Fournier gangrene
Definition - What is Fournier gangrene?
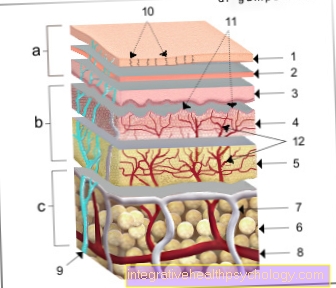
Fournier gangrene is a special form of necrotizing fasciitis and occurs in the genital, perineal and anal regions. This leads to a bacterial infection, which in turn triggers an increased circulatory disorder and leads to the death of the skin.
The bacteria spread within the fascia (fasciitis) and can get into the blood system and trigger a systemic reaction there. Fournier gangrene is an absolute emergency and should be treated as soon as possible. Despite therapy, Fournier gangrene is associated with mortality (mortality) of over 20-50%.

causes
Fournier's gangrene is caused by an infection with, usually anaerobic bacteria such as streptococci, Escherichia coli or clostridia. Anaerobic bacteria multiply in oxygen-free areas and are very sensitive to the presence of oxygen.
Possible sources of infection are above all the anal region, the skin and the urinary tract. From there, the bacteria spread through the fascia and reach the genitals. Men are significantly more likely to suffer from Fournier gangrene than women.
The infection leads to a thrombosis (blockage) of the superficial blood vessels, which in turn leads to an insufficient supply of oxygen.
Rapidly progressing gangrene occurs, followed by death (necrotizing) of the skin. The bacteria often form so-called toxins (poisons) and release them.
The bacteria can also spread into the blood system, which can lead to sepsis (systemic blood poisoning). Risk factors for Fournier gangrene are diabetes, a weakened immune system, chronic alcohol consumption, smoking and being overweight.
How contagious is Fournier gangrene?
Fournier's gangrene is a disease of the genital organs, but not a typical sexually transmitted disease. In contrast to typical sexually transmitted diseases such as chlamydia, syphilis or AIDS, Fournier gangrene is not transmitted through sexual intercourse.
The infection usually occurs from the body's own regions or, for example, by injections. However, since Fournier gangrene is a bacterial infection, it should always be treated with caution.
Mostly they are harmless pathogens that belong to the natural bacterial flora of humans. In principle, however, infection with atypical pathogens is also possible and can be dangerous for contact persons.
diagnosis
Since Fournier gangrene causes the infection to spread and progress quickly, a so-called visual diagnosis is usually possible. This means that the doctor in question only has to take a look to make a suspected diagnosis.
Even in doubtful cases, the doctor will initiate immediate therapy. The reason is the high mortality (mortality) of Fournier gangrene, which is why complex diagnostics take up valuable time.
A blood sample is always part of the diagnosis to see how far the infection has progressed or whether septic parameters can already be determined. A smear of gangrene is also taken in order to classify the relevant pathogen and to find an optimal antibiotic.
How is the transmission route?
The bacterial infection in Fournier gangrene can occur in different ways. One possibility is that the bacteria enter the tissue through small wounds in the skin and multiply there. A transfer of bacteria naturally occurring in the intestine (e.g. Escherichia Coli) to the perineum or genital region is also possible.
Another option is a urinary tract infection, such as a bladder infection. An infection of the anal or urethral glands often occurs. There the bacteria multiply and then spread along the fascia boxes.
Concomitant symptoms
Fournier gangrene is always associated with skin changes in the form of redness, swelling, livid discoloration, severe pain or a bad smell.
In the early stages it can also cause itching in the genital area. In Fournier gangrene, especially in the later stage, there is also a high fever, increased heart rate and a poor general condition.
The reason is the systemic reaction and the secretion of bacterial toxins (poisons). This can also lead to symptoms of shock. This means that the patient compensates for a blood pressure that is much too low with an increased heart rate.
This can lead to unconsciousness, paleness, feeling cold, tingling in the limbs, organ failure, or death. The infection can also be transmitted to other organs.
Treatment and therapy
The therapy of Fournier gangrene consists of several parts. Treatment as quickly as possible is important. Too much time is often lost in a doctor-patient consultation.
How early a therapy is given depends strongly on the outcome of the disease.
Fournier gangrene is treated with a broad-acting antibiotic. The reason is that at this point you do not yet know which bacteria caused the infection. Therefore, the gangrene will also be smeared.
The next step is an immediate surgical "debridement". This means that the already necrotic (dead) areas are generously removed so that only healthy tissue remains.
The success of the therapy is usually decided at this point, since complete removal is often no longer possible due to anatomical conditions. If the debridement is successful, a skin graft may be necessary at intervals.
In any case, patients with Fourner's gangrene should be strictly monitored by intensive care medicine.
How is the process?
After therapy in the form of surgical debridement and antibiotic therapy, the patient will continue to be closely monitored. The first step towards successful treatment is to prevent or treat any systemic inflammation (sepsis) that may be present. This can take up to several days and require intensive medical care.
The complete removal of the infectious and necrotic areas is also essential for a successful therapy. If the result is a large loss of skin area, a skin transplant may be necessary. However, this is carried out at intervals. This means that the skin would only be covered when the patient is stable and physically fit again for another operation and the transplant is likely to be successful.
Overall, the course of Fournier gangrene can be very variable. Whether the treatment is successful is primarily determined by timely therapy and uncomplicated surgical interventions. The presence of risk factors such as diabetes, a weakened immune system, alcohol, smoking and being overweight can also have a negative effect on the course.
Duration of healing and prognosis
Despite therapy, Fournier gangrene is associated with a mortality rate of 20-50%. If left untreated, such gangrene is an absolutely fatal disease.
The early start of medical therapy is particularly important for the prognosis. Especially when there are changes in the genital area, patients go to the doctor much too late because the situation is uncomfortable for them.
Other important prognostic factors are whether complete surgical debridement is possible and whether the respective antibiotics are effective. A weakened immune system, for example through suppression with cortisone, has a rather bad effect on the prognosis.
Furthermore, the presence of a systemic reaction and the presence of risk factors play an important role. These are also particularly crucial for the successful growth of a skin graft.
Should a Fournier gangrene go well, the healing time depends on the need for a skin covering, which means a renewed intervention in the interval. It is possible that Fournier gangrene will heal itself after a few weeks or that it will still cause problems after months.





















.jpg)