Wound healing
introduction
Wounds can heal primarily or secondarily. In primary wound healing, the wound edges adapt themselves or are adapted without tension using sutures. The wounds usually heal very quickly and with almost no scars. All that remains is a fine, barely visible scar.
Prerequisites for primary wound healing are smooth wound edges, non-irritating wounds and no infections may occur. Typically, these prerequisites are given after operations, for wounds caused by sharp objects or after larger superficial wounds (e.g. abrasions).
You might also be interested in this topic:
- Bruises
- Laceration
- Lacerated wound

Secondary wound healing usually does not take place without complications. The wound edges are not smooth and they cannot adapt well to each other or cannot be adapted without tension using sutures. The wound heals from the depths through granulation, contraction and epithelialization.
The wound remains open until the end, so that pus and wound secretions can drain. Secondary wound healing occurs as a result of infections or a poor circulation situation (e.g. gangrenous foot in diabetes mellitus). The healing process takes much longer than with primary wound healing and a wider scar remains.
Stages of wound healing
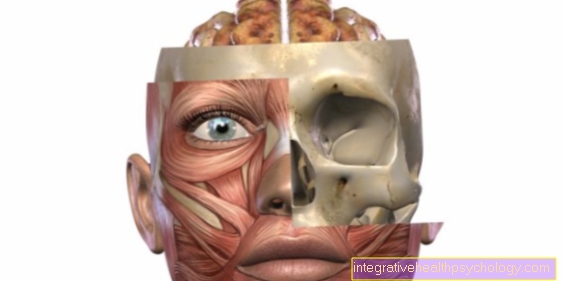
A tissue defect can be closed either by regeneration or by repairing the tissue. During physiological regeneration or in the event of superficial injuries (e.g. skin abrasions), the tissue is completely replaced by the original tissue. No scars remain and the tissue is as functional again after healing as it was before the injury.
The epidermis and mucous membranes in particular have this ability to regenerate. The vast majority of injuries, especially deeper injuries to the skin, heal through repair. This creates inferior replacement tissue (scar tissue). This is less functional. It only closes the defect, but is not capable of all cellular differentiation forms. This means that no skin appendages such as hair or sweat glands can be formed.
The reparation is divided into four main phases.
- In the exudation phase of wound healing (1st to 8th hour after injury) the capillaries are initially narrowed in order to keep blood loss as low as possible, clotting begins and hemostasis occurs. This causes the vessels to widen, causing white blood cells and platelets to be transported to the injury site. The wound is filled with wound secretion, dead collagen particles are removed and growth-promoting cytokines are released. Fibrin formation occurs. This closes the wound defect mechanically and makes it resistant to mechanical stress.
- At the first to fourth day After the injury, the resorption phase of wound healing occurs. This is shaped by the body's own defenses. Bacteria are repelled, necrotic tissue is cleared away and the fibrin is dissolved again. The entire resorption phase is characterized by the cleaning and defense of foreign bodies in order to protect the wound from infections and to prepare it for new cells to grow in.
- The proliferatin phase of wound healing follows the resorption phase (3rd to 10th day) on. In this phase new capillaries sprout (Angiogenesis). In addition, new epithelial cells and fibroblasts are activated. These close the wound defect mechanically. The strongly capillarized connective tissue grows from the edge of the wound into the wound until the defect is completely filled. Due to the strong capillarization, the wound appears grainy (= granulum, lat- the granule) and is therefore also referred to as granulation tissue.
- The differentiation phase of wound healing begins around the 7th day. This can last for months and consists of the actual scarring. The number of connective tissue cells in the area of the wound decreases, as does the number of capillaries. There is an increase in fibrous connective tissue.
- Wound healing concludes with epithelialization. Here, marginal epithelial cells migrate into the fibrous connective tissue and the actual scar is created. The resulting scar tissue is initially raised and impressed with a reddish color. After a few weeks, the scar tissue will adjust to the level of the skin and the color will fade. A white scar appears. Since the pigment cells (Melanocytes) are not regenerable, the scar remains lighter than the rest of the skin surface.
