Diagnosis of coronary artery disease
anamnese
The anamnesis, the collection of the medical history, comes first in the diagnosis. If the patient is suspected of having coronary heart disease (CHD), risk factors such as:
- Smoke
- High blood pressure or
- Diabetes mellitus
and the family anamnesis regarding cardiovascular diseases (cardiovascular diseases) of the closest relatives (grandparents, parents, siblings, biological children) are collected.

The main symptom for the diagnosis of CHD is angina pectoris (chest pain, "tightness of the chest").
If angina attacks have occurred in the patient's medical history, cardiovascular disease is likely. The absence of these symptoms does not rule out coronary heart disease (CHD), however, since a high percentage of ischemias (lack of oxygen in the heart muscle cells) is silent, i.e. without anginal discomfort.
In the next step, the patient should describe the nature of the pain, indicate the location and describe the situations in which the seizures occurred. It is important to find out whether the symptoms have increased in intensity, duration and frequency and whether there was a response to the use of nitro preparations. With this information, a distinction can be made between the stable and the unstable form of angina.
In addition, questions should be asked about shortness of breath, palpitations / racing heart (palpitations) or short periods of unconsciousness, as these can be further symptoms of coronary heart disease (CHD).
Physical examination
The physical exam looks for risk factors that predispose to the development of coronary artery disease. Obesity, increased blood pressure or weak pulses in the hands and / or feet can indicate arterial circulatory disorders.
What can the blood count show in coronary heart disease?
Blood is drawn and parameters such as total cholesterol, lipoprotein and blood sugar levels are determined. If angina pectoris is unstable, troponin-T or -I can be determined. The troponins are sensitive markers for an acute heart attack.
Usually no direct “marker” for coronary artery disease (CHD) can be found in the blood. Instead, attention is paid primarily to laboratory values that favor CHD and thus make the diagnosis probable.
However, these examinations are only effective if the previously asked symptoms match a CHD. Badly balanced blood lipids (cholesterol) are a particular risk factor for CHD. The higher the LDL and the lower the HDL, the more likely it is that a CHD is present or can develop.
Since diabetes mellitus (blood sugar disease) also plays a role, the blood sugar is also determined.
Can the doctor hear anything unusual while listening to it?
The physical examination of people with coronary heart disease is usually normal at first glance. Normally nothing is noticeable when listening to the heart. Only when subsequent damage has occurred due to coronary artery disease (CHD) can these possibly be monitored.
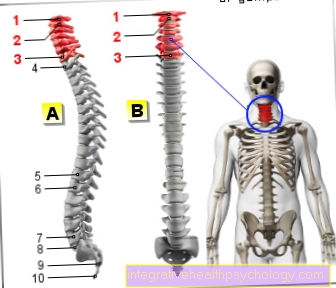
CHD is characterized by calcification of the coronary vessels. These calcifications can also occur in other parts of the vascular system. Are for example the so-called Carotids (Arteries that lead from the heart through the neck to the head, carotid arteries) affected by the calcification, flow noises may be found here when listening.
Resting EKG
The Resting ECG (EKG = echocardiogram), in which the patient lies on his back and does not put any strain on himself, can have an indicative function in the diagnosis of CHD. Through a EKG the electrical processes in the heart are mapped in the form of a characteristic EKG curve. Various heart diseases lead to changes in the normal EKG curve. If the patient has not had a heart attack with myocardial ischemia (lack of oxygen in the heart muscle cells), the resting ECG is normal in many CAD patients or only offers uncharacteristic changes that are not conclusive for CAD.
Exercise ECG
An exercise ECG (Ergometry) can be carried out as part of CHD diagnostics to determine ECG changes during physical exertion. Under controlled conditions and under medical supervision, an increase in cardiac output and oxygen consumption is induced in the patient. This can be used to prove myocardial ischemia (lack of oxygen in the heart muscle cells), which occurs as a result of coronary heart disease (CHD). Characteristic changes in the ECG, such as a depression of the ST segment, indicate the presence of coronary heart disease.
An exercise ECG should include In no case should the patient suffer from unstable angina pectoris, have recently had a heart attack, an acute one Myocarditis is ill, has a cardiac defect with clinical symptoms or is known to have severe general illnesses.
Please also read our page Exercise ECG.
Long-term ECG
A Long-term ECG Over 24 hours, ischemia-related EKG changes and, above all, silent ischemias (oxygen deficiency in the myocardial cells without symptoms for the patient) can show.
