Colonoscopy
synonym
Colonoscopy, intestinal examination
English: colonoscopy
Definition of colonoscopy
A colonoscopy is a diagnostic measure in which the inside of the large intestine can be inspected and diagnosed with a flexible endoscope.

Indications for a colonoscopy
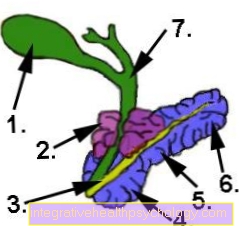
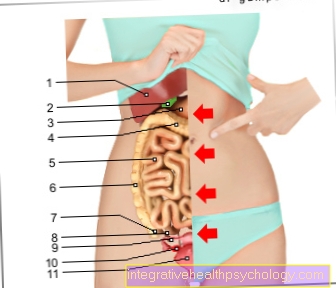
A colonoscopy (Colonoscopy) is performed to get an insight into the rectum (rectum) and the colon (colon) to get.
Indications for a colonoscopy are initially all intestinal complaints that persist over a long period of time. These include long-lasting pain in the intestine, blood in the stool, and a drop in hemoglobin in the blood count (this value can indicate bleeding in the intestine, which must be ruled out). Blood in the stool may either be immediately visible in the form of black, sticky stools (Tarry stool) noticeable or invisible to the naked eye (see: intestinal bleeding). This is why a so-called haemoccult test is often carried out, which shows whether there is blood in the stool.
Read more on the topic: Blood in the stool
In addition, colonoscopies are also performed for chronic diarrhea.
Another indication is the search for tumors based on suspicious symptoms. These include, for example, the typical triad of unclear weight loss (> 10% of body weight within 6 months), heavy night sweats and fever (>38 ° C), also known as B symptoms. A colonoscopy can also be carried out if a chronic inflammatory bowel disease such as Crohn's disease or ulcerative colitis is suspected. These can manifest themselves, for example, through abdominal pain and frequent diarrhea, some of which are bloody, and often appear for the first time at a young age. Symptoms such as changes in bowel movements such as sudden constipation (Constipation) or frequent diarrhea (Diarrhea) or a change from both, a colonoscopy should also be considered for diagnosis.
Read more on the topic:
- How is colon cancer diagnosed?
- How do you recognize colon cancer?
The colonoscopy as a preventive examination
A large area of application of colonoscopy is also the preventive examination. Every patient aged 55 and over is recommended to have a regular colonoscopy carried out as a preventive measure in order to detect colon cancer or its preliminary stages at an early stage. Like mammography or skin cancer screening, colonoscopy is paid for by the statutory health insurance companies. Experts have agreed for a number of years that the risk of developing neoplasms that can develop into malignant structures increases significantly from the age of 50. However, this has not yet been taken into account by the health system and the first preventive colonoscopy, the costs of which are covered by health insurances a maximum of twice within 10 years, is still ongoing from the age of 55 intended. Follow-up examinations should be carried out every 10 years if the results are normal. If colon polyps were seen in the examination and removed, they should already be after 5 years another colonoscopy will be done.
For people with family members who are or have suffered from cancer of the colon (colorectal carcinoma), the preventive colonoscopy has been financed by the health insurance companies in previous years. With a certain familial form of colorectal cancer, the familial adenomatous polyposis (FAP), the first colonoscopy should be in 20 years of age because the risk of illness is very high here. Following should each year a colonoscopy done.
Colon cancer is the second leading cause of fatal cancer in men and women, after the Cardiovascular diseases are the most common causes of death in Germany.
Detecting the tumor as early as possible has been shown to improve the patient's chances of recovery and survival. Nobody is obliged to conduct the investigation and everyone can decide for or against the investigation after weighing the arguments.
Before deciding to have an examination, a consultation in Germany is mandatory.In this consultation, the potential candidate contains information about the frequency of the disease being examined, the risks of the examination and what happens if one actually does one tumor finds. Those to be examined should also always bear in mind that a finding as “sick” does not always represent the final diagnosis. For many of those affected, the first conspicuous examination finding in the further course of the examinations and clarifications turns out to be harmless.
