Hormone therapy for breast cancer
definition
There are a number of ways to fight a tumor disease, one of which is hormone therapy.
Breast cancer is often linked to hormones, so that hormone therapy can be used to influence the hormonal balance. Among other things, this can result in slower growth.

Forms of hormone therapy
These are the different types of hormone therapy:
- Additive hormone therapy: Here, hormones are supplied to the body with the aim of slowing down or even stopping tumor growth. Mostly one uses an opponent to the hormone of the originally affected organ (example: estrogen administration in prostate cancer).
- Ablative hormone therapy: The therapy consists in withdrawing hormones from the body. This is most likely done by surgical removal of the hormone-producing organ or with the help of medication. The aim of this therapy is also to stop the growth of the tumor by stopping the hormonal growth stimulus.
- Therapy with hormone antagonists: Here no hormones are added or organs removed, but the effect of the hormones is blocked. It does this either by inhibiting hormone production or by inhibiting the target organ or hormone receptor.
Read more on the topic here: hormone preparations
When does hormone therapy make sense for breast cancer?
Hormonal treatment for breast cancer is recommended if the tumor has hormone receptors.
Approx. 75-80% of patients have breast tumors that are sensitive to hormones. Various studies have shown that these patients benefit greatly from hormone therapy in all stages. Depending on the stage, however, additional measures must be taken, for example switching off the ovarian function, in order to ensure successful therapy.
In pre-menopausal patients with stage I or IIA breast cancer, anti-hormonal therapy alone can be considered if chemotherapy cannot be performed.
Treatment with anti-hormonal drugs is also recommended for people with metastatic breast cancer. This therapy leads to an extension of the survival time and in 20% to 30% of the cases to a remission. Compared to classic chemotherapy, the tumor-free time is also longer. Hormone therapies also usually have fewer undesirable side effects than classic chemotherapy.
Which hormone therapy should be used depends, among other things, on the stage of the disease and the tolerance of the drug. Anti-hormonal therapy usually takes several years. Before menopause, therapy should be followed for at least 5 years; Therapy lasts 4 to 10 years after the menopause.
Patients whose tumors do not have hormone receptors benefit little if at all from such a treatment and should therefore not receive any hormone therapy.
Find out more about the topic here: The different therapies for breast cancer
Why is hormone therapy also useful after breast cancer?
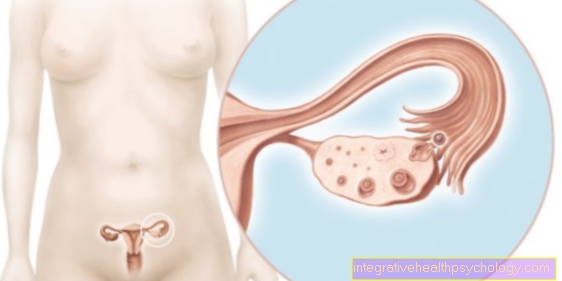
In tumors that have hormone receptors, the estrogen produced by the body causes the tumor to grow more quickly. In order to prevent or slow down growth, the hormone production must either be stopped (by irradiation or removal of the ovaries) or the effect of these hormones must be prevented.
Hormone therapy can, depending on the active ingredient, reduce both the formation of the hormones and their effect. Hormone therapy can therefore be used to slow down tumor growth or, for example, prevent tumors from recurring after removal of the tumor.
If the tumor has been successfully removed, anti-hormonal therapy is recommended to reduce the risk of recurrence (recurrence of the tumor). As a rule, such treatment lasts 5 years, although studies have shown that a treatment of 10 years should lower the risk of recurrence even more and thus increase survival time.
Patients who fall ill after the onset of menopause are sometimes at an increased risk of the recurrence of tumors and are therefore particularly at risk. It is advisable to carry out hormone therapy in order to prevent a relapse.
Hormone therapy after breast cancer is cured is therefore an important part of the treatment and is intended to extend the patient's survival time.
Also read:
- Follow-up care for breast cancer
- Breast cancer recurrence
What hormone therapies are there?
Hormone therapies can be effective at different points in the hormone control loop. For this reason, a distinction is made between three large groups of active ingredients:
- Antiestrogens
- Aromatase inhibitors
- GnRH analogs
Anti-estrogens like Tamoxifen are also called Selective Estrogen Receptor Modulators (SERMs for short). These active ingredients do not inhibit hormone production, but they do block the receptors on the target organs. As a result of this blockage, estrogens can no longer bind to the receptor, causing the cells to lose their growth stimulus. As a result, the tumor cell can no longer divide and growth is stopped.
As an alternative to tamoxifen, one can also use it at an advanced stage Fulvestrant deploy. Fulvestrant is stronger than tamoxifen in its effects. It not only reduces the hormone activity to a minimum, but switches it off completely and leads to the breakdown of the receptors.
A second class of active ingredients are aromatase inhibitors.This group of drugs bind to the so-called aromatase enzymes and thereby disrupt the conversion of estrogen precursors into estrogen. As a result, the estrogen level drops and the tumors lose the hormonal growth stimulus. However, aromatase inhibitors are only used in post-menopausal women, since aromatase only has a decisive effect on estrogen production from this point on.
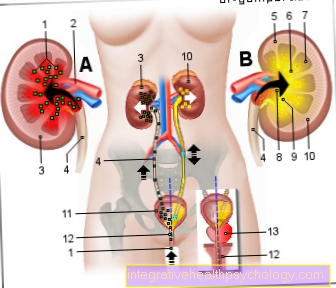
In addition to antiestrogens and aromatase inhibitors, GnRH analogues are used. GnRH (Gonadotrophin-releasing hormone) is a hormone that works in the brain. It binds to receptors on the pituitary gland (Pituitary gland) and causes the release of hormones (follicle-stimulating hormone (FSH) and luteinizing hormone (LH)), which in turn stimulate the production and release of estrogen. GnRH analogues are similar in structure to the body's own GnRH, so they bind to the same receptors, but do not cause any hormone release. In this way, the hormone supply to the tumor is cut off and its growth is stopped.
What are the side effects of hormone therapy?
Various side effects can occur depending on the active ingredient.
Side effects of antiestrogens
Antiestrogens such as tamoxifen or fulvestrant typically cause menopausal symptoms because they prevent the estrogen from working.
Which includes:
- Hot flashes
- sleep disorders
- nausea
- Vaginal dryness
- Difficulty concentrating
- Sweats
- depressive moods
- Loss of libido
- Itching and bleeding around the vagina
- thrombosis
In addition, the lack of effect of the estrogen can lead to increased growth of the uterine lining and in rare cases to uterine lining cancer.
The side effects of fulvestrant are usually less severe than those of tamoxifen.
Also read: Menopause symptoms
Side effects of aromatase inhibitors
The side effects include:
- Menopausal symptoms (but less often thrombosis or uterine lining degeneration)
- Discomfort in the musculoskeletal system, e.g. Muscle and joint pain (Myalgias and Arthralgia)
- Decrease in bone density, increased fragility, osteoporosis
To reduce the risk of bone fractures, the bone density should be checked regularly and, if necessary, vitamin D and calcium should be taken to strengthen the bone structure.
Side effects of the GnRH analogues
GnRH analogues intervene in the hormone control loop and also have some side effects:
- Menopausal symptoms
- decreased bone density, increased fragility (osteoporosis)
Weight gain
One side effect of hormone therapy is weight gain.
This is one of the typical menopausal symptoms and can be a burden for patients.
The weight gain can result from an increased appetite or from water retention in the tissue (edema). The changes in weight can also be based on the influence of the anti-hormonal treatment on lipid metabolism. The aromatase inhibitors in particular lead to weight gain.
For this reason, regular exercise is recommended to stabilize the weight.
Benefits of hormone therapy
Hormone therapy has many advantages:
- In contrast to chemotherapy, it does not attack healthy cells. The antihormonal therapy deprives both sick and healthy cells of their hormone supply, but does not cause them any direct damage. After discontinuing therapy and removing diseased cells, the healthy cells can function normally again.
- No lengthy hospital stay as most of the active ingredients can be taken in the form of tablets.
- In general, antihormonal therapy has few side effects and is therefore better tolerated than classic chemotherapy.
- It should also be noted that fertility can be maintained after discontinuing hormone therapy.
Disadvantages of hormone therapy
Hormone therapy has several disadvantages. These include, for example, the very long duration of treatment. As a rule, anti-hormonal therapies must be followed for 5 to 10 years. This is due to the low level of aggressiveness of this form of treatment.
Another disadvantage of hormone therapy can be temporary menopausal symptoms.
Duration of therapy
In contrast to classic chemotherapy, hormone therapy usually lasts several years. The reason for the long duration of treatment is the non-aggressive and indirect effect of hormone therapy.
Usually the duration of treatment is 5 years, in some cases up to 10 years. Even after successful treatment, the continuation of the therapy is sometimes recommended, as this can significantly reduce the risk of tumor recurrence. This prevention is usually done for 5 to 10 years as well.
All in all, hormone therapy takes a very long time and requires adaptation to life or a certain discipline when it comes to taking medication (at least for preparations in tablet form).
How do you deal with a desire to have children during hormone therapy?
Hormone therapies lead to a transient menopausal condition and prevent pregnancy. However, this condition can be reversed after successful treatment, as hormone therapy does not cause any damage to the ovaries.
However, women who are about to enter menopause at the start of treatment have an increased risk of losing ovarian function as a result of treatment. If there is an unfulfilled desire to have children, this should be discussed with the treating doctor at the beginning. Depending on the degree of the disease, the therapy can be adapted to the desire for children. In addition, measures can be taken to maintain the patient's fertility.
If therapy has already started, stopping the medication on your own does not make sense and should only be discussed with a doctor.
After completing the treatment, there is usually no need to take a break until the time of pregnancy. However, it can take some time before the ovaries are fully functional again.