Deep vein thrombosis
definition
A deep vein thrombosis (DVT), also known as phlebothrombosis, is caused by an occlusive Blood clot in a deep vein evoked.
The clot forms due to various disorders of the blood and vascular system such as a modified one Blood composition, Blood flow rate or Vessel wall.

The signs of deep vein thrombosis are swelling, tenderness, and cyanosis of the affected leg. Cyanosis is a bluish discoloration of the skin caused by a lack of oxygen. To clarify such symptoms or to avoid complications such as pulmonary embolism, a doctor should be consulted.
Read more on the topic Thrombosis in the leg and burning sensation in the leg
causes
Normally, the blood contains cells, the so-called platelets (thrombocytes) and coagulation factors, which are used to close vascular injuries and thus stop the blood from leaking out of the vessel.
The blood platelets or thrombocytes and coagulation factors have to be activated by various factors or activate each other so that a blood clot forms and closes injuries. However, if the cells or coagulation factors are activated by various pathological processes in the body and thus form clots, sometimes even without an injury being present, these clots can partially or completely block a vessel. Blood can then no longer flow through the clogged vessel and it backs up. If the affected vessel is a deep leg vein, this leads to a deep vein thrombosis.
Three factors are important for the development of deep vein thrombosis, of which only a single one or all of them can be changed at the same time.
On the one hand, there is damage to the inner vessel wall (endothelium). This vascular wall can be damaged by inflammation or by trauma. As a result of this damage, substances that promote coagulation become active, which lead to the formation of clots. This clot can be so large that it obstructs blood flow. However, it can also loosen and get stuck in a constriction during the migration through the veins and clog the vessel so that the blood can no longer flow.
The second factor is decreased blood flow rate. By slowing blood flow, the clotting factors have time to react with each other and activate, even when there is no injury. A blood clot forms and the result is a deep vein thrombosis.
Various things can reduce blood flow. Immobilization after an operation, varicose veins or external pressure on the legs can lead to a decrease in blood flow. Heat treatment can also slow the blood flow. The veins relax and widen, so that the blood can no longer be transported from the legs to the heart quickly enough.
Further information on this topic can be found at: Pain after knee surgery
The last factor is an altered blood composition. Hereditary diseases can alter the composition of the blood and thus lead to increased blood clotting. Furthermore, drug treatment can lead to an increased risk of clot formation.
Read more on the topic Causes of Thrombosis
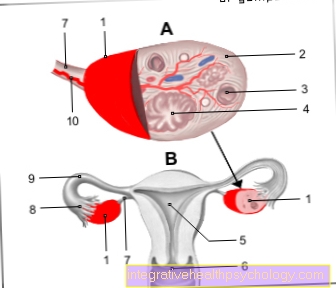
These causes can also lead to a pelvic vein thrombosis. This is problematic because of its symptom-free course, which is why it can be discovered too late. Also read the following article in this context: Pelvic vein thrombosis
Symptoms
A deep vein thrombosis can develop certain symptoms to make noticable. However, it can also remain symptom-free. If symptoms occur, there are three typical symptoms in the affected leg where the clot has formed. Leg swelling, one dull pain as well as one Discoloration of the skin due to lack of oxygen in the blood (cyanosis). It can also become a Overheating of the leg come.
Also a Feeling of tension or heaviness in the legs may indicate a deep vein thrombosis. Since the blood flow is disturbed and the blood backs up in a deep vein thrombosis, a increased vein markings to make noticable.
If there are complications such as one Pulmonary embolism, symptoms can include sudden shortness of breath and dizziness. A feeling of weakness is also possible. Pulmonary embolism is one Occlusion of one or more pulmonary arteries. These can include caused by a clot in the legs that has migrated in the bloodstream.
Diagnosis
Even a deep vein thrombosis can only be recognized when symptoms occur. For example, you can optically do a bluish discoloration or one increased vein markings recognize on the affected leg. The leg may feel warmer than the other. Also indicates a Dull pain a deep vein thrombosis in the leg. So you can independently perform the so-called "Homans sign", whereby the tip of the foot is pulled upwards. The sign is positive when there is pain in the calf. However, all of these symptoms are not sure signs that a deep vein thrombosis is actually present, as other conditions such as a torn muscle can also be involved.
To A doctor should be consulted for clarification In addition to the visual and tactile changes mentioned above, imaging methods such as the Color duplex sonography can apply. The veins are displayed on a screen and compressed (compressed) with the aid of the ultrasound head. In a healthy person, the veins can be compressed. If there is a thrombosis, compression is not possible.
Also can Laboratory values, such as a D-dimer increase, indicate a deep vein thrombosis.
therapy
If a deep vein thrombosis is diagnosed, the doctor initiates what is known as acute therapy. The aim here is to prevent pulmonary embolism, to avoid the spread of the thrombosis and to make the vessel passable again (recanalization) and to avert secondary diseases such as post-thrombotic syndrome.
For this a compression treatment is started. For the time being, an elastic bandage is applied because the leg is still swollen and a compression stocking that is adapted to the patient would not make sense. When the swelling has subsided, a compression stocking is fitted and must be worn during the day for at least 3 months. In addition, the patient should take care to exercise enough. If there is too much pain or a pulmonary embolism, bed rest is usually ordered. In addition to these general measures, drug therapy is carried out. For this purpose, blood-thinning medication is given for at least 5 days. The blood is thinned into the vein using low molecular weight heparin (LMWH) such as Clexane®, so that clots cannot form again.
So-called factor Xa inhibitors, for example fondaparinux, can also be given. If the kidneys are weak, Clexane® must not be given. Then the so-called unfractionated heparins (UFH) are used.
Another alternative is Xarelto®. This drug contains the active ingredient rivaroxaban and inhibits coagulation factor X, which is very important for clot formation. Unlike the heparins, Xarelto is given orally as a tablet and not into the vein.
The third goal, recanalization, is achieved by means of so-called thrombolysis or fibrinolysis. This is intended to dissolve the clot that has formed. Various drugs such as streptokinase or urokinase can be used to dissolve the thrombus.
One surgical method to remove the thrombus is a thrombectomy. The thrombus is removed from the vessel using a catheter. This procedure is mainly used for clots in the pelvic veins in young patients or to prevent a limb amputation. After the emergency measures, maintenance therapy with coumarins (vitamin K antagonists) takes place. How long therapy is necessary depends on the circumstances and the risk of developing a new thrombosis. Therapy can last at least 3 months up to 1 year.
Compression stockings for the treatment of deep vein thrombosis
Compression stockings are an important part of deep vein thrombosis treatment. A compression stocking is used for this Class II adapted to the patient who applies a mean pressure of approximately 25-30 mmHg on the leg. Through the external pressure should he Blood flow in Accelerated towards the heart become. This is also important in order to prevent secondary damage such as post-thrombotic syndrome.
It is important that compression stockings can either be put on by the patient independently or that a nurse or assistant takes over this work, since the compression stocking cannot or cannot sufficiently fulfill its task without being properly put on. Compression stockings are reimbursed by the statutory health insurance.
Risk factors
Various factors favor the development or increase the risk of developing a deep vein thrombosis (.
For example, there is a 30 times higher riskif the patient is already at a deep Leg vein thrombosis or pulmonary embolism was ill in the past. Is there a longer one Inability to move For example, long-haul flights, an injury or operations that require a longer layover time increase the risk by a factor of 20.
Various Hereditary diseases, the one increased blood clotting also increase the risk of deep vein thrombosis. Another risk factor sets in BMI over 30 In addition, the likelihood of deep vein thrombosis increases with age, especially in patients over 60 years of age. There is also a greater risk with Womenwho the Take pill and at the same time smoke.
Also Tumors can increase the risk of deep vein thrombosis. During the pregnancy and the puerperium usually increases blood clotting so that the woman does not bleed to death during and after childbirth. Therefore, the risk is also increased here.
Guideline for the diagnosis and treatment of deep vein thrombosis
For the Diagnostics and therapy deep vein thrombosis medical guidelines, which should support doctors in deciding which diagnostics and therapy to use. It should be noted that the doctors do not have to adhere to these recommendations, but therapies can be individually adapted for the patient.
It is therefore recommended that the diagnosis should begin with an assessment of the probability of a deep vein thrombosis. There is the so-called Wells Score, of the Risk factors such as symptoms of a leg vein thrombosis, previous thrombosis or pulmonary embolism, a heart rate over 100 beats / minute and much more in a point system.
If you get a score above 6, there is a high probability of a deep vein thrombosis. There is also one Recommendation for therapy the deep vein thrombosis and also one List of approved drugs. According to the guideline, blood should be thinned with the approved drugs as early as possible.
Consequences of deep vein thrombosis
As a serious consequence of the deep vein thrombosis counts the Pulmonary embolism. This represents a life-threatening complication in which the Blood clots through the veins from the leg to the heart and lungs hiked and there one Clogged artery.
Symptoms are above all one to fast or difficult breathing, Dizziness and weakness. This condition should be treated as soon as possible.
A further episode deep vein thrombosis can do that Post-Thrombotic Syndrome be. The blood flow obstruction caused by the clot results in a Damage to the venous valves. As a result, the blood can no longer be transported well from the legs to the heart and sags in the legs.
Leg swelling, pain and even open ulcers can result from impaired wound healing. Rapid treatment of deep vein thrombosis is therefore important in order to prevent secondary damage.
Exercise after deep vein thrombosis
After deep vein thrombosis is Sport recommended. It should above all Endurance sports how To go biking, Walking, Swimming or hiking operate. The patient should be careful not to exercise too intensely at the beginning and to adapt the sport to their physical condition.
In the beginning, compression stockings should also be worn, which can gradually be left out if there is no longer any pain or swelling. The exact procedure should always be discussed with the attending physician.




.jpg)