Diagnosis of facet syndrome
Diagnosis of facet syndrome

The medical history (anamnese) of patients with facet syndrome and the symptoms described point the way ahead.
The physical examination for facet syndrome with the exclusion of root irritation symptoms, pressure pain over the vertebral joints (suspension pain, medically referred to as the jumping test), increased pain when reclining (backward bending) and restricted movement of the lumbar spine provides important information for diagnosing the disease.
Imaging methods help diagnose facet syndrome and its extent.
X-ray
In principle, x-rays of the spine can be described as basic imaging diagnostics. The attending physician receives an insight into the posture of the spine via the X-ray images. In addition, bony changes (reduction in calcium salts / osteoporosis, spinal curvature, a vertebral body fracture, vertebral joint arthrosis / spondylarthrosis, vertebral body attachments) and disc degradation can be recognized.
On the other hand, it cannot be seen on an X-ray to what extent the vertebral joint osteoarthritis is pressuring nerve structures.
For this purpose, sectional imaging methods such as CT (Computed Tomography) and MRI (magnetic resonance tomography) are necessary, which through their incision the width of the spinal canal and the spinal nerves (Spinal nerves) can be displayed in different views.
Appointment with a back specialist?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The spine is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
The treatment of the spine (e.g. herniated disc, facet syndrome, foramen stenosis, etc.) therefore requires a lot of experience.
I focus on a wide variety of diseases of the spine.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
CT / MRI of the back (especially cervical and lumbar spine)
The cross-sectional diagnosis (CT and MRI of the back, either with or without contrast agent) enables the pain to be assigned to a specific nerve or a specific section of the spine.
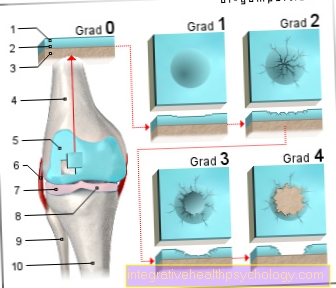
With the help of a diagnosis using CT (Computed Tomography) Examination, in particular, further questions regarding the bony structure can be answered (e.g. spondylarthrosis, spinal canal stenosis, vertebral fracture).
In contrast, diagnosis using MRI of the cervical spine / MRT of the lumbar spine is even more valuable in spinal column diagnostics (Magnetic resonance imaging), which, in addition to the bony structures, shows the soft tissue structures (intervertebral discs, nerve roots, ligaments) much better than the CT. All of the above Diseases can be detected with the MRI and assigned to a specific section of the spine.
In contrast, none of the diagnostic methods mentioned are conclusive for a facet syndrome. Even with clear evidence of vertebral joint arthrosis, it cannot be said that this image diagnosis is also the cause of the complaint.
Sample injections into the vertebral joints are therefore suitable for further diagnosis.
Diagnostic facet injection
Under X-ray control (image converter) or CT, it is possible to specifically numb or irritate the suspicious vertebral joints that have previously been identified as decisive for the cause of the facet syndrome.
This can be done either through a targeted injection of hypertonic saline solution (pain provocation) or a local anesthetic (pain relief). In one case, patients would report an increase in their typical pain, in the other case they would be pain-free for some time.