Impingement Syndrome
Synonyms in a broader sense
- subacromial tight syndrome
- Shoulder constriction syndrome
- Shoulder bottleneck
- Shoulder bottleneck syndrome
- Impingement Syndrome
Gender distribution
The gender distribution in impingement syndrome is roughly balanced between women and men.
definition
Narrowing of the sliding space for the tendons of the rotator cuff muscles and the bursa between the humerus head and the shoulder roof.
Impingement syndrome is a functional impairment of the shoulder joint that can arise as a result of chronic overload, for example in tennis or golf players, swimmers or throwers.
Often, however, one cannot identify the actual cause that triggers the disease. In these cases there is a constriction under the shoulder roof due to the nature of the structure.

introduction
The impingement syndrome is referred to as shoulder bottleneck syndrome and is one of the most common diseases in the shoulder and shoulder joint. People who do sports or jobs that require overhead movements or overhead work are particularly affected. Depending on the cause, a distinction is made between a primary impingement syndrome and a secondary impingement syndrome. In the primary form, the problem lies in a narrowed space between the roof of the shoulder and the humerus head (subacromial space). Possible causes are wear and tear of the shoulder joint (omarthrosis), inflammation in the area of the bursa and / or the shoulder-stabilizing muscle groups (rotator cuff), calcium deposits in the area of tendons and muscles, protruding bones (bone spurs) and an anatomically unfavorably shaped shoulder roof. The secondary form is used for bony misalignments of the spine (especially in the neck and chest area), muscular imbalances (muscle imbalances) and stability problems of the shoulder as a result of sports injuries or accidents. Ultimately, both soft tissues and structures (e.g. tendons or muscles) in the subacromial space are narrowed, which significantly restricts their mobility. This then ultimately leads to pain and significant restrictions on movement of the shoulder and shoulder joint.
You might also be interested in: Spinal disorders
Age
The disorder typically occurs around that 50 years of age on.
Appointment with a shoulder specialist

I would be happy to advise you!
Who am I?
My name is Carmen Heinz. I am a specialist in orthopedics and trauma surgery in the specialist team of .
The shoulder joint is one of the most complicated joints in the human body.
The treatment of the shoulder (rotator cuff, impingement syndrome, calcified shoulder (tendinosis calcarea, biceps tendon, etc.) therefore requires a lot of experience.
I treat a wide variety of shoulder diseases in a conservative way.
The aim of any therapy is treatment with full recovery without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- Lumedis - your orthopedic surgeon
Kaiserstrasse 14
60311 Frankfurt am Main
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
You can find more information about myself at Carmen Heinz.
frequency
It is assumed that approx. 10% of the population suffer from pain-related movement restrictions of the shoulder.
causes
Simplified are shown at the emergence of a Impingement Syndrome three components involved. These are:
- the humerus head
- the shoulder roof (formed from the acromion and ligamentum acromio-acromiale)
- the rotator cuff with the subacromial bursa
Changes in one or the combination of several components can be possible causes for the development of an impingement syndrome:
- Overweight of the upper arm lifting muscle groups and the resulting rise of the humerus head
- Incorrectly healed fractures on the head of the humerus
- Thickening of the tendon on the rotator cuff due to excessive strain and / or exercise
- Increase in the volume of the tendon and the bursa due to chronic inflammation
- Calcium deposits in the tendon
- Bony protrusions on the lower surface of the acromion
- Arthrosis of the shoulder joint (AC joint)
- Unfavorable shape variants of the acromion that deviate from the norm, for example with the tip angled downwards
While Injuries Occurring at a young age primarily in the course of acute trauma, ruptures of the rotator cuff in older ages (over 40 years) are often the result of chronic degenerations, i.e. wear and tear on the tendons. The supraspinatus tendon is most commonly affected. It often affects people who work or act a lot with their arms above their heads. That can go through sport activity (Volleyball, handball, throwing sports and bodybuilding) or work-related (Painter, mechanic).
Holding the arm overhead narrows the subacromial space. Through the Narrowing (Impingement) the tendon of the supraspinatus muscle is pressed, irritated and rubbed through over time, so that in the worst case, the tendon can rupture or partially tear. But before that usually occurs Inflammatory process the tendon that closes Fluid retention and the smallest calcifications. If there is a rupture of the supraspinatus tendon, different treatments are available.
System-related tightness between the shoulder head and the shoulder roof
A constraint-related tightness between the shoulder head and the shoulder roof can have various causes. In addition to primary and secondary osteoarthritis, an anatomically poorly shaped shoulder roof can also lead to problems. This then has to be reshaped by means of an operation so that the structures and soft tissues underneath can move again without disruption.
In both cases, the subacromial space is narrowed, which significantly restricts tendons and muscles in their mobility. Calcium deposits in the shoulder area can also lead to an impingement syndrome. This so-called calcified shoulder primarily affects the tendons of muscles (mostly the supraspinatus tendon). The cause of the limescale formation has not yet been fully clarified. It is assumed that the muscle-stabilizing muscle groups and their tendons have insufficient blood flow, which is e.g. can be triggered by a fall on the shoulder. Reactive calcium deposits occur in the area of the tendons, which thicken and become inflamed if the irritation persists (see also: tendinitis).
Read more on the topic: Inflammation of the shoulder blade
Osteoarthritis of the shoulder joint
Arthrosis of the shoulder joint (omarthrosis) can be a cause of impingement syndrome. In general, osteoarthritis is a mostly age-related change in the articular cartilage caused by wear and tear. In addition, a distinction is made between primary osteoarthritis and secondary osteoarthritis. In the primary form, the age-related wear and tear of the articular cartilage is in the foreground, and in the secondary form, accidents or various diseases lead to pathological changes in the shoulder.
In both cases, the cartilage thickness between the humerus head and the shoulder socket (glenoid) decreases in the area of the shoulder joint, which significantly narrows the joint space between them. Due to the lack of cartilage mass, both bones rub against each other.
The result is increasing pain and significant restrictions on movement in all areas of the shoulder joint, the pain initially occurring when moving or lying on the shoulder. As the disease progresses, these also occur in a resting state. In the worst case, osteoarthritis of the shoulder joint can lead to a frozen shoulder (“frozen shoulder”) or to a complete joint replacement.
Thickening of the bursa and tendon
Thickening of the bursa and tendons occur in inflammatory processes or in the case of constant incorrect or excessive stress. Bursae are structures filled with fluid that help reduce friction and pressure in areas that are particularly exposed to mechanical stress. If an inflammation occurs, e.g. As a result of an impingement syndrome, these produce increased amounts of fluid and swell, causing the muscles and tendons in this area to become trapped, which leads to severe pain, overheating of the shoulder and restricted mobility. Thickening of the tendons can occur due to a calcareous shoulder, due to an impingement syndrome or also due to a bursitis. As a result of the increase in size, they can no longer slide smoothly, which results in pain and poor mobility.
Injury to the shoulder
Sports injuries or accidents in the shoulder area can cause impingement syndrome. Especially dynamic sports such as Handball or volleyball, which requires overhead movement, pose a high risk. Tears in muscles or tendons, dislocation of the shoulder (shoulder dislocation) and falls on the shoulder joint are particularly common. Accidents such as A bicycle or car accident can also lead to various illnesses or fractures, which is associated with severe pain and significant restrictions on movement in the shoulder and shoulder joint.
Duration
Impingement is usually a process of over years arises. Due to the chronic inflammatory process, one slowly but steadily forms Narrowing under the Shoulder roof (Fornix humeri). At a certain point, this bottleneck becomes so painful and problematic for those affected that they seek medical treatment. By Medication, physical therapy, Ultrasound, heat and cold, electrotherapy and other approaches can be treated conservatively. As it takes time for the inflammation to get out of the subacromial Space is eliminated, it can up to 3 months take until complete freedom from symptoms is achieved. However, this also depends on how long the inflammation has existed and how severe the damage is that has occurred. It is quite possible that after 3-4 months of conservative therapy you will surgical intervention must be carried out. Then, ideally, the symptoms will be gone after 4-6 weeks of follow-up treatment.
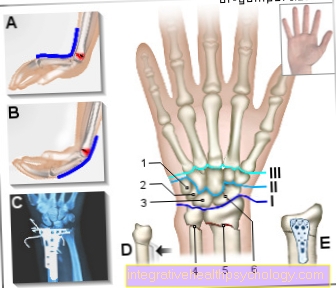
Figure impingement syndrome
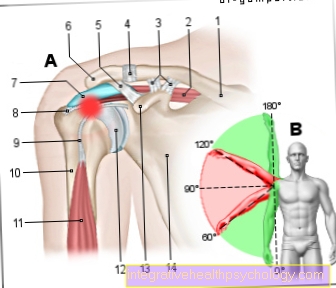
Impingement syndrome (shoulder)
(Narrowing, crushing of the tendons)
- Collarbone - Clavicle
- Upper bone muscle -
Supraspinatus muscle - Raven beak collarbone ligament -
Coracoclavicular ligament - Shoulder and collarbone
steer -
Articulatio acromioclavicularis - Raven beak shoulder band -
Coracoacromiale ligament - Shoulder corner - Acromion
- Bursa -
Subacromial bursa - Supraspinatus tendon
(Upper bone tendon) - Tendon of the long biceps head
- Upper arm shaft - Corpus humeri
- Two-headed upper arm muscle (biceps),
long head -
Biceps brachii muscle, caput longum - Humerus head -
Caput humeri - Raven beak process -
Coracoid process - Shoulder blade - Scapula
You can find an overview of all Dr-Gumpert images at: medical illustrations
Symptoms of Impingement Syndrome
If a patient has a well-founded suspicion of impingement syndrome, he usually complains of moderate to severe shoulder pain even in the early stages of the disease. In the early stages of impingement disease, pain is almost exclusively movement-dependent.
This can usually be triggered by the so-called painful arch.
Read more on the subject below: Shoulder Neck Pain - What You Should Know About It
With this phenomenon, which is also known as "painful arc", there are initially no symptoms when the arm is raised at a 90 degree angle. This is due to the fact that there is usually still sufficient space in the shoulder roof and the muscles in the shoulder joint are not restricted.
If the arm is raised over an angle of about 60 degrees, the space in the shoulder area becomes increasingly narrow and the pain begins. If the arm is raised further to the side and reaches over 120 degrees, the space in the shoulder area increases again and the pain decreases again.
The classic alternation between freedom from symptoms, pain and renewed freedom from symptoms when the arm is raised piece by piece already speaks very strongly for the presence of an impingement syndrome, since no other orthopedic disease has such a characteristic pain development
Is it a advanced impingement syndrome, the space in the shoulder area is already so narrow that even the smallest movements in the arm area lead to discomfort.
With especially pronounced impingement syndromes so-called resting pain can also occur. The shoulder pain at night, which is more often worse than that during the day, is particularly typical.
With advanced impingement syndromes there is also nocturnal pain, especially when the patient lies on the diseased shoulder. In this case, severe pain can also occur even if the arm is not moved.
In addition to the classic arm lift, which leads to the symptoms of impingement described, it can also happen that a Arm rotation pain to be triggered. A rotation in the shoulder joint is understood to mean a External rotation the palm or a Internal rotation. The pain is described as punctual in the area of the narrowed shoulder area, but it can also pull in the upper arm towards the hand or over the shoulder towards the head. In addition to the pain, movement in the arm can also be restricted.
In the case of severe impingement syndrome, for example, raising the arm and turning it outwards is only possible to a limited extent or can no longer be carried out at all. In some cases, too sensitive disorders above the skin in the shoulder area described.
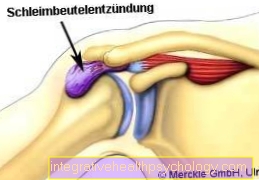
Impingement syndrome in combination with bursitis
Inflamed bursa often also contribute to the development of an impingement syndrome in the shoulder. Then one speaks of a bursitis. The bursae are located in the shoulder area to provide a kind of slide bearing for the tendons so that they do not rub against the bone and cause damage. The inflammation of the bursa in the subacromial space (Subacromial bursitis) is mostly based on degenerative wear and tear of the supraspinatus tendon due to the reasons mentioned above.
Read more on this topic at: Bursitis of the shoulder
The inflammation of the bursa leads to the fact that it no longer fulfills its actual task (protecting the tendon) and becomes sticky. The supraspinatus tendon is no longer protected by the bursa, but instead constricted and further damaged. If this inflammation persists, damage to the tendon can lead to a rupture.
The medium-term consequence of this process would be a so-called “frozen shoulder” - the shoulder becomes completely immobile due to the inflammation process. This must be prevented. When the arm is moved upwards or when the orthopedic surgeon tests for impingement, the typical tests are positive, as the inflammation and entrapment of the supraspinatus tendon has created a symptomatic constriction under the roof of the shoulder.
The therapeutic approach here is to eliminate the inflammatory process. This can be done conservatively with injecting steroids and using ibuprofen or voltaren. In addition, it is advisable to gradually increase physiotherapy in order to regain full mobility of the shoulder. If the therapy fails, surgical removal of the inflamed bursa and soft tissue is appropriate. If necessary, parts of the supraspinatus tendon have to be removed as well, as these are so damaged by the chronic irritation and inflammation that they are no longer strong enough. Then a reconstruction or a muscle transfer operation is indicated.

Figure shoulder joint
- Collarbone / clavicle
- Shoulder roof (acromion)
- Space between the head of the humerus and the roof of the shoulder
- Upper arm bone / (humerus)
- Shoulder joint (Articulatio glenohumerale
This disease is a wear-related (degenerative) change in the so-called supraspinatus tendon. This change occurs as a result of a tightness in the area of the arm rotating shoulder muscles called the rotator cuff and the muscles lying on top Bursa (= Subacromial bursaThe pain occurs as a result of the bruising between the humerus head and the overlying shoulder roof (acromion and acromio-clavicular ligament).
The distance between the humerus head and the shoulder roof is usually determined by means of an X-ray or a Magnetic resonance imaging.
In the context of the determination, the shoulder height is called the acromio-humeral distance, called the distance between the humerus head and the shoulder roof, which should ideally be greater than 10 mm. This 10 mm distance is considered to be the minimum dimension that squeezes the soft tissues in between, i.e. from Rotator cuff and subacromial bursa (Bursa the shoulder roof) should prevent. If this range is smaller, the probability