Stress echocardiography, myocardial scintigraphy and coronary angiography are to be mentioned as imaging methods for assessing the presence of CHD, with coronary angiography not only having a diagnostic function but also of therapeutic importance in CHD treatment.
Echocardiography
The Echocardiography, a sonographic examination (ultrasound) of the heart, is a key diagnostic tool for examining the anatomy of the heart and its pumping function. With this examination it is possible to ascertain findings such as enlarged heart chambers or heart valve malfunctions and areas of scarring in the heart muscle after one that has expired Heart attack to represent.
Stress echocardiography
In stress echocardiography, the patient is loaded with medication and wall movement disorders that occur due to insufficient supply of the heart muscle under this load can be revealed.
Does a myocardial scintigraphy of the heart make sense?
Myocardial scintigraphy is one of the imaging procedures and is a nuclear medical examination that can be used to identify scars and areas of the heart muscle that are under-supplied. With their help, the metabolic activity of heart muscle cells can be displayed and a statement about the vitality of the heart can be made.
The method is particularly suitable for showing the exact cause of a reduced metabolism in the heart muscle. If the cause is a previous heart attack, there is no sufficient metabolism in the tissue either at rest or during exercise.
If the cause lies in the coronary arteries, the metabolism is normal at rest. A reduced metabolism is only found during exercise due to the reduced blood flow. A distinction can be made between a previous heart attack and CHD.
Read more on this topic at: Scintigraphy
Cardiac catheter / coronary angiography
Coronary angiography (Cardiac catheter) represents the so-called "gold standard" in the diagnosis of coronary heart disease. It is currently the best and most efficient method for diagnosing CAD.
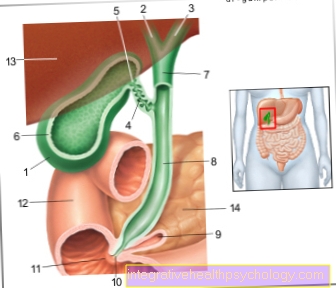
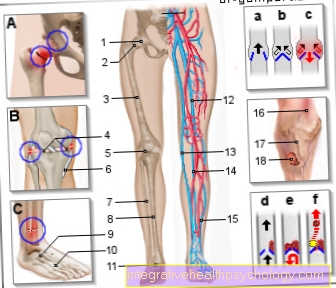
The shape and shape of the coronary arteries is examined by means of a catheter, usually pushed through the inguinal artery (directable tube) and associated X-ray examinations with administration of contrast medium. Occlusions or narrowing of the cross-section of the coronary arteries can be detected, but this does not provide direct evidence of an oxygen deficiency (ischemia). If the degree of occlusion of an artery is more than 90% or if wall movement disorders are recognizable in the x-ray, it can indirectly be concluded that the associated supply area is insufficiently supplied.
Coronary angiography is used to confirm a suspected CHD and to exclude or prove a coronary heart disease in a clinically ambiguous situation.
In addition, it is possible to immediately follow the diagnostic procedure with the therapeutic procedure: balloon dilation, i.e. An expansion of the constricted or closed vessel, or a stent insertion to keep the coronary artery open are possible and the success of the intervention is checked and documented immediately after the implementation by means of an X-ray.
What is coronary CT angiography?
Coronary CT angiography is based on the technique of computed tomography (CT). So there are layered images of an organ recorded. This technique works by means of X-rays and is carried out in a CT tube.
An angiography is a special representation of the vessels. By means of a contrast medium, which is particularly noticeable in the CT, the blood flow situation of various vessels can be shown.
If the blood flow in a vessel is not permeable, this can be an indication of calcification, for example. The coronaries are the coronary arteries.
Coronary CT angiography is therefore the specific representation of the coronary vessels using computed tomography.
Read more on this topic at: Angiography of the heart
Does an MRI of the heart make sense in coronary heart disease?
An MRI (magnetic resonance tomography) is a cross-sectional imaging procedure in which the organs can be assessed in their three-dimensional arrangement. It is not of paramount importance for the diagnosis of coronary heart disease (CHD). This is mainly due to the fact that if a CAD is suspected by an MRI, a cardiac catheter must still be performed, which finally proves the disease. For people for whom the catheter is considered to be a potentially critical procedure, an MRI will still be performed beforehand. In this way, a CAD can be excluded or the urgent need for a cardiac catheter can be shown.
Read more on this topic at: MRI of the heart