Alternatives to Marcumar®
Synonyms in a broader sense
Phenprocoumon (active ingredient name), coumarins, vitamin K antagonists (inhibitors), anticoagulants, anticoagulants
What are alternatives to Marcumar®?
The drug known under the trade name Marcumar® contains the active ingredient phenprocoumon, this active ingredient belongs to the main group of coumarins (vitamin K antagonists). Medicines that contain the active ingredient warfarin also belong to this class of drugs.
The term coumarins is used to summarize those medicinal products that have a suppressive effect on the natural processes of blood clotting and thus inhibit the clotting of the blood (anticoagulants).

In contrast to other anti-clotting drugs, the effect of coumarins is very slow delayed a. This can be explained by the fact that vitamin K antagonists can only develop an effect when the natural supply of vitamin K and already carboxylated, fully activatable coagulation factors have been used up.
For this reason, they cannot be used in acute emergency situations, but only in long-lasting, chronic bleeding disorders Find.
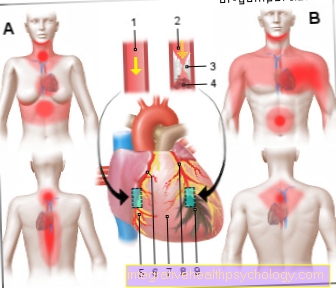
Marcumar® is usually used to prevent one thrombosis applied, this can be in the context of an implantation of artificial heart valves or Vascular bypasses, to Heart attacks or with chronic Cardiac arrhythmias become necessary.
Due to the comparatively extensive side effects and counter-signs, there are now many alternative active ingredients that can be used for therapy with Marcumar® can be circumvented.
These are mainly drugs that contain the active ingredient Warfarin or Acenocoumarol contain or are derived from them.
Examples of such drugs are those under the trade name Coumadin or Sintrom known anticoagulants.

Each of these alternative drugs has the same mechanism of action as Marcumar®However, the difference is based on the different half-lives (half-life), i.e. also the duration of the effectiveness within the organism. This duration of action depends on the time the body needs to break down the drug. The half-life (half-life), in turn, is the exact time in which the drug concentration has decreased by exactly half the amount originally administered.
The half-life (half-life) of Marcumar® is approximately 70 - 95 hoursthat from Coumadin only approx 30-40 hours and the time in which the Sinitrom concentration has decreased to exactly half is only 9 hours.
Marcumar® therefore has the longest and Sinitrom the shortest half-life (half-life).
Knowing how long an anti-coagulant like Marcumar will work® or Sinitrom is especially important if the drug should or must be discontinued.
The deposition can be planned before major Operations or an extensive Visit to the dentist become necessary to minimize the risk of bleeding.
The effect of the anticoagulant can be based on the so-called INR value be measured. The INR value is an international measure for assessing blood coagulation. High values mean that the coagulation time is longer than the normal value and that the Bleeding tendency is correspondingly high. A low value, on the other hand, suggests a shortened blood clotting time and an associated increase Risk of thrombosis.
Basically it can be said that anti-coagulant drugs like Marcumar®, Coumadin and Sintrom increase the INR value and thus reduce the risk of thrombus formation.
The normalization of this value after discontinuation of the anticoagulant occurs after administration of Sintrom already after one to two days after taking Marcumar® this usually takes up to two weeks.
Another promising substitute for coumarin therapy is one under the trade name Eliquis known drug. The active ingredient in this medicine is a molecule called Apixaban.
In contrast to the coumarins, apixaban does not act on all vitamin K-dependent blood clotting factors but selectively only on the Factor X.
Clinical studies show that both the possible side effects and the contraindications for an alternative therapy with apixaban are considerably lower.
This is a valuable new alternative strategy, especially for patients for whom normal therapy with the help of coumarin-containing drugs cannot be carried out without problems.
However, it has not yet been conclusively clarified whether this Marcumar®- Replacement can keep up with the intensity of action of the coumarins in the long term.
Pradaxa®
The commercial product Pradaxa® contains the active ingredient dabigatran etexilate. The active ingredient is one of the direct thrombin inhibitors. This means that it directly and reversibly inhibits what is known as thrombin. Thrombin plays an important role in blood clotting. The active ingredient dabigatran etexilate therefore inhibits blood clotting in this way. The indications are similar to those of the active ingredient phenprocoumon. At 12-14 hours, Pradaxa® has a significantly shorter half-life than Macumar®. The advantage of this is that you can react more flexibly. When unplanned operations have to be carried out and the blood-thinning effect of the medication has to be stopped quickly, a short half-life of the active ingredient is practical. However, a longer half-life, as with the Marcumar®, has the advantage that stability in the blood plasma can be achieved.
Read more on the topic: Blood clotting
Furthermore, under certain conditions, no coagulation monitoring is necessary during treatment with Pradaxa®. This means that the target range of the INR value can be estimated in persons with healthy liver and kidney functions. It is more difficult in people with disorders of the kidney or liver. The methods of coagulation monitoring, as with the Marcumar®, cannot be used for Pradaxa®. There are special tests to check the effects of dabigatran etexilate. But these tests are only available in specialized laboratories. In addition, Marcumar® and Pradaxa® are metabolized differently. Since the active ingredient dabigatran etexilate is metabolized via the so-called P-glycoprotein, it is independent of certain enzymes on which Marcumar® is dependent. As a result, there is less interaction with other drugs during treatment with dabigatran etexilate. However, there may be interactions with drugs that inhibit P-glycoprotein. An example of this is the antibiotic clarithromycin. The active ingredient dabigatran etexilate is largely independent of ingredients from food. Since 85% of it is eliminated via the kidneys, it is dependent on good kidney function. In addition, the Pradaxa® preparation is significantly more expensive than Marcumar®.
Xarelto®
The commercial preparation Xarelto® contains the active ingredient rivaroxaban. It is one of the direct and reversible inhibitors of coagulation factor 10. This factor also plays a very important role in blood coagulation. The indications are similar to those for the other anticoagulants. Rivaroxaban has a half-life of 7-11 hours. This makes it more flexible to control. With Xarelto® therapy, the same conditions and limits apply to coagulation monitoring as with Pradaxa®. The active ingredient rivaroxaban is partly metabolized by the same enzymes as Marcumar®.
You may also be interested in this topic:
- Xarelto® and alcohol
Another part is also metabolized via a P-glycoprotein. The interaction with other drugs is low, but can occur. Interactions with certain ingredients in food are less common. 1/3 of Xarelto® is excreted via the kidneys. If uncontrolled bleeding or other side effects occur, it is difficult to react quickly to the active substance rivaroxaban. The countermeasures for overdose that are used with Phenprocoumon do not work here. The same is true for dabigatran etexilate. However, there is a so-called antidote for Pradaxa®. This does not yet exist for rivaroxaban, but it is to be developed. In terms of costs, Xarelto® is somewhat cheaper than Pradaxa®, but also significantly more expensive than Marcumar®.
You might also be interested in the topic: What should be considered when stopping Xarelto?
Eliquis®
The commercial preparation Eliquis® contains the active ingredient apixaban. It is also one of the direct and reversible inhibitors of blood coagulation factor 10. It belongs to the same class of substances as Xarelto®. It therefore has properties similar to Xarelto®. It's a little younger. While Xarelto® came onto the market in 2008, Eliquis® has been on the market since 2011. The indications are similar. The so-called pharmacokinetics are slightly different. That means how the organism affects the drug is different for the preparations. Elquis® has a half-life of 9-14 hours. It has a slightly lower bioavailability. Accordingly, it has a bioavailability of 50%, while Xarelto® shows a bioavailability of over 80%. That can have advantages and disadvantages.
A higher bioavailability means a stronger distribution and effect in the body. But it also means that the side effects, such as a tendency to bleed, can be more pronounced. An antidote is also currently being developed for the active ingredient apixaban.Eliquis® is eliminated 1/4 via the kidneys and 3/4 via the bile. There are certain contraindications for Pradaxa®, Elquis® and Xarelto®. These include pregnancy and acute, clinically relevant bleeding, diseases with risk factors for severe bleeding and the simultaneous use of other anticoagulants such as heparin. The recommendation for kidney dysfunction is different for the three preparations.















.jpg)