Inflammation of the intervertebral disc
definition
In the Disc inflammation, also Discitis called, it is an inflammation of the intervertebral discs. Most of the time they too neighboring vertebral bodies are affected, one speaks of a Spondylodiscitis. The Band washers are the cartilaginous bodies that lie in the spine between the individual vertebral bodies. There reduce the mechanical stress and Steaming for example the Impact loading while walking. In addition to pain, inflammation leads to progressive damage to the affected tissue with degeneration of the spine.

causes
There are various causes for inflammation of the intervertebral disc apparatus. For one thing, a endogenous (coming from the body itself) Infection with bacteria, Viruses or Mushrooms spread to the intervertebral discs and thus lead to inflammation.
Another possibility is that these pathogens are the result of a Intervention, so about one Surgery to the spine or by injections can penetrate into the intervertebral discs in this area. In many cases, however, a specific pathogen detection is not possible, one then speaks of the so-called Fugax spondylitis.
Diagnosis of inflammation of the intervertebral disc
Making the diagnosis of disc inflammation is not always easy, especially because of what the examination suggests Symptoms vary widely can be.
Sections of the chest- or Lumbar spine. Here you can Knocking pain and Tenderness occur. The mobility of the corresponding segment can be severely restricted or completely intact. But usually there is one Cramping of the surrounding muscles ascertain. Often there will be pain when Back straightening up described from diffraction. There are usually no outward signs of inflammation. In any case it should be a complete neurological examination be done to any Nerve damage to recognize.
Increased infection levels in the Laboratory examination can be another clue.
The damage to the vertebral bodies and intervertebral discs, if it is already pronounced, can easily be seen in the X-ray image represent. However, this damage does not occur until later in the course of the disease.
Appointment with a back specialist?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The spine is difficult to treat. On the one hand it is exposed to high mechanical loads, on the other hand it has great mobility.
The treatment of the spine (e.g. herniated disc, facet syndrome, foramen stenosis, etc.) therefore requires a lot of experience.
I focus on a wide variety of diseases of the spine.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at Dr. Nicolas Gumpert
Typical are there Resolutions and Changes of the Base and cover plates of the Vertebral bodies.
A more precise imaging and delimitation of possible other clinical pictures should most likely by means of Magnetic resonance imaging (MRI) respectively. By means of this imaging, a Damage to neighboring nerves, of Spinal canal or the formation of Abscesses or Edema best captured.
If an MRI (magnetic resonance imaging) is not possible, for example because of a Pacemaker, can also be a CT Investigation. A definitive confirmation of the diagnosis and, above all, the pathogen detection, which is important for antibiotic treatment, can then be carried out by means of a puncture. Alternatively, the pathogen can be detected with the help of a blood culture.
frequency
The disc inflammation presents with a Frequency of about 1 in 250,000 in Germany a very rare disease The mortality is up to 10% for very severe courses.
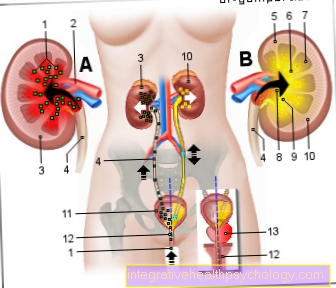
In principle, patients can become ill at any age, but the frequency peak is in the 5th to 7th decade of life. There is also an increase in disc inflammation in patients who are under Diabetes mellitus, Autoimmune diseases, Renal failure, Inflammation of the liver, Cancers or alcoholism Suffer. Men are three times as likely to be affected as women.
Symptoms
In principle, the severity of the inflammation of intervertebral discs and vertebral bodies varies enormously.
So the spectrum ranges from symptom-free coursesthat are only noticed as incidental findings, up to the most severe pain. The pain mainly occurs at rest and at night. In addition to the locally limited pain in the back area General symptoms, how fever, Exhaustion, chills or increased signs of infection in the laboratory occur. Also Neck tension or Sciatica pain can be an indication of a disc inflammation. Usually the mobility of the spine is limited.
Irritation of the nerve roots occurs less often, but this then increases strongest neuropathic pain and neurological failure symptoms being able to lead. If due to the inflammation a epidural abscess, so one Liquid accumulation forms in the area of the membranes of the spinal cord, which then presses on the spinal cord, it can even cause symptoms Paraplegia come.
Another inflammation in the area of the spine, which must be distinguished from the inflammation of the intervertebral disc, is the inflammation of nerve roots, i.e. at the points at which the nerves emerge from the spinal cord. It can have symptoms very similar to the inflammation of the disc.
Inflammation of the intervertebral disc in the lumbar spine
The Lumbar spine (Lumbar spine) is a frequently affected area when the intervertebral disc is inflamed. Due to the inflammation in the lumbar vertebrae, bending, lifting, straightening and sitting are often a painful affair for those affected. With a deep corset the movements of the lumbar spine can be restricted as far as possible. Therapy must take place as early as possible with the help of antibiotics, otherwise the inflammation can spread to the abdomen and pelvic organs. In rare cases, the nerves in the lumbar spine can also come out of the Spinal cord leak, be affected. They are responsible for motor and sensitive tasks in the legs. If they are damaged, the deficiency symptoms can be felt along these nerve fibers down to the legs and feet.
Inflammation of the intervertebral disc on the cervical spine
The Cervical spine in the human body is a very sensitive area. Inflammation of the intervertebral disc at this level leads to extreme conditions for those affected severe restrictions. The cervical spine moves very strongly in everyday life and the movement in the cervical spine is involuntarily carried along with almost every eye movement. If the intervertebral disc is inflamed, this pain can be felt permanently. A Ruff can stabilize the neck during the treatment and restrict freedom of movement.
The antibiotic therapy in the case of inflammation of the intervertebral disc in the cervical spine is extremely important, as otherwise the bacterial pathogens can spread and spread to surrounding organs. There are some vital pathways and organs in the neck in particular.
therapy
In the treatment of uncomplicated disc inflammation there is one Antibiotic care and a Immobilization of the affected area in the foreground. In addition, a supply of Pain relievers and anti-inflammatories (anti-inflammatory) Substances.
If there are already nerve damage or signs of entrapment, or if the infection cannot be managed in any other way, must operational Be treated.
Conservative therapy
The main component of conservative therapy for disc inflammation is an antibiotic treatment lasting several weeks. Except in emergencies, e.g. in the case of a septic course, always only after identification of the pathogen and resistance testing. This is supplemented by resting in bed for several days.
Then the affected area should be stabilized for several weeks with a corset or an orthosis to prevent further irritation.
If the disc inflammation affects the area of the lower lumbar spine, a considerably longer bed rest of approx. 6 - 12 weeks is necessary, as immobilization cannot be achieved otherwise. Therefore, the operative approach is often preferred here. The total duration of treatment can extend over a period of up to a year.
If after 4-6 weeks of conservative therapy there is no osseous build-up in the affected area, or the infection persists, an operation is usually necessary.
Medical therapy
Treatment of inflammation of the intervertebral disc must be largely medicated. A distinction must be made between causal and symptomatic therapy. Both should be done, the former being indispensable in the treatment of disc inflammation.
The main cause of the inflammation is a settlement of bacterial pathogens. These are often persistent and continue to spread in their surroundings. Serious ones develop over time Inflammatory settlements and in the worst case, colonization of the blood and life-threatening complications. To curb bacterial inflammation, you need to Antibiotics can be used. There are antibiotics that have a very broad effect against a large number of pathogens. In particularly acute cases, these are used first. However, they have disadvantages compared to targeted agents, since a pathogen-specific antibiotic works better and less often leads to the development of resistance in bacteria.
With the help of Blood samples and also Tissue samples the causative pathogens must be obtained and identified from the intervertebral disc. Only then can the most suitable antibiotic be selected and administered. In the hospital, this is mainly administered intravenously via a infusion given, as more active ingredient reaches the intervertebral disc and lower doses are necessary. If the intervertebral disc becomes inflamed, the intravenous antibiotic must in many cases be administered for up to 4 weeks. The entire therapy takes several months.
In addition to antibiotics, they are also used in the treatment of disc inflammation Pain medication for use. Due to the long healing time, the pain must be made as bearable as possible. Initially, naturopathic remedies can be used. For moderate pain, drugs from the group are more likely to be NSAIDs used, for example Ibuprofen or Diclofenac. If the pain is extremely severe, opiates can also be given, for example Morphine.
homeopathy
The homeopathy represents an alternative medical approach to healing in which it is not a disease that is to be treated, but the holistic person. Homeopathic remedies are highly diluted active ingredients, for example in the form of Globuleswhich are supposed to stimulate the body's self-healing powers when taken. In the case of acute inflammation of the intervertebral disc, the globules can be used as Supplement to the antibiotics are used. It is extremely important to take antibiotics for this condition. In this case, the globules do not represent an independent therapy alternative. They can only support the inner healing powers when the inflammation subsides and the pain is processed.
Operative therapy
in the chest- or Lumbar region Both surgical and conservative therapies are possible, im Sacral area an operation is always indicated.
On the one hand, this is the aim of operative care Clearing out the source of infection (Wound debridement), on the other hand one Stabilization of the spine.
The stabilization takes place by means of a so-called Spinal fusion, partly with additional Implantation of bone tissue, e.g. from the Iliac crest. Individual vertebral bodies are connected to one another using screws and plates, or replaced by titanium implants.
After the operation, the spine is naturally mobile partially or completely restricted. In general, surgical treatment can be carried out either in one operating theater or in two rounds. In the latter case, only the infectious tissue is removed first and then, after a brief healing phase, in a further surgery to stabilize the spine.
The exact surgical method depends on the extent of the damage and the patient's condition. The intervention can either be carried out from the front, i.e. via the abdomen as an access route, or from the back.
Overall, the surgical procedure has the advantage that the Time to complete immobilization shortened can be. In conservative therapy, this particularly harbors the risk of a Degeneration of the holding muscles and the formation of so-called Pseudarthroses (wrong joints) with misalignments of the spine.
This also increases with long bed rest thrombosis Risk. However, immobilization of about 8 weeks is necessary even after the operation until the wound has healed sufficiently. In addition, further treatment with antibiotics should be carried out for approx. 12 weeks.
prophylaxis
General behaviors or preventive measures to protect yourself from an inflamed disc there is not any.
In principle, any serious infection can lead to the pathogen sown into the intervertebral discs. The risk of infection of the Abdomen, of Genitourinary tract or des Basin especially high. To prevent infection around a surgical procedure is sterile work mandatory requirement. However, even under the best of conditions, a Wound infection never be excluded.
In order to recognize an unnoticed recurring disc inflammation at an early stage, one is necessary in the first time after the treatment regular laboratory examination, as well as a X-ray control recommended for the spine.
forecast
Regardless of the therapy, destructive spinal changes and the resulting neurological restrictions, such as disorders of feeling or motor skills, remain in many patients. These can also be associated with a severe reduction in the quality of life. Overall, these limitations are somewhat less pronounced in patients who received surgical treatment. The risk of relapse (Recurrence) of the disc inflammation is up to 7%.
An inflammation of the intervertebral disc can be fatal only in very severe cases with sepsis.