How contagious is pneumonia?
introduction
Pneumonia, whether caused by viruses or bacteria, is not contagious per se in the sense that it can automatically trigger pneumonia in another person.
There are numerous pathogens that can cause pneumonia. In most cases these are bacteria, in some cases viruses, and in a few exceptions, pneumonia is caused by fungi.
General information on pneumonia can be found under our main topic: Pneumonia
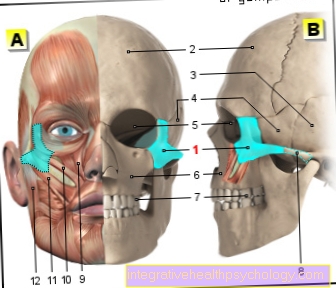
Figure Risk of infection from pneumonia
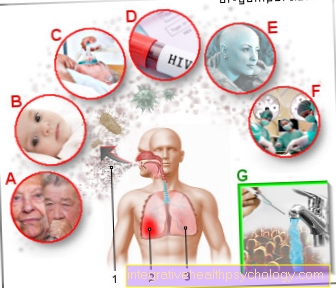
Pneumonia contagious
- Droplet transfer
(Speaking, coughing, sneezing) - Lung infection -
(Infection with bacteria,
Viruses and fungi)
pneumonia - Healthy left lung -
Pulmo sinister
Particularly vulnerable
Groups of people:
A - Elderly patients
(fewer defense cells and antibodies)
B - infants and young children
(Immune system not that strong yet
pronounced)
C - patients with multimorbidity
(many parallel
Diseases)
D - patients with HIV infection
E - diseases in the frame
chemotherapy
F - patients after a
Organ transplant,
Cancer
How can you get a contagion
avoid:
G - Regular hand washing
(disinfect),
Avoid close physical contact
with an infected person and
large gatherings of people,
Vaccination (see doctor)
You can find an overview of all Dr-Gumpert images at: medical illustrations
Viruses are known to be able to get through the air, i.e. in the form of so-called Droplet infectionto get from one patient to another. The transmission route is therefore relatively simple and happens quickly, especially when people come close to one another.
The transfer of bacteria In the case of pneumonia, this does not happen so easily because the bacteria are mostly present in the bronchial secretions and do not “fly” freely through the exhaled air.
Mushrooms on the other hand, pneumonia is a rare cause of pneumonia but it is a form that can also pass quickly from one carrier to another. Fungi that caused pneumonia are also found in the Exhaled air of the affected patient, usually in the form of small spurs. In principle, the fungal spores can also be inhaled by other people through the air and lead to the same course of disease there.
In some cases that happens Transmission from animals to humans. The germ Chlamydia psittaci is found in bird droppings and, if dried droppings get into the air in summer, people can accidentally inhale them and cause pneumonia.
The so-called Legionnaires' disease, caused by Legionella, can also be transferred to humans. In most cases, legionella are kept in the Water and pipe systems in older houses on. Legionella can survive and multiply in this system for a long time, especially when the base temperature of the water is low. The name legionnaires' disease comes from the earlier legions who contracted legionella in hotels with old water pipes and got pneumonia. The main infection is the inhalation of legionella, which are in evaporating water (water vapor when showering, etc.).
Besides mushrooms, Chlamydia or Legionella, the numerous viruses that cause pneumonia are also transmitted by air. To be mentioned here Influenza viruses, RS viruses and Adenoviruses.
Typical bacteria that cause pneumonia are: Streptococci, Staphylococci, Pseudomonads, Mycoplasma, E. Coli and Klebsiella.
In principle, the pathogens of whatever kind that can trigger pneumonia are contagious and can be transmitted from person to person via various routes (but mostly airborne droplet infection).
With a few exceptions, however, the pathogens do not necessarily trigger the same symptoms and the same course of the disease in the infected patient, i.e. even if a patient changes from a fellow patient who has pneumonia with e.g. Streptococcus does not mean that these pathogens also trigger pneumonia in him.
Many factors play a role here, most of which are closely related to the immune system. Patients with a compromised immune system have a comparably higher risk of developing pneumonia.
Above all, older patients should be mentioned here, whose immune system is often no longer as reactive, as well as small children who do not yet have such a mature immune system and patients who have many and severe comorbidities. So-called multimorbidity (many parallel diseases) weaken the immune system and thus increase the likelihood of infection.
Furthermore, pretreated patients, e.g. if you are pretreated in oncological diseases as part of chemotherapy, you are at great risk of developing pneumonia.
These patients should therefore not be so close to fellow patients who have pneumonia. Patients with HIV or those who have had organ transplants are also immunocompromised and are at high risk of developing pneumonia.
Transmission of fungal pneumonia also has an increased risk of being transmitted from person to person, even if there is no previous immune-depressing disease or many comorbidities.
Patients who have pneumonia caused by fungi should therefore initially distance themselves from their surroundings.