This is very impressive with the eye-catching one Breast cancer findings. In the case of this type, further examinations reveal real breast cancer only in less than 20%. The effectiveness of preventive examinations for colorectal cancer is very high, however, since colorectal cancer often arises from existing polyps, benign growths of the intestinal mucous membrane, which are present and detectable years to decades before they become tumors. A high percentage of these polyps degenerate into a tumor at some point, so that removing them can reduce the risk of colon cancer enormously.
preparation

A colonoscopy requires a few days in advance Preparations. Because the intestine has to be empty for examination so that you can even see anything in the intestine other than the remains of digested food, instead of the intestinal wall. This is done the day before the colonoscopy (around 2 p.m. the previous day) laxative prescribed. This is given to the person to be examined as a liquid to drink or as a powder, which must be drunk with a lot of liquid. Since the juice is not easy to drink for many due to the unpleasant taste, it is possible with some varieties to dilute them with a little fruit juice. However, this should be inquired about in advance.
Many patients also report that the liquid is easier to drink when cooled. The amount is about 2 litersin a time window of 90 minutes should be drunk. Another liter of the liquid should be drunk the morning before the examination. All intestinal contents should then be excreted until there is only and only clear liquid in the intestine clear or slightly brownish liquid is eliminated. The effectiveness of the examination depends crucially on the complete emptying and cleansing of the bowel. Should the intestine prove to be insufficiently emptied during the examination, a subsequent cleaning in the practice may be necessary, which can delay the duration of the examination by several hours.
In addition to the laxative, there are also a few other tips for effective bowel emptying. About 5 days before the examination, you should avoid fiber-rich foods such as grains and fruit containing seeds, as swelling grains can clog the intestines. Easily digestible foods such as porridge or yogurt should be used for the remaining days. You should refrain from eating at least from lunch the day before. If you have a sluggish bowel, you should avoid solid food beforehand. Drinks such as fruit teas, water and clear broth are allowed during the food abstinence. Black and green tea, cola and coffee, however, can leave stains on the intestinal wall and should also be avoided. By filling the intestines, the drinks often prevent the patient from feeling too hungry. If you are still hungry, chewing gum can also help, but it should only be chewed up to a maximum of two hours before the examination.
If you take medication regularly, you should also discuss the intake with your doctor. diabetic should adjust their insulin dose accordingly for the period of food abstinence. Patients who blood thinner should also discuss the procedure in the days before the examination, as taking it increases the risk of bleeding during the examination. Patients who have the Birth control pills taking additional contraception is recommended in the period after the examination, as the changed bowel function can change the absorption of the active ingredients and the effect of the pill can no longer be guaranteed.
The examination itself can be done in otherwise healthy patients outpatient be performed. This means that the patient comes for the examination in the morning and can then after a monitoring phase to be released back home.
Immediately after the examination, everything can be eaten again, only the digestive system may need a few days to recover before it has completely returned to normal.
procedure
As a rule, the patient can decide whether to use a sedative (for example Midazolam) or would like to receive a short anesthetic (mostly with propofol) so that he does not notice anything from the examination. However, it should be noted that the ability to drive for 24 hours is then considered to be impaired.
First the patient is given a so-called Flexule This is a small tube that is placed in the vein so that the sedative or narcotic can be injected. Before this happens, the patient is usually placed on his side. A pulse oximeter is also attached to the patient's finger, which measures oxygen saturation and pulse. The sedative / narcotic is injected and then you wait for it to work.
The examiner then begins to carefully insert the colonoscope rectally and advance it until it reaches the foremost part of the large intestine or the last part of the small intestine. Then the colonoscope is slowly withdrawn and air is insufflated (blown) into the intestine so that it expands, which significantly improves vision. After the examination, this air can sometimes lead to slight flatulence. Then all sections of the colon are carefully examined.
During the colonoscopy, not only can the intestine be assessed, but small interventions can also be carried out if necessary. This is possible through small tools that can be inserted into the colonoscope. In the case of minor bleeding in the large intestine, it is possible to stop bleeding using injections. If colon polyps (protruding mucous membranes that threaten to degenerate into colorectal carcinoma over the years) are discovered, these are usually removed in the same examination. In the case of narrowing (stenoses) of intestinal sections, these sections can be widened again during the examination (bougienage). If conspicuous areas of the mucous membrane are discovered, a small tissue sample (biopsy) and then sent to a laboratory for examination.
Read more about the topic here: This is how colon polyps are removed
The entire examination usually takes about 15-30 minutes. The patient can then eat and drink normally again. If the patient has been given a sedative or anesthetic, he or she will remain in the facility for monitoring for some time and can then be discharged home. In this case, however, driving is no longer permitted on this day. As a rule, the patient has no complaints after the examination. Occasionally there is a slight gas and a slight feeling of lightheadedness that can last for the rest of the day and is due to the sedative / narcotic.
If symptoms such as fever, malaise or severe abdominal pain occur following the examination, a doctor should be consulted.
Read more on the topic: The course of a colonoscopy
Findings
A common finding are Polyps of Intestines. These do not initially cause any complaints, so they are not noticed by the patient and are usually only noticed during a preventive examination.
Polyps of any kind must be removed as they are dangerous Carcinomas can develop. Usually these polyps are removed with the help of an electric loop and sent to the pathologist for diagnosis. Larger polyps must be removed with a small knife. In some cases a small suture is necessary after removal.
Bleeding is also more common during a Colonoscopy seen. Depending on whether the bleeding is acute and splashing or older and has already been stopped, the injured vessel must be ligated with the help of a small electrical device. Sometimes it is necessary that adrenaline must be injected under the vessel to seal it. In the case of heavily bleeding vessels, the vessel must be closed with a suture.
Small inflammations of the intestinal wall are usually only documented photo-technically in addition to taking a sample. All these interventions of the Colonoscopy are possible with a colonoscope under certain technical conversion.
Duration of a colonoscopy
Depending on the findings, the duration of the examination can be one Colonoscopy vary greatly. Furthermore they still play anatomical conditions a major role. The more convoluted a bowel, the more difficult it will be for the examiner to maneuver the colonoscope through the convolutions. The visibility conditions also play a major role. Has the patient had too little time before Colonoscopy drained and the intestine is not clean, the examination time can be extended. Depending on the findings and the number of samples taken, a shorter or longer examination time can also be achieved. The duration of a Colonoscopy is included, taking into account the factors mentioned above 20 minutes to an hour.
Complications / risks

Every procedure carries risks, even if the colonoscopy is generally considered to be very low-risk and safe. In Germany there are numerous therapeutic or diagnostic Colonoscopies carried out and in the rarest of cases there are complications.
However, risks are pointed out before each colonoscopy. These include first of all the intolerance to the Anesthetics. It is true that these are usually small doses and therefore also short anesthetic times. However, intolerance reactions can always occur and require intensive medical follow-up treatment.
During the colonoscopy and after the examination, bleeding may occur, which may also require further medical attention. Bleeding can occur in particular when skin areas are biopsied or when Polyps be removed. Even after the procedure, there should be a drop in hemoglobin in the Blood count think of bleeding caused by the colonoscopy.
While that Colonoscope (special tube) is moved back and forth through the intestine and maneuvered over curves and past angles, punctures can occur in individual cases (Perforations) of the intestine, which in the worst case can end in tearing the intestine and result in an emergency operation in which the intestine has to be sutured and the abdomen must be cleaned of bacteria from the intestine to prevent serious blood poisoning. However, this complication is extremely rare and in most cases it can be prevented.
The organs in the immediate vicinity of the intestine can also be affected. If there is a perforation, an open one may be possible surgical Abdominal surgery may be necessary. After bleeding or perforation, wound healing disorders and inflammation can also occur, which must also be treated separately.
Superficial injuries to the intestinal wall caused by the tube, which can lead to bleeding, are less dramatic, as is secondary bleeding after taking samples or removing polyps from the intestine. This bleeding must then be stopped during the examination or a follow-up examination necessary if the bleeding does not occur until later after the examination. As with all drugs, allergic reactions can occur to all of the materials and drugs used, which can result in life-threatening allergic shock or even death. Any use of medication and allergies should therefore be discussed in the preliminary discussion in order to keep the risk as low as possible.
All these complications are very rare and many can be prevented with sufficient experience of the examining doctor, but one must always point them out in advance of the examination, as there is no guarantee that one will not be spared. However, the risk generally increases with the age of the patient. The risk also increases for patients with a chronically inflamed bowel wall like that Crohn's disease. Since the intestinal wall is more vulnerable here, under normal circumstances the examination is never carried out during a disease flare-up and otherwise only with great care.
Read more about here Abdominal pain after colonoscopy.
The anesthesia for a colonoscopy
In the Colonoscopy (Colonoscopy) becomes a endoscope (tubular instrument with camera) through the anus into the Large intestine introduced so that the doctor can recognize any changes in the mucous membrane there. This process is usually painless, but a little uncomfortable.
A Anesthesia is during a colonoscopy therefore not absolutely necessary. In consultation with the patient, it will be decided whether the patient will experience the colonoscopy with full consciousness or whether he or she does not want this. That depends on the duration of the colonoscopy, the personal pain sensation and the patient's fear of the colonoscopy.
In most cases, however, the colonoscopy is performed under a light anesthetic called a Sedation, carried out. Here, the patient is injected with a sedative, which then lets him sleep so that he does not notice anything about the examination.
The difference to one general anesthetic is that with sedation, sleep is not as deep. Although the patient is given an infusion, he does not have to be ventilated during sedation. The Heart-However, circulatory and respiratory functions are controlled. After the colonoscopy has been performed, the patient can sleep in and is not allowed to drive a vehicle for the next 24 hours.
Sedation should definitely be used in patients with high blood pressure or heart failure. It is also recommended for very anxious patients.
Read a lot more information on this topic at: Anesthesia for a colonoscopy
Summary

Colonoscopies are also known as colonoscopy and are now a routine diagnostic and therapeutic treatment.
The procedure is carried out with the help of a colonoscope. A colonoscope is a flexible tube with a small camera, a powerful light and various openings for inserting instruments attached to the end. Glass fiber bundles guide light and color points along the colonoscope and project the image to be seen onto a screen.
Before everyone Colonoscopy the patient must first his Intestines cleanse in the form of drug laxative measures. Furthermore, he must before the Colonoscopy to be sober. Shortly before the procedure, a Short anesthesia injected and the patient positioned to the side. After that, the colonoscope is pushed into the anus and slowly until the transition from Small intestine to Large intestine advanced. In order to create optimal visibility for the examiner, the introduction of air is necessary so that the bowel unfolds during the examination.
The examiner tries to push the tube all the way forward with various rotational movements. While withdrawing, he then inspects the intestinal wall, examining it for inflammation, bleeding and Tumors and can also take samples with small pliers inserted from the outside, which are then examined microscopically. Often smaller and larger Polyps seen, which are usually removed in the same session in order to avoid the development of cancer.
Tumors are usually biopsied; in rare cases, a visual diagnosis may be sufficient in the case of advanced colon cancer. Bleeding that is seen can be stopped with suture or medication injections. The Colonoscopy is used therapeutically to clear up long-lasting pain or Diarrhea as well as frequent changes of diarrhea and Constipation and used for blood in the stool.
As a preventive check-up, everyone should start 55 years a Colonoscopy, paid for by health insurances.Despite the minor intervention, bleeding, perforation and inflammation can occur in rare cases, which require further medical attention.