Uveitis
introduction
Inflammation of the middle skin of the eye (Uvea), which in turn is divided into three layers, is called uveitis. Every year 50,000 people develop new uveitis, around 500,000 people currently suffer from the dangerous disease.
The risk of infection is relatively low, but a possible consequential damage of uveitis is loss of vision, which makes it so dangerous for those affected. Uveitis is often confused with the highly contagious conjunctivitis.

Symptoms
You can tell whether you have uveitis by the fact that the eye is very reddened, there is stabbing pain, the eye is watery, you can only see blurred, the pupil is narrowed and bright light makes the symptoms worse.
If the eyesight deteriorates and a visual disturbance with veils or blurred spots persists, it is very likely that chronic uveitis is already present.
causes
Possible triggers for the inflammation of the uvea are bacteria, viruses or fungi.
Chronic inflammation in other parts of the body can also cause uveitis. These include a rheumatic disease, chronic inflammatory bowel disease, an autoimmune disease or acute stress. In the case of inflammatory bowel diseases such as Crohn's disease and ulcerative colitis, uveitis can be an indication of a new flare-up.
Read more on the topic: Crohn's disease attack
Can stress be a triggering cause?
Stress can cause various physical and psychological complications. It activates different brain regions. The consequences are muscle tension, hormone release, increased blood pressure, etc. In most cases, acute stress leads to few long-term complications, especially not in the eye.
But chronic stress, combined with other side effects such as chronically high blood pressure or sugar, can lead to long-term damage to the eye. However, uveitis is usually an acute inflammation. Therefore, stress is only in very rare cases the trigger for uveitis.
What role does HLA B27 play?
HLA B27 describes a leukocyte antigen and is located on the surface of human cells. It has important functions in the immune system. A mutation in the gene of this protein complex is associated with various autoimmune diseases. Those affected have an increased risk of diseases such as Bechterew's disease, Reiter's disease or other spondylarthritis. These diseases are often associated with acute uveitides. The association with the HLA-B27, however, has primarily classification purposes. The prognosis of uveitids does not usually change.
Therapy of uveitis
In order to prevent permanent damage, the inflammation should be relieved quickly and effectively by an ophthalmologist. The anti-inflammatory drug cortisone is usually used for this purpose and substances for immunosuppression are also used (Damping the immune system) for use.
Depending on the cause, treatment should then be continued and other existing chronic inflammations in the organism should be eliminated, stress should be reduced and rheumatic diseases should be treated therapeutically.
Humira
Humira is a medicine that contains the antibody adalimumab. This antibody acts against tumor necrosis factor-α (TNFα). It is mainly used to treat rheumatic and autoimmune diseases, such as rheumatoid arthritis, psoriasis, spondylitis, Crohn's disease and ulcerative colitis. Because uveitis is often associated with these conditions, Humira is often used in the treatment of uveitis. However, it can lead to some side effects such as allergy, nausea, anemia etc. and should only be taken under regular control by a specialist.
Duration of uveitis
With good treatment, uveitis can heal within a few days to weeks without complications. An early diagnosis is a prerequisite. The disease is chronic only in rare cases. However, the prognosis often depends on the underlying disease.
What is the healing like?
The likelihood of a cure lies on the one hand in the early diagnosis and on the other hand in the underlying disease. With early diagnosis and good therapy, symptoms are relieved within a few days. However, if the underlying disease is not treated effectively, the uveitis can become chronic, making healing more difficult. Chronic uveitis usually occurs in 25%. If it becomes chronic, the likelihood of further complications, such as increasing visual disturbances or glaucoma, also increases.
forecast
In some cases, inflammation of the uvea is chronic, with an increased risk of complications. Consequential damage can be reduced or prevented by early therapy, so that the speed of therapy is decisive for success.
Complications
Possible complications are adhesions between the iris and the lens, an increase in intraocular pressure (glaucoma), clouding of the lens of the eye (cataract), the storage of calcium in the cornea (Ligament keratopathy), a development of what is known as macular edema (water retention at the point of sharpest vision) or blindness.
The clouding of the lens of the eye (Cataracts, cataracts) and the increase in intraocular pressure (Glaucoma, glaucoma) can be a complication of uveitis, but also a side effect of prolonged cortisone therapy.
If uveitis occurs more often, a regular eye check by the ophthalmologist is recommended every three months, regardless of symptoms.
Forms of uveitis
What is anterior uveitis?