Treated pneumonia, on the other hand, are no longer as strongly infectious.
In principle, however, it can be stated that the transmission of pneumonia is a problem mainly in patients whose immune system is weakened. In healthy patients, in most cases there is no outbreak of pneumonia, even if the pathogens were inhaled through the air (droplet infection). The reason is that in healthy people, the immune system reacts immediately when pathogens enter the organism. This also happens when pathogens enter the respiratory system (lungs). In the form of phagocytes (Macrophages), the pathogens are usually rendered harmless within a very short time and thus cannot establish themselves in the lungs and multiply. Either the pathogens are broken down by the macrophages or they are bound by mucus and coughed up.
Also read our article: Pneumonia incubation period
Risk of infection with small children
Pneumonia is relatively common in young children and babies.
This is to a large extent due to the weaker immune system of the children, which cannot fight off the pathogens that are responsible for the development of pneumonia so easily. In addition, children are often confronted with pathogens and put their hands in their mouths. This makes it easier for a baby to get infected from an adult or other infected child and develop pneumonia themselves.
An infection with a certain bacterial pathogen, the so-called pneumococci, is usually only possible if the affected baby has not been vaccinated against infection with the pathogen. The Standing Vaccination Commission (STIKO) recommends vaccination against pneumococci for babies from the age of 2 months. A vaccination against the bacterium Haemophilus Influenza Type B is also recommended for small children.
Despite vaccinations, infection with other bacteria or viruses can occur and pneumonia can develop in babies. As a general rule, if the symptoms of the disease go away, infection is unlikely.
In the case of pneumonia caused by bacteria, in particular, infection is only likely via the coughed up mucus.
Read more on the topic:
- Pneumonia in the baby
- Pneumonia in the child
- Vaccination against pneumococci
Contagion during pregnancy
In general, pneumonia during pregnancy is no more common than in other people.
If pneumonia is nevertheless present, it is usually treated in the hospital under strict observation in pregnant women.
There will only be certain ones Antibiotics used for therapy which are unproblematic for the mother as well as for the child and pose no danger.
Pneumonia in the mother cannot be passed on to the unborn child. Since pneumonia has a strongly debilitating effect on the mother, it requires special medical attention.
As a prophylactic measure, vaccination is generally not recommended before pregnancy to prevent pneumonia.
There is an exception for women who have the spleen got removed. Vaccination against pneumococcal bacteria is recommended for these women.
Infection after antibiotics
In many cases, pneumonia is treated with antibiotics. Which antibiotic is used depends on the individual disease severity as well as the age and immune status.
Pneumonia is not considered particularly contagious for otherwise healthy people. Infection is more likely for people whose immune system is weakened.
This can be due to other infections such as HIV or chemotherapy, or simply the age of the person. Immunocompromised people should avoid contact with people with pneumonia. The risk of infection with pneumonia after antibiotic use depends on various factors.
Above all, the pathogen that is responsible for the inflammation is decisive for this. If taking the antibiotic improves symptoms, it is likely that the antibiotic you are taking is working against the bacteria in the lungs. Then it applies that after about 3-4 days an infection of others is considered unlikely. If symptoms persist or viral pneumonia is present, this rule does not apply.
In these cases, infection is possible as long as the symptoms of pneumonia persist.
Find out more about the topic here: Antibiotics for pneumonia.
incubation period
The incubation period describes the time in which a person already carries the pathogen, but the disease which it triggers has not yet broken out. This explains why a general incubation period for pneumonia cannot be given.
This depends on the individual pathogen with which the person has become infected. So can in case of infection with the bacterium Streptococcus pneumoniae the incubation period is only one day. Other pathogens can lead to an incubation period of over a month.
Most pathogens that can cause pneumonia, however, have an incubation period of 1-3 weeks. Specifying the incubation time is also difficult when infected with a virus. In addition to the individual pathogen, the body's own immune system is also responsible for the duration of the incubation period. A weak immune system can sometimes only control a pathogen for hours before pneumonia breaks out, whereas a strong immune system keeps some pathogens in check for weeks and the disease breaks out after a month. In general, however, a person who is infected with a pathogen, although the disease has not yet broken out, is still potentially contagious for his environment.
How can you avoid infection?
In general, pneumonia does not count as a highly contagious disease for normally healthy people. An infection of an otherwise healthy patient with a strong immune system is not likely, even if he is in direct contact with a sick person.
In order to avoid infection with pneumonia in the area, the basic rules of hygiene should be observed. Regular hand washing and preferably disinfecting the hands as well as strict avoidance of close physical contact with an infected person are among these rules.
Immunocompromised people should also avoid large crowds in order to avoid infection. A vaccination against certain pathogens can be useful. Whether the vaccination can be recommended individually should be discussed with a doctor. In some cases, a vaccination against certain bacteria is required by law, for example when it comes to risk groups such as medical staff.