Overall, the wound is most sensitive in the period between the clearing of the necrosis and the build-up of granulation tissue. Mechanical stress in this phase can lead to serious complications and severely impair wound healing. After collagen synthesis has started, the mechanical load-bearing capacity and tear resistance of the wound increase continuously. Rough times can be given as a guide: After approx. 1 week of wound healing, the tear strength of the wound is approx. 3%, after 3 weeks approx. 20% of the maximum. This maximum tear strength of a scar is around 80% and is reached after around 3 months.
Read more on the topic:
- Phases of wound healing
and - Scar care
Phases of wound healing

The body begins to close the wound again just minutes after a wound has formed. Depending on the author, a distinction is made between three to five phases of wound healing, which overlap in time. The process is as follows:
- Rest or latency period
- Exudation phase
- Granulation or proliferation phase
- Regeneration phase
- Maturation phase.
If one only speaks of three phases, the first and last phase are omitted.
The latency phase describes the period between the onset of the injury and the onset of wound healing; this period is called the latency period. Immediately after the wound has formed, a blood clot forms from leaking blood from injured vessels, so that major blood loss can be prevented by closing the vessels again as quickly as possible.
The exudation phase then follows. In medicine, exudation refers to the leakage of fluid. In this case, the exudate consists of a liquid that is squeezed out of the blood, more precisely the blood serum, and is then called wound secretion. The task of the wound secretion is to flush foreign bodies out of the wound. The secretion also contains cells of our immune system, especially scavenger cells (lat .:Macrophages) and white blood cells (especially Granulocytes) that kill bacteria and pick up and remove dead material from the wound. For example, dead skin and clotted blood are removed from the wound to make room for the newly growing tissue. The immune cells also produce signaling substances that stimulate the cells to grow, which should later close the wound again. If there are too many bacteria in a wound, pus can develop from the wound secretion through many, many immune cells and an inflammatory reaction occurs. If only a few germs are present, the inflammation is barely noticeable. It is also contained in the wound secretion fibrin, a kind of self-adhesive. On the one hand, it is part of the blood coagulation system and, on the other hand, fibrin seals the wound edges as well as possible by sticking them together. The wound secretion usually dries up over the course of a few days, so that the typical wound scab forms on the surface. This acts like the body's own plaster and underneath it the healing process can take place undisturbed.
You can find a lot more information under our topic: Phases of wound healing
Are the wound conditions made accordingly new tissue completely close the wound again. This is done in the Granulation or proliferation phase. Proliferation means cell growth. It does this through intact cells on the edges of the wound. These begin to divide steadily and thus produce new tissue. Do the wound edges fit e.g. superficial cuts optimally on top of each other, the tissue can grow back together with the original tissue. Larger wounds must first be filled with granulation tissue. Granulation tissue describes a network of connective tissue and ingrowing blood vesselsthat has to gradually stabilize and remodel into the desired tissue. Since this tissue looks granular (lat = granulum: grain), this gave the phase its name. If the original tissue can no longer be exactly restored, it arises Scar tissue. This does not have the same properties as the original fabric and is therefore less resilient. Also missing hair, Sweat glands, Pigment cells and Nerve tracts for sensitivity e.g. against pain. New blood vessels for the supply of nutrients are also imperative for the new tissue. These sprout into the granulation tissue as the tissue multiplies and supply the new tissue with oxygen and nutrients.
The top layer of skin is also regenerated. This happens in the Regeneration or repair phase. On the one hand, new skin is formed, on the other hand, the wound edges contract and thus reduce the wound surface.
The final scar tissue takes many months to two years to form Maturation phase (Maturation = maturation). It adapts to local requirements, but always remains less resilient than the original fabric. This is also the reason why the smallest possible scars should be induced during surgical treatments.
Duration of wound healing
The Duration of wound healing cannot necessarily be strictly defined as they are used by many depends on various factors.
A well perfused, low-germ woundthat can heal primarily needs about 10 daysuntil it has healed completely and either through Scar tissue or newly formed skin was locked. In these 10 days the classic, primary wound healing different stages, which are divided into purification, granulation and differentiation phase.
In general, however, the duration of wound healing is from depending on various influencing factors: enable a good and fast healing process, for example:
- well-perfused, low-germ wound conditions
- smooth, tightly fitting wound edges
- the presence of oxygen, zinc, heat and vitamins.
negative wound healing is always affected when the The edges of the wound do not stick together lie or even necrotic are the Wound with bacteria infected, themselves excessively strong Bruising or Connective tissue growths form or Underlying diseases are presentwhich can be associated with impaired wound healing (e.g. diabetes mellitus).
How can I accelerate wound healing?
Wound healing is a complex mechanism. In addition to the blood, the main organ involved is the skin. Wound healing takes place in different stages until the new skin has formed on the injured area. Wound-promoting agents usually have zinc as an ingredient. Zinc has a healing effect and is antibacterial. In addition, zinc is a co-factor of the immune system.
Read more about this: Zinc ointment
In addition to zinc, the dermatologist can prescribe cortisone cream for complicated or inflammatory wound healing disorders. The cortisone suppresses the inflammatory reaction, which leads to faster wound healing. If the wound is infected, wound healing is difficult. Antiseptic (germicidal) ointments must be used for therapy. These can best be selected after a smear and the determination of the pathogen. If you have an infected wound, you should see a dermatologist. An infected wound can be recognized by a bad smell, discoloration of the wound base and the wound edges (mostly greenish) and increased pain.
Also read: Bepanthen® scar gel
Removal of fibrin
Fibrin deposits should be removed if they are firmly attached to the wound bed and impede healing.
Various treatments are available here. The measure is selected depending on where the fibrin deposits are located and how firm the fibrin deposits are.
The gentlest method is to rinse the wound. An antibacterial solution is used to clean the wound. If the fibrin deposits are superficial and not very firm, this can be used to remove fibrin deposits.
If this method does not work, surgical wound cleansing (Debridement) should be considered. This is a surgical procedure that is usually carried out under short anesthesia. The attending physician cleans the wound manually and removes the fibrin deposits. Care is taken to ensure that the wound edges are smooth and free of irritation. This is important for good wound healing.
If surgical debridement is not possible, other methods can be used to loosen the fibrin deposits. Chemical processes are available here, for example in the form of enzymes. However, this type of wound care takes a very long time and therefore also the wound healing.
Does the scab need to be removed?
The scab is part of natural wound healing. Scab formation occurs through the accumulation of fibrin and closes the wound. The scab also protects the wound from the ingress of germs. The scab should not be removed unless it prevents the wound from healing. Since the scab is used to protect the wound, it should be left in place until it loosens by itself. When the scab is loosened, new skin can be seen underneath.
An exception, when the scab should be removed, is the formation of pus in the wound. If pus forms under the scab, it is removed to remove the pus as well. If pus has formed under the scab, a doctor should be consulted to clean and treat the wound.
What ointments are there?
Bepanthemum ointment, for example, promotes wound healing. This is very rich and moisturizes the skin. The Bepanthes ointment is also available with an antiseptic effect, which means that this cream also has a germicidal effect.
Another ointment that works particularly well on healed scars is linola grease ointment. However, this should only be applied to the scar once it has healed. The linoleum grease ensures that the scar remains supple and that no knots form. Thus, the scar optically fades into the background.
Ointments that promote wound healing are ointments that contain zinc. The zinc promotes healing and the zinc also has a germicidal effect.
The iodine ointment is recommended as a special cream for skin injuries. Iodine also has a germicidal and healing effect. If used daily, infected wounds can be treated well. Please note that the cream rubs off strongly on textiles.
Better with or without a patch?
The plaster serves to protect against bacterial colonization. In everyday life, a plaster should be worn where a bacterial colonization of the wound is to be expected. This includes especially the hands and feet with open shoes in summer. A plaster can also be used to stop bleeding from small wounds.
It is beneficial for wound healing if air and some UV light get to the wound. This can best be achieved without a patch. Therefore, if possible, it should be ensured that the plaster is removed, for example at night, when the risk of contamination is not so high, so that air can get to the wound.
If the wound is subject to mechanical stress, for example in the shoe, a plaster should also be used for padding. This also serves for wound healing.
Wound healing in diabetes

In addition to the typical secondary diseases of the kidneys and eyes, wound healing is also impaired in many patients with longstanding diabetes. The reason for this is that the blood vessels and nerves are affected by permanently increased blood sugar levels.
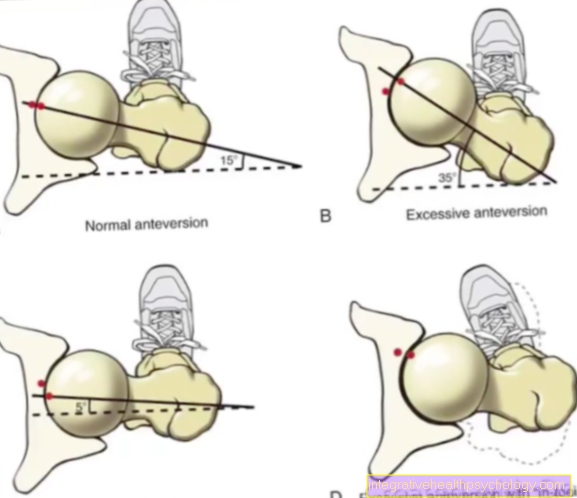
This leads to the destruction of the small vessels (Microangiopathy) and the great vessels (Macroangiopathy). Especially through the Microangiopathy it comes to circulatory disorders in the area to be supplied. The reduced blood flow leads to a deterioration in the supply of oxygen and nutrients, so that healing is worsened due to a lack of energy and nutrient supply.
A classic example is the "Diabetic foot". This late complication is very much feared, but one in four will develop it in the course of their illness. Because of the circulatory disorders in the legs, there are open spots that can no longer heal or only with great difficulty. These can even enlarge dramatically, so that in the extreme case, amputation can occur.
Chronic wounds are one of the most common sequelae of diabetes if the blood sugar is poorly controlled. One speaks of a chronic wound when a wound has not healed within four weeks with proper care. It can even happen that wounds get bigger. The causes of chronic wounds are diverse. It starts with the skin, which is losing water content due to diabetes, becoming more brittle, flaky and more vulnerable. In the case of a wound, the skin itself is already weakened and cannot do the work to build up new tissue effectively enough and thus delays wound healing. In addition, even the smallest injuries and scratches can develop into full-blown chronic wounds. The wounds are a serious risk, as they represent entry points for an enormous amount of germs which in extreme cases can cause blood poisoning in the whole body, which is often fatal.
These wounds are so dangerous that from a certain size and a certain risk of infection only the leg amputation can protect. Every year there are almost 60,000 leg amputations due to chronic wounds in diabetics.
The longer the diabetes persists, the more common the development of a diabetic foot and a chronic wound due to a wound healing disorder.
In addition, the nerves are attacked by the high blood sugar levels. It comes to one Neuropathy. Through the Neuropathy the wounds caused by shoes that are too tight go unnoticed. As a result, they get bigger and bigger and don't heal. This phenomenon can also slow down wound healing.
The immune system is also impaired by diabetes. The immune system can no longer properly protect the wound from invading bacteria and the wound becomes more easily infected. In addition, even smaller wounds become infected, which do not pose a challenge to a healthy immune system. Theoretically, every inconspicuous skin injury such as a scratch can become a gateway for germs and a wound is created.
Diabetes also damages nerve cells that are also responsible for pain perception. This means that patients do not take wounds seriously or do not even discover them in inaccessible parts of the body such as the soles of the feet and heels. In order to avoid enlargement of the wound, diabetics are advised to check their legs and feet on a daily basis in order not to miss small wounds that are later difficult to get under control.
An optimal blood sugar control can significantly reduce this risk and enables the body to heal better and faster wounds, while it is also able to fight germs effectively. The long-term sugar level (HBA1c) should be checked and the antidiabetic therapy stopped accordingly.
Read more on this topic: Therapy of diabetes
Wound healing in smokers

Like diabetes, smoking also damages blood vessels. The reason for this is arteriosclerosis (= Hardening of the arteries). The calcification leads to a narrowing of the blood vessels and a decrease in their elasticity over the years. All people experience this process in the course of their lives. However, smoking speeds up this process enormously.
In addition, substances in cigarette smoke lead to a contraction of the vascular muscles, so that the vessels also constrict. These vascular constrictions lead to an increasing lack of blood flow to various organs such as the heart, brain, skin and, of course, the arms and legs. This process is particularly noticeable in the often cold hands of smokers. This process of vasoconstriction alone allows one to understand why wounds heal more poorly in smokers, because the lack of blood circulation simply lacks the essential supply of oxygen to the cells, as well as important blood components and nutrients that are necessary for a wound to heal, and wound healing is delayed.
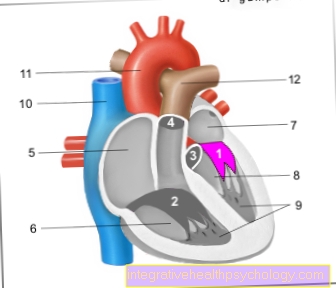
But that's not all. Smokers also inhale carbon monoxide with every cigarette. Carbon monoxide is absorbed by the oxygen carriers in the blood just like oxygen. Strictly speaking, they are much more likely to receive it. In the blood of smokers, the important oxygen carriers, the erythrocytes (= red blood cells), are saturated with carbon monoxide to a not inconsiderable extent, namely up to 15%, and so cannot transport any vital oxygen. In non-smokers, the proportion is only around 0.5% of red blood cells. The blood vessels, which are already constricted by arteriosclerosis, also deliver blood that is less oxygenated, which makes the supply of tissue even worse.
Both processes together make the critical situation of smokers clear and show why the vast majority of smokers have to deal with wound healing disorders in the course of their lives. With a progressive lack of blood circulation, in addition to wound healing disorders, more drastic situations can also arise. The best-known example is the smoker's leg, which, like the diabetic foot, often leads to amputation.
Since the problem of smokers also affects surgical wounds, smokers are advised to stop smoking before an operation and to refrain from smoking after the operation. It is particularly important not to smoke after surgery on the abdomen. This can lead to wound healing disorders of the intestines, which can have serious consequences. For example, after an intestinal operation, the two ends of the intestine cannot grow together properly and the seam can therefore open. Here, the leaking of stool into the abdominal cavity can lead to life-threatening peritonitis (Peritonitis) come. An emergency operation must be carried out here immediately.
Wound healing and alcohol
With moderate alcohol consumption, the alcohol does not interfere with wound healing. However, long-term alcohol consumption should be avoided, especially after operations. Chronic alcohol consumption weakens the immune system and makes it easier for wounds to become infected. This impairs wound healing.
However, alcohol has no direct effect on wound healing. Under no circumstances should alcohol be applied directly to an open wound. The alcohol is toxic to the tissue. Alcohol causes necrosis in the wound area, which can spread over the entire extremity and is very dangerous.
Wound healing after tooth extraction
Healing after tooth extraction is usually very quick. The mucous membranes are subject to very rapid regeneration, so that the skin can reproduce itself very quickly here. In addition, the saliva contains antibacterial substances, so that the saliva promotes wound healing. Chlorhexamed as a mouth rinse can be used for about a week after tooth extraction. This also promotes wound healing through its antibacterial effect. Care should be taken that the wound does not come into contact with coarse soiling, such as bread crumbs or the like.
Read more about the topic here: Tooth extraction
Diet after tooth extraction
When dieting after tooth extraction, care should be taken to ensure that no coarse dirt gets into the wound. This includes breadcrumbs, hot dishes or the like. In addition, the consumption of dairy products should be avoided. Eating dairy products can cause mucus to form on the wound. This hinders wound healing. Apart from the dairy products and grainy rolls, however, everything can be eaten. After eating, the mouth should be rinsed out with Chlorhexamed in order to keep the germ colonization of the wound as low as possible.
In general, care should be taken not to chew on the side of the mouth where the wound is located.
Wound healing after laser treatment
Small skin wounds remain after laser treatment. However, these usually heal very quickly. If possible, only normal skin care products should be applied to the wounds. The wounds usually heal even without sore creams. In the case of wounds that do not heal, a doctor should be consulted and individual treatment arranged.
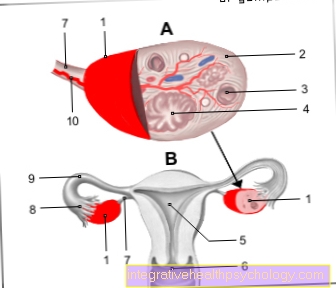
Wound healing after caesarean section
The scar from a caesarean section is treated like any surgical scar on the abdomen. The scar from a caesarean section runs horizontally. The reason for this is that there is no cutting along the course of the abdominal muscles. This prevents a predetermined breaking point from developing in the abdominal muscles. These predetermined breaking points are the reason for umbilical hernias. The intestines push through the non-intact muscle layer and thus cause instability. This can lead to entrapment of the intestines, which makes an operation with the insertion of an abdominal mesh necessary.
A so-called panhandle incision is therefore made during a caesarean section. How the scar heals after a caesarean section depends on several factors. The first factor is the type of seam. Most of the time, an intracutaneous suture is made during a caesarean section, that is, the thread is sewn into the skin and not visible on the surface. This is mainly for cosmetic reasons, but the seam is just as stable as any other seam. Then it depends on how well the seam is made. When suturing the suture, the surgeon must ensure that the wound edges are close together, but not overlapping. If the wound edges overlap, wind healing disorders can occur.
Another point is the texture of the skin. If the subcutaneous fatty tissue is poor, the wound usually heals faster. Since adipose tissue is not well supplied with blood, wound healing is sometimes more difficult. Smoking should be avoided while the wound is healing, and this should never be done during pregnancy or when caring for an infant. Smoking increases the likelihood of sudden infant death syndrome. In the first few days after the operation, the abdominal muscles should not be strained very hard. No water should get on the scar either.
Wound healing disorders
Disorders of wound healing can be caused by infections (bacterial) or caused by hematoma formation. Both should be done as quickly as possible through cleaning and antibiosis (infection) or by puncture or opening the skin suture (Hematoma) be treated.
The scar itself can heal without complications, or it can increasingly form celloid. In the process, more connective tissue is formed, which leads to unsightly scar growth in the area of the scar and beyond. In scar hypertrophy, scar growth occurs only in the area of the scar. Another complication is scar rupture due to infection or suture insufficiency. The scar bursts open and then has to be closed again.
Read more on the topic: Wound healing disorder
Promote wound healing
To a optimal wound healing In addition to good wound care, various, supportive measures can be done independently.
Flawless wound care primarily includes application or. Implementation of suitable hygiene measures (Hand disinfection, wound cleaning with Ringer's solutions, wound disinfection) when treating the wound area in order to Ingress of germs and a resulting Avoid infection of the wound.
In addition, the wound area should be covered by suitable Wound dressings closed be, in most cases moist wound environments should be created (e.g. through hydroactive wound dressings in the form of plasters or gels). This ensures that the Optimized healing process, one Barrier against microorganisms formed and the Desiccation of the wound area and the Prevents scab formation so that the Scarring and the itching during wound healing reduced becomes.
In order to additionally promote wound healing, a sufficient, balanced nutrition care must be taken that every healing process requires an increased need for energy and nutrients. In addition to a adequate hydrationto promote the blood flow to the wound area and the alluviation of immune cells and nutrients is also a sufficient supply Proteins, Carbohydrates, Fats, Vitamins (A, B, C), Trace elements (Zinc, copper, manganese, iron) necessary. over- or Underweight conditions such as Deficiencies can therefore to Wound healing disorders to lead.
Furthermore, the one affected by the wound should Body part - in particular Wounds over Joints - during the healing process kept calm and scratching or removing any build-up scab or. Crusts be avoided. Also one direct sunlight fresh wounds should be avoided.
The is also beneficial for wound healing Quit smoking, because that is in the cigarette smoke nicotine demonstrably disturbs or slows down the healing process (due to reduced blood flow, reduced oxygen supply and delayed cell regeneration).
Also warmth can wound healing influence positively, since this leads to an expansion of the vessels and an improved blood flow situation in the wound area (e.g. by using infrared heat lamps).
Should it still lead to an infection from a bacterial colonization local or systemic administration of a wound, so that the healing process is made more difficult and delayed Antibiotic the attending physician will direct the course back on the right track.
How can I promote wound healing after an operation?
Wound healing after surgery is very important. It should be noted that the scar is covered with a sterile plaster for the first few days in order to minimize the number of germs. In addition, the affected area of the skin should be exposed to little stress, i.e. the skin should not be excessively stretched or stressed. It is important to always check the scar after surgery. It is ideal if the wound is not reddened or slightly reddened and the wound edges are dry. If the edges of the wound are reddened and oozing, this can be a sign of inflammation.
In order to ensure optimal wound healing after an operation, alcohol and smoking should be avoided during this time. The ingredients in a cigarette in particular weaken the blood circulation in the skin and make healing more difficult. Another reason for impaired wound healing can be poor sutures. If the wound edges are not sewn together well, the wound healing can be delayed here as well. If there is a particularly large amount of subcutaneous fatty tissue, the wound may take longer to heal because the fatty tissue has a poorer blood supply than the rest of the skin. In addition, an infection of the affected area can be the cause of impaired wound healing.
No ointments or the like should be applied to fresh surgical wounds. The patch should be changed daily and no water should be given on the wound for the first few days.
How can I accelerate wound healing in the anus?
In contrast to other parts of the body, wound healing in the anus is more difficult. On the one hand, there is a much higher colonization of germs here, on the other hand, the wound is sometimes also exposed to mechanical stress. Wound healing can be accelerated by adhering to hygiene. For example, the wound should be cleaned after every use of the toilet. This can be done with an antibacterial soap on the bidet, or with an antibacterial wet wipe. It should be ensured that cleaning also takes place outside the toilet in the morning and in the evening. In addition to hygiene, it is important to ensure that the wound is not manipulated. This worsens wound healing. In addition, as with any wound, healing can be accelerated with an iodine cream.
physical therapy
Wound healing and physiotherapy are not mutually exclusive. Of course, the skin around the wound shouldn't be stressed by movement, but a little movement is not bad. Since the physiotherapists are medically trained, these exercises can be done with the patient without harming the wound.
Another area of wound care in physiotherapy is pressure ulcer prophylaxis. A pressure ulcer is caused by lying on the support points for a long time. Colloquially, the pressure ulcer is referred to as "bedsores".
nutrition
Like all renewal processes, the wound healing process requires sufficient nutrients and energy to run smoothly.
A lack of carbohydrates, fats, proteins, vitamins, trace elements and minerals can slow down wound healing or even in extreme cases (chronic) Lead to wound healing disorders.
The proteins primarily serve to generate energy for wound healing work and as an essential substrate for rebuilding. Carbohydrates, on the other hand, are important for enzyme and defense functions. In addition, fats play a major role in the formation and structure of new cells, while vitamins and trace elements are essential for the immune and connective tissue cells. Vitamins A, B, C and D seem to be particularly important here, as do the trace elements Selenium, zinc, copper and manganese must be available in sufficient quantities.
It is also important to have sufficient fluid intake to enable the desired blood flow and allow the nutrients to float into the wound area.
A balanced diet can therefore have a positive effect on wound healing and prevent chronic wound healing disorders.
Do vitamins support the healing process?
Vitamins are important for all of the body's functions. Usually enough vitamins are ingested with food.
The only vitamin that should be substituted for almost everyone in latitudes with less sun is vitamin D3. Vitamin D3 is produced by the skin with the help of sunlight. Since the sun doesn't shine particularly often in this country depending on the season and is also weak, almost everyone has a vitamin D3 deficiency. However, the memory can easily be refilled in the form of tablets. Vitamin D3 is available over the counter in pharmacies. A vitamin D3 deficiency can show up on the skin in the form of sores or rough areas.Rhagades at the corners of the mouth are also typical. These wounds can be healed with vitamin D3. Vitamins also have a healing effect on other wounds.
homeopathy
There are some homeopathic remedies available to promote wound healing. These can be taken orally as globules or applied topically as compresses or tinctures.
Calendula is available for wound healing on the body. Calendula is said to have an anti-inflammatory effect. It also promotes wound healing and scar healing.
However, the Staphisagria is particularly suitable for the pain after sewing a wound. It is particularly effective for deeper injuries and has a pain-relieving effect.
The Hypericum is said to work particularly well after dental treatments.
Read more on this topic: homeopathic medicines
Home remedies
Sea water is a well-known home remedy for promoting wound healing. Generally, however, it should be handled with care. Sea water is said to have an anti-inflammatory effect due to the high salt content. But not with open wounds. In the case of open wounds, it is essential to keep away from sea water.
Air often helps with wounds. The oxygen allows the wound to heal more quickly, which is why a plaster should not always be worn. Here it is advisable to take off the plaster if no dirt can get into the wound.
It is also advisable to put honey on the wound. The viscous honey is like a film on the wound and prevents the wound from drying out. If the wound remains permanently moist, this is a breeding ground for bacteria.



.jpg)