Uveitis is an inflammation of the vascular skin of the eye. This layer, which lies between the sclera and the retina, is also known as the uvea. It consists of the iris (iris), the ciliary body (Corpus ciliary) and the choroid (Choroid). Depending on which components are affected, a distinction is made between anterior and posterior uveitis.
Anterior uveitis is an inflammation of the iris and the ciliary body. Collectively, this is also known as iridocyclitis. This disease occurs mainly in systemic diseases such as Bechterew's disease, Crohn's disease, ulcerative colitis or sarcoid. An anterior uveitis can also occur with infectious diseases such as herpes, chickenpox, borreliosis or syphilis.
Most affected patients complain of pain in the eye area and redness. In some cases, chronic uveitides have few symptoms. The therapy consists of a high dose of cortisone, which often relieves symptoms within a few days.
What is posterior uveitis?
Posterior uveitis causes inflammation of the vitreous humor, choroid, and retina. Together it can also be called chorioretinitis or retinochoroiditis. This condition can occur with many diseases. The eye is often involved, especially in rheumatic diseases and inflammatory bowel diseases. But also with infectious diseases caused by viruses (herpes, chickenpox, rubella, etc.), bacteria (e.g. tuberculosis) and fungi, posterior uveitis can occur.
Affected patients often complain of impaired vision. The absence of pain is typical of the disease, as the affected structures have no nerves. The therapy consists primarily in the treatment of the underlying disease with antibiotics or antivirals and, if necessary, the additional administration of cortisone.
What is intermedia uveitis?
In intermediate uveitis there is inflammation of the ciliary body (Cyclitis). Similar to anterior uveitis, this disease occurs primarily in systemic diseases such as Bechterew's disease, Crohn's disease, ulcerative colitis or sarcoid. Infectious diseases such as herpes, chickenpox, borreliosis or syphilis can also lead to uveitis intermedia.
In most cases, affected patients complain of pain in the eye area, but this is usually not as severe as with anterior uveitis. In addition, redness can occur. The therapy consists of a high dose of cortisone, which often relieves symptoms within a few days.
What is fox uveitis?
Fuchs 'uveitis, also known as Fuchs' uveitis syndrome (FUS) or Fuchs heterochromic iridocyclitis, is an inflammation of the anterior segment of the eye. It is named after the Austrian ophthalmologist Ernst Fuchs. This rare, often chronic disease affects young adults in particular. Usually it only occurs on one side. The first sign is often a color difference in both eyes (Heterochromia). Affected patients have rainbow skins of different colors. The eye with the lighter color often represents the sick eye. The disease is usually benign and in most cases is mild. However, regular examinations often still make sense, as affected patients often have a higher risk of developing glaucoma.
Difference between iritis and uveitis
Uveitis is an inflammation of the skin of the blood vessels. It consists of different structures. The iris only denotes the iris. If there is inflammation (Iritis) only this structure is affected.
However, similar to anterior, intermedia and posterior uveitis, this disease occurs more frequently in systemic and autoimmune diseases such as rheumatoid arthritis, Crohn's disease, ulcerative colitis or sarcoid. Infectious diseases are also often associated with isolated iris inflammation.
Here, too, patients often complain of reddening of the eyes, visual disturbances and pain. Therapy consists of administering cortisone and treating the underlying disease.
How do I find a specialist?
Uveitis is a relatively common eye disease and should be treated by any ophthalmologist. There are no specialists. However, the search for an ophthalmologist is often not that easy. There are not many of them and those who do often have no appointments. In the beginning it makes sense to search the internet for the ophthalmologists and read reviews. As a rule, your own family doctor often knows a good contact point.
In rare cases it also makes sense to visit special eye clinics, as these have a larger repertoire of diagnostics.
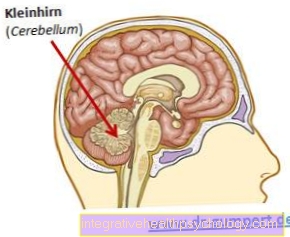
Can uveitis be an indication of MS?
Multiple sclerosis (MS) is a chronic inflammatory disease of the central nervous system. This results in damage to the nerves with consequences for the whole body. Common initial symptoms are visual disturbances and inflammation of the optic nerves. There is no clear association with uveitis, but it is often much more common in MS patients than in those who are not affected. The uveitis intermedia occurs above all. The exact cause of this increased likelihood of illness has not yet been clarified. However, if there is only uveitis and no other symptoms corresponding to MS, it is relatively unlikely that those affected will have MS.
Read more on the subject at: Multiple sclerosis diagnosis












.jpg)