Osteoarthritis in the knee
Synonyms
Gonarthrosis, knee arthrosis, knee arthrosis
definition
Osteoarthritis in the knee is an irreversible, progressive destruction of the Knee joint, mostly as a result of a permanent Disproportion between Load and resilience.

introduction
By the age of 75, around 60-90% of people have one or more joints arthrosis. The Knee osteoarthritis occurs less often than, for example Osteoarthritis in the fingers.
Since the knee is a central joint that is always connected to the total body weight is stressed, the suffering of the patient is relatively more pronounced, and there are greater restrictions on the quality of life than if smaller joints are affected.
The bony knee joint consists of three bones:
- Thigh bone (femur)
- Lower leg bone (tibia)
and - Kneecap (patella).
These can all together (Pangonarthrosis) or individually affected by arthritic changes.
One of the most common forms of osteoarthritis is that between the thighbone and the kneecap (femoropatellar arthrosis = kneecap arthrosis).
Symptoms
Often the Osteoarthritis in the knee mute for the first few years. This means that changes in the joint can already be seen on the X-ray, but the person concerned has no symptoms.
At the beginning, the patients describe their symptoms as stiffness and extensive Joint pain and Muscle aches.
Within a activated osteoarthritis can the knee swell and overheated appear. The increased pressure in the knee joint can also lead to the development of a Popliteal cyst come. The mobility of the knee is more limited due to the pain, which improves again after the irritation subsides (e.g. a break for several days).
Especially in the morning, after getting up, and after sitting for a long time, the disease develops as the disease progresses Starting painwhich disappears after a few minutes of movement.
Some patients feel stronger discomfort in damp or cold weather.
After several years of illness, deformities of the joints, misalignments and tiredness pain can occur.
Without therapy, patients with osteoarthritis of the knee can be so limited in their ability to walk that they have to move with forearm crutches or in a wheelchair / rollator. However, an almost symptom-free course is also possible. As is usually the case in life, the individual course lies somewhere in between.
Appointment with a knee specialist?
I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The knee joint is one of the joints with the greatest stress.
Therefore, the treatment of the knee joint (e.g. meniscus tear, cartilage damage, cruciate ligament damage, runner's knee, etc.) requires a lot of experience.
I treat a wide variety of knee diseases in a conservative way.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
causes
Primary and secondary arthrosis are to be distinguished based on their causes.
While with a primary osteoarthritis the reason unknown stays with one secondary osteoarthritis another illness or a Trauma / accident of the knee precedes osteoarthritis.
Special causes for secondary osteoarthritis of the knee are long-standing malpositions such as Knock knees (genu valgum) or Bow legs (genu varum). There is a disproportion between the load and the load-bearing capacity of the middle or outer joint space and thus the unilateral wear and tear of the articular cartilage.
Other causes are previous injuries in the knee joint space such as Fractures / breaks of the thigh or lower leg bone with gap formation in the joint as well Meniscal injuries.
If bumps remain on the joint surfaces after injuries in the knee, the cartilage on the opposite sides is increasingly worn down to the point of Bald bone.
Frequent carrying of heavy objects (mostly at work) contributes to increased pressure in the knee joint, so that degenerative changes in the cartilage surfaces occur more quickly.
Working in a kneeling position, such as Laying tiles puts enormous strain on the knee.
As a result, under certain conditions, osteoarthritis in the knee has been Recognized as an occupational disease in 2009.
diagnosis
The diagnosis is made primarily on the basis of the symptoms described, the physical examination (e.g. Rubbing pain of the kneecap) and one X-ray image posed. Typical signs such as narrowing of the joint space, bone extensions and deformities can be visible here.
The expression of the changes on the X-ray image however, they do not have to correspond to the severity of the complaints.
If anything is unclear, you should Infections such as inflammatory rheumatic diseases be excluded.
Therapy of knee osteoarthritis
First of all, the therapy of osteoarthritis in the knee should be started by reducing the load on the knee joint:
- Weight loss
- Appropriate diet for osteoarthritis
- Improvement of the cushioning (e.g. through a running analysis)
and - Exercise that is gentle on the joints, such as swimming, Nordic walking or cross trainer and easy jogging (please refer: Sport for knee osteoarthritis, strengthening exercises for knee osteoarthritis and is it allowed to jog despite knee osteoarthritis?)
Physiotherapeutic measures (see knee school osteoarthritis) are intended to improve and maintain the mobility of the joints and to counteract possible deformities through targeted muscle building. A therapy with ultrasonic waves is recommended here.
Depending on the patient's condition, heat or cold can provide pain relief.
Drugs like:
- Ibuprofen
- Diclofenac
- Paracetamol
- Metamizole
- Cox 2 inhibitors
or - also weak opioids
are used successfully for pain therapy.
During activated osteoarthritis, injections of glucocorticoids into the knee joint can contain the inflammation and speed it up.
Read more on the topic: Knee osteoarthritis, which drugs help?
Multiple injections of hyaluronic acid into the joint space improve the mechanical properties of the cartilage and synovial fluid.
Learn more about: Hyaluronic acid for knee osteoarthritis.
Depending on the patient's level of suffering and the prospect of improvement, there are various options for treating osteoarthritis of the knee surgically. In addition to minor interventions (knee arthroscopy) such as flushing the knee joint (lavage) or smoothing cartilage (debridement), especially in the case of low-grade osteoarthritis, conversion osteotomies and prosthetic knee joint replacements (knee prosthesis) are available.
Joint replacement procedures on the knee are now the method of choice for severe osteoarthritis. If the middle or outer joint space is affected alone, a unilateral (unicondylar) surface replacement ("sled prosthesis") can be used.
If there is pangonarthrosis (all surfaces of the joint are affected), a complete surface replacement, a total knee joint prosthesis (knee prosthesis for short) would be preferred.
Depending on the condition of the knee ligaments, different prosthesis variants come into question, which must be selected according to the clinical picture.
Read more on the topic: Therapy of knee osteoarthritis
Prognosis and prophylaxis
Osteoarthritis in the knee is to be prevented primarily through balanced strain on the knees.
These include:
- Body weight in the normal range
- straight axis of the legs (footwear / insoles)
- joint-friendly sport (swimming, cycling)
Please also read: Knee osteoarthritis. which sport is advisable?
- Avoid additional weight loading by carrying heavy objects.
Even if all these factors are taken into account, the development of osteoarthritis in the course of life cannot be ruled out, as it is also crucially dependent on genetic factors.
If osteoarthritis is present, it can only be treated symptomatically and can only be largely cured with a knee prosthesis. It should be noted that a joint prosthesis can only approximately bring back the movements and stability of the natural knee.
The course of the disease can be very different. While some patients have only minor symptoms over the years and can live well under conservative therapy, there are also contrary examples in which a knee prosthesis is inevitable within a few years.
Please also read: Knee osteoarthritis, when can you treat conservatively? and knee osteoarthritis, when do you have to operate?
Depending on the patient's constitution, surgery may not be useful (e.g. osteoporosis, multimorbidity). Osteoarthritis in the knee can lead to such pronounced walking difficulties that a wheelchair or walking aids are necessary to move around.
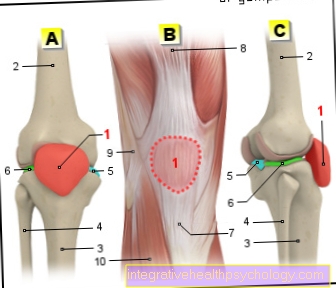
Illustration of the knee

A - Right knee joint from the left
B - Right knee joint from the front
C - Right knee joint from behind
- Kneecap - patella
- Femur - Femur
- Shin - Tibia
- Fibula - Fibula
- Inner meniscus -
Meniscus medialis - Outer meniscus -
Lateral meniscus - Kneecap ligament -
Ligamentum patellae - Outer band -
Ligament collaterale fibulare - Inner band -
Ligament collateral tibial - Posterior cruciate ligament -
Ligament cruciatum posterius - Anterior cruciate ligament - Ligament cruciatum anterius
You can find an overview of all Dr-Gumpert images at: medical illustrations