Herniated disc of the thoracic spine
Synonyms:
Disc prolapse, Nucleus pulposus prolapse
definition
Under a herniated vagina, that too Prolapse can be mentioned, one understands the back pain and sensory disturbances up to motor failures caused by a nerve root compression in the spinal cord. This means that in severe cases, movement and especially walking can be restricted.
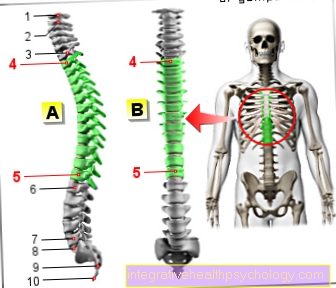
The herniated disc occurs in the vertebral bodies of the cervical, thoracic and especially lumbar spine.
Read more about the topic here: disc prolapse

root cause
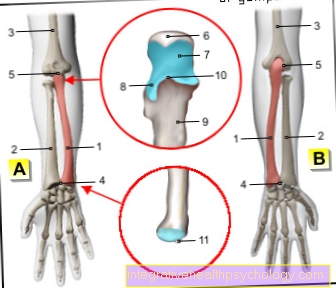
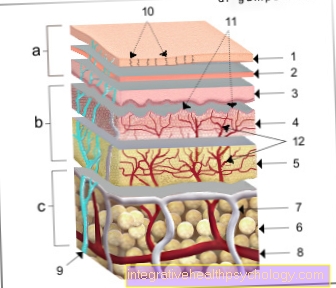
The intervertebral discs are located along the entire spine between the individual bony vertebral bodies. The intervertebral discs consist of an outer fiber ring (Annulus fibrosus) and an inner central gelatinous nucleus (Nucleus pulposus). These two structures serve to buffer the stress that affects the spine and contribute to optimal mobility.
With increasing age, the water-binding capacity of the gelatinous core decreases and cracks and crevices begin to form in the outer fiber ring, which means that the buffering effect is also lost. This process is called degenerative change designated. Now degenerative parts of the central gelatinous nucleus can penetrate these cracks. In doing so, the tissue usually everts backwards towards the back or laterally to the rear. This often happens after previous sudden, indefinite movements (Lifting trauma, rotation) and overuse of the vertebral bodies.
A distinction is made between different degrees of severity in intervertebral disc degeneration: When the gelatinous nucleus is advanced within the fibrous ring, one speaks of one Protrusion. If the jelly core breaks through the fibrous ring, i.e. if it bulges into the central canal, the nerves supplying the regions below this section can be damaged. There is a constriction (Stenosis) of the central channel (Central canal) and, depending on the characteristics and direction, leads to disconnection (compression) single nerves.
In extreme cases, there is no longer any connection between the gelatinous core and the incident that emerged through the crack. As the intervertebral disc loses volume as a whole, the distance between the surrounding vertebral bodies is reduced. The pressure on the vertebral joints increases and this can lead to bony marginal bulges (Spondylosis) to lead. Because of this, changes in the vertebral bodies can also occur in parallel, which can then also constrict the nerves.
Read more on this topic at: Causes of a herniated disc
Appointment with a specialist for a herniated disc?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
A herniated disc is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
Therefore, treating a herniated disc requires a lot of experience.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
Symptoms of a herniated disc of the thoracic spine
The patients complain of sudden shooting pain, which manifests itself in a belt-shaped manner but also locally in the thoracic spine area.
Often this sudden pain is a dull thud or an unfortunate movement such as lifting a heavy object in a leaning forward position.
The radiating symptoms in this region are called intercostal neuralgia and can extend to the middle of the anterior chest. Intercostal neuralgia can cause many other symptoms.
Read more about this: Symptoms of a herniated disc of the thoracic spine
The symptoms of a herniated disc of the thoracic spine are usually felt on one side and can be more pronounced in the back or leg. The surrounding muscles are often hardened and tense. An increase in pain can be observed with coughing, straining and depending on the breathing position. The pain occurs especially when you consciously deepen your breathing, followed by the feeling of not being able to breathe properly.
Depending on the orientation and severity of the incident, the spinal cord will compress and other symptoms will appear. These include sensory disorders, such as tingling in various areas of the skin such as the thighs or legs, bladder and rectal disorders and gait problems. For example, it is then difficult for those affected to lift the forefoot. Often the patients take a pain relieving posture and feel an increasing decrease in strength in the legs. Continuous narrowing of individual nerves can lead to paraplegia.
Read more on the topic: Symptoms of a herniated disc of the thoracic spine
dizziness
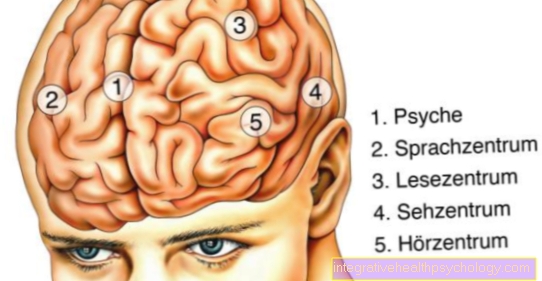
Dizziness is a multifaceted symptom. Dizziness occurs in the brain and can have many causes. Blood vessels that supply the brain with oxygen run along the spine to the skull. In the case of herniated discs, these can be impaired or squeezed. This can lead to dizziness, headaches and unconsciousness. The herniated disc can also act on the spinal cord and cause dizziness. The dizziness is often psychogenic.
If there is severe pain during the herniated disc, the body is in a stressful situation. Dizziness can occur as a psychological reaction to the pain and stress.
Chest pain with a herniated disc
In most cases, chest pain is too quickly mistaken for heart and lung problems or diseases of the upper abdominal organs. But the spine can also be behind chest pain. At the level of the 2nd and 3rd thoracic vertebrae, nerves emerge from the spinal cord, which are responsible for the sensitive supply of the superficial chest area. In the event of a herniated disc, the rupture of the disc and the emergence of the jelly-like core of the disc can cause irritation and pressure on the nerves near the spinal cord.
Often, patients have already gone through lengthy and numerous diagnostic procedures before the diagnosis of a herniated disc of the thoracic spine as the cause of the chest pain is made. Typically, the pain arises in the spine and can be passed along the rib cage from there. Movement and breathing can make the pain worse, which can differentiate it from a heart attack in some cases. With the therapy and the reduction in the swelling in the spine, the nerves also recover in most cases, so that the pain subsides.
Cardiac arrhythmia in a thoracic spine prolapse
In addition to sensitive chest complaints, a herniated disc of the thoracic spine can also have a direct influence on the heart function and especially the heart rhythm. The irritation of the nerve outlets at the level of the second and third thoracic vertebrae can lead to cardiac arrhythmias and fluctuations in blood flow to the heart.
Those affected may feel additional heartbeats, rhythm fluctuations, palpitations and palpitations. First, all potential organ-induced causes must be ruled out. Only when these are ruled out should the spine be diagnosed. Even sensitive disorders of the thoracic spine can simulate various diseases of the heart. Chest pain, along with cardiac arrhythmias, can falsely suggest a heart attack.
Stomach pain with a slipped disc
The stomach pain is also a typical symptom of a herniated disc of the thoracic spine. This is also due to irritation of the nerve cords emerging from the spinal cord, triggered by pressure of the disc fluid on the nerve roots. The pain can be projected onto the upper body along the course of the nerves and transmitted to the epigastric region and can have a pulling character. The cause can go undetected for a long time, so that those affected have often already gone through numerous diagnostic procedures.
stomach pain
Abdominal pain can be a Accompanying symptom of spinal diseases and herniated discs be. Abdominal pain occurs in the context of back pain, especially in older patients. The reasons for this are not always clear. The exact nature of the pain must be asked by the doctor and possibly an ultrasound examination should also be carried out in order to rule out possible threatening causes. The pain can be a consequence of the pressure on the abdominal organs when there are problems with the thoracic spine be. In the case of a herniated disc, inflammatory processes in the abdomen can also occur. For deep herniated discs, a Irritation of the sciatic nerve exist. This can sometimes be so severe that the pain can be felt up to the stomach, legs and toes.
Shortness of breath
Difficulty breathing is a rare symptom of a herniated disc. Shortness of breath always represents an acute emergency situation, the cause of which must be clarified as soon as possible. In most cases, the shortness of breath comes from the heart or the lungs themselves, but diseases such as the herniated disc can also be behind it.
In the case of a herniated disc, surrounding structures can be damaged by the emerging core of the disc. This can affect the spinal cord, surrounding nerves, or blood vessels. In the chest area there are some nerves that are involved in breathing movement. Many muscles on the ribs help you breathe by expanding your chest. These muscles come into play, especially when the effort is increased. If they are impaired by a herniated disc, breathing difficulties can arise in these situations.
For more information on the causes of shortness of breath, visit: Shortness of breath
frequency
Herniated discs can occur especially between the ages of 20 and 65. The most common herniated discs occur with around 62% in the lumbar spine, followed by 36% in the cervical spine.Only about 2% of all herniated discs are located in the thoracic spine.
Please also read our topics:
- Herniated disc of the cervical spine
- Herniated disc of the lumbar spine
diagnosis
First of all, the anamnesis is carefully taken. The attending physician lets the patient describe the complaints regarding pain and restricted mobility. In addition to viewing (inspection) and tapping (Palpation) of the spine, functional tests are still carried out, which should clarify the range of motion and the localization of the pain.
Depending on the severity of the abnormalities, an orientating neurological examination should also be carried out. These focus on any numbness or tingling (Sensory disturbances, paresthesias), Disorders of the reflexes and motor skills. These examinations also provide information about the location of the herniated disc.
Read more about this on our website Diagnosing a herniated disc
Imaging examinations are also carried out. This includes the X-rays in 2 planes (from the front and side), usually while standing. The actual advancement of the gelatinous nucleus cannot be seen in the X-ray image, but you get an overview of the position of the vertebral bodies in relation to each other, so that a visible decrease in height of the intervertebral disc increases the suspicion of a herniated disc. In addition, other diseases such as tumors, fractures or advanced spinal curvature (Scoliosis) can be excluded.
Another method is myelography followed by computed tomography. Contrast medium is added to the Dural space, in which the nerves run, injected and is shown in white in the finished picture. An existing constriction of nerves can now be easily recognized and the actual herniated disc becomes clearly visible.
Magnetic resonance tomography (MRI of the thoracic spine) also shows the soft tissue structures very well. This method is of the greatest importance nowadays, as it is a non-invasive and radiation-free examination.
Please also read our relevant topic:
- MRI scan of the thoracic spine
- MRI for a herniated disc
Conservative therapy
The most common form of therapy for a herniated disc is conservative treatment. This means that no operation is performed initially. Since pain relief is paramount, the patient is given pain medication (Analgesics) and medication to reduce the swelling of fluid build-up (edema) in the spinal cord (Anti-inflammatory drugs).
Another possibility is the injection of local anesthetic (Narcotics) or anti-inflammatory drugs such as cortisone in the area where the pain is occurring.
You can find more information on the topic here:
- Cortisone therapy for a herniated disc
- Medication for a herniated disc
It is also important to protect the spine by ensuring that those affected stay in bed. A relieving position for the patient is particularly important. Through the so-called Step bed supporti.e. the legs are raised by cushions and the hip and knee joint are bent, the pressure on the spine is reduced and the pain is reduced.
Physical measures such as local heat treatment, massages and electricity therapy (Electrotherapy) are intended to relieve the pain-related increased muscle tone and prevent relieving posture. Targeted physiotherapy and back training are also part of conservative therapy and help strengthen the back muscles and prevent further herniated discs.
Read more on this topic at: conservative therapy of a herniated disc
Exercises
The Physiotherapy is an important pillar of conservative therapy for herniated discs. However, the timing of the exercises is crucial. Shortly after the herniated disc, protection and drug therapy are the first priority. Only when this therapy has caused symptom relief should physiotherapy start to maintain and restore mobility in the back.
A first exercise for targeted muscle building of the upper back is the so-called "Planking". You take a position similar to push-ups, but with your forearms on the floor. Hold the position with your back and legs straight. Initially, 10 seconds are sufficient, which can be repeated 3-5 times after a short break. The time intervals and repetitions can be increased later.
Then another kneeling exercise can be performed with your hands propped up. On all fours, the back is slowly stretched into a hollow back and the head is placed back. Then the strongest possible hump is created and the head is left hanging. If the exercises are performed very slowly, there will be considerable muscle activity.
A very strenuous exercise for the upper back starts in the lying position on your stomach. Then the arms are placed on the back and the chest is lifted off the floor. The shoulder blades are pulled back. This position should be maintained for several seconds, followed by a break.
When do I need a herniated disc surgery?
Herniated discs are still operated too often, although the benefits of an operation are very limited. As a rule, equally good success can be achieved with the help of timely pain relief and professionally guided physiotherapy. A surgical procedure is only indicated in particularly acute cases with severe symptoms and indications of nerve involvement. These are, for example, neurological deficits such as paralysis or bladder and rectal disorders. If there is a threat of paraplegia, the operation should be carried out as soon as possible. If there is severe transmitted pain and sometimes organ malfunctions due to the herniated disc of the thoracic spine, the affected nerves should be relieved by surgery as soon as possible. Otherwise, surgery should only be an alternative after lengthy, unsuccessful conservative therapy and persistent symptoms.
The operation removes the advanced tissue completely from the central canal and removes other loose parts without reducing the stability of the movement segment. This intervention is called Nucleotomy designated.
In the case of more pronounced herniated discs, the affected area is accessed microsurgically from the back (dorsal). In more severe cases, such as impending paralysis, the operation area can be opened laterally through the ribs and the disc space can be removed.
During this major surgical procedure, the resulting gap is then stiffened with a bone chip and the adjacent vertebrae are screwed together.
Read more on this topic at: Operation of a herniated disc
Duration
The Duration varies greatly with the severity of the herniated disc. First of all, the risk to surrounding organs, ducts and especially the spinal cord must be excluded. Operative and conservative procedures also take different lengths of time. Depending on the severity of the disease, medical conservative therapy can improve after a few days.
After a few weeks at the latest, the symptoms should subsideso that physiotherapy can start. Above all, this should be done over a long period of time to prevent further back problems, with strength and movement training if possible forever. On average, symptoms should be free after about 1-2 months. However, these numbers are very variable, as the healing of the herniated disc depends on an enormous number of factors.
Potential paralysis and failure symptoms should also get better after a while. If there is no improvement within a few months, other therapy methods must be considered.
forecast
75% of all operated patients are after the operation symptom-free and are not restricted in your working life. About 15% of the cases becomes one significant pain relief achieved, but the ability to work is limited. 10% of those affected continue to have Residual complaints and 5% suffer from a recurrent disc prolapse in the same location.
Only 1-2% suffer one disc prolapse at a different level of the spine.




















.jpg)