This leads to a reduction in pain and swelling in the affected part of the body, and in the long term to prevent skin changes.
With simultaneous moderate movement of the affected body part (Activation of the muscle pump) the blood flow is further improved. Compression stockings are available in four different degrees of strength (Grades one to four) available.
Grade two is usually used to treat a thrombosis. Compression stockings have to be re-prescribed about every six months as they lose their strength and thus their effectiveness over time.
Depending on the location of the thrombosis, compression stockings in half-thigh, knee or thigh length, as well as tights, can be used. Other clinical pictures in which compression stockings are used are, in addition to venous thrombosis, lymphedema, varicose vein disorders or chronic venous insufficiency. Compression stockings can also be worn prophylactically to prevent thrombosis, for example after an operation.
Complications
The most feared complication is this Pulmonary embolism.
If the blood clot (thrombus) adheres very loosely to the vessel wall, it can come off. The thrombus now swims with the blood flow back to the heart and then into the lungs. The pulmonary arteries become increasingly narrow. The blood clot blocks the vessel and forms a pulmonary embolism.
The part of the lungs behind the blockage can no longer participate in gas exchange. If the thrombus is very large, large parts of the lungs are no longer supplied with blood for gas exchange. If the capacity of the blood flow in the remaining lungs is exhausted, the heart quickly becomes overloaded (Right heart strain) with life-threatening complications.
Pulmonary embolism often goes undetected. A pulmonary embolism can also be detected in half of all thromboses without the patient noticing anything. In these cases, the doctor speaks of an occult, i.e. hidden pulmonary embolism.
Pelvic vein thrombosis has the highest risk of pulmonary embolism.
Post-thrombotic syndrome is a common late complication.
Thrombosis prophylaxis
To Thrombosis prophylaxis Before surgery, compression stumps are put on and heparin (low molecular weight heparin derivatives) are administered as an injection. The dose depends on the risk potential of the patient (already had a thrombosis?) And the operation (high-risk operation like artificial knee joint, artificial hip joint) from.
Early exercise is also important for blood circulation.
You can find more about thrombosis prophylaxis under our topic: Thrombosis prophylaxis
After the thrombosis has been overcome, a blood-thinning drug is often given for a limited period (6-12 months) (Marcumar) given to avoid re-thrombosis.
forecast

Many thromboses heal without consequences after timely therapy. In particular, if a thrombosis is not detected in time, the risk of permanent damage is high.
If a thrombosis is not treated, scar tissue will develop from the blood clot after a few days. This scar tissue usually forms a new duct, i.e. a new vessel. Problems with the new vessels, however, are that they do not have venous valves. Venous valves allow blood to flow in only one direction (towards the heart).
A possible consequence of the uncontrolled blood flow as a result of the missing venous valves is an overload of the superficial venous system. Varicose veins (Varices) can arise.
The full picture of overload is called post-thrombotic syndrome.
The consequences are:
- Water retention in the tissue (edema)
- the development of varicose veins (varices)
- inflammation of the skin (dermatitis) and
- the formation of open ulcers (ulcus cruris).
Once there was a thrombosis, the risk of a new thrombosis is considerable! Men in particular are at great risk of re-thrombosis.
For upcoming operations, the Thrombosis protection can be run particularly high with heparin.
Thrombosis in the eye
Thrombosis in the eye is also possible. The thrombus forms in a vein that supplies the retina (retina) and therefore leads to impaired vision. Rapid therapy is important in order to be able to reverse the possible damage.
Thrombosis in pregnancy
During one pregnancy the risk of thrombosis is increased. The reasons for this are on the one hand the changed hormonal balance of the woman but also the pressure that the child exerts on the maternal vessels. Also the Inheritance plays a role. For example, if the mother or grandmother of the pregnant woman already had a thrombosis, the risk of thrombosis during pregnancy is increased. To avoid thrombosis are Support stockings and also regularly Move helpful.
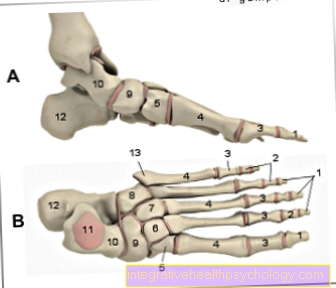
Thrombosis in the leg
Venous thromboses are most commonly localized in the leg.
- About 50 percent of venous thromboses in the leg affect the femoral vein, the Femoral vein.
- About 20 percent fall on the knee veins, the Popliteal vein and various lower leg veins.
- The last 10 percent affect the pelvic vein, which Iliac vein.
In some cases the thrombus may rise to the lower level Vena cava, the Inferior vena cava come. Due to the course of the venous vessels in the leg, the left leg is also more often affected.
When creating Thrombosis in the leg A slowdown in blood flow, a changed composition of the blood and damage to the vascular walls play a role.
The development of a thrombosis in the leg is favored by numerous risk factors, such as:
- female gender
- Smoke or
- Obesity
Venous thrombosis manifests itself as swelling, blue discoloration, and sore muscles in the affected leg.
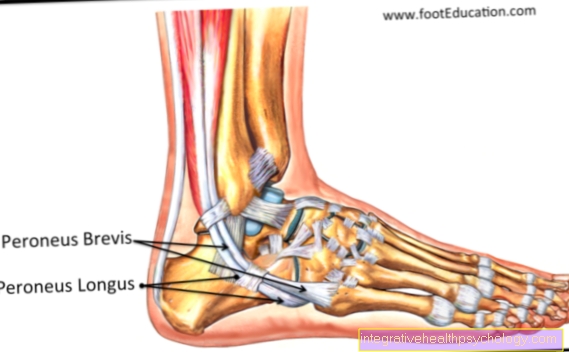
Furthermore, there is overheating and a feeling of tension in the affected leg. Pain is also characteristic Pressure on the calf (Meyer sign) and at Extension of the foot (Homans sign), as well as pain when pressure is applied to the sole of the foot (Payr sign).
The diagnosis of venous thrombosis in the leg is made on the basis of the typical symptoms and Doppler sonography, a special ultrasound examination of the leg veins.
Venous thrombosis of the leg should be treated in any case, as the thrombus in the leg can loosen and be washed into the lungs. One then speaks of one Pulmonary embolism, a life-threatening complication of thrombosis in the leg.
For the treatment of thrombosis in the leg, blood-thinning drugs such as Heparin or Rivaroxaban, as well as physical measures such as compression treatment with stockings.
Furthermore, the affected leg should be moved; bed rest and protection of the affected leg are only recommended if the pain is severe. Depending on the risk, the measures mentioned are also used to prevent a new thrombosis in the leg.
Thrombosis and pill
There are numerous factors that increase the risk of developing thrombosis.
In particular, the combination of different risk factors increases the risk. An important and common risk factor in women is the use of oral contraception, the so-called pill.
Oral contraceptives are drugs that are mainly used to Prevention of pregnancy are taken and contain two active ingredients, the hormones estrogen and progestin.
Depending on the preparation, the two active ingredients are combined (Combination preparation), or just the progestin alone (Single substance preparation) contain. By taking oral contraceptives, hormonal control loops are created between brain, Ovaries and uterus and thereby prevents the fertilization of an egg.
The estrogen prevents ovulation, while the progestin makes the mucus in the uterus more viscous. The viscous mucus makes it difficult for the Sperm.
These mechanisms lead to reliable contraception of pregnancy. Common unwanted side effects of an oral contraceptive are nausea, Vomit, Weight gain, a headache, Blemishes, Hair loss and Cycle irregularities.
Another important but rarer side effect is the occurrence of Thrombosis while taking the pill. Estrogens lead to changes in the vessel walls and a slowdown in blood flow and can thus promote the occurrence of thrombosis.
To reduce the risk of thrombosis, oral contraceptives with a low estrogen content are therefore recommended.
There are also various gestagens, such as this Levonorgestrelwhich, in combination with low-dose estrogen, have a lower risk of thrombosis than other preparations. Particularly in women with other risk factors such as smoking, obesity, a coagulation disorder or age over 35, care should be taken to use a preparation with a favorable side effect profile.
Women who already have a thrombosis in the leg or other thromboembolic diseases such as a pulmonary embolism or a stroke should not use an oral contraceptive. A gynecologist can provide information about alternative contraceptive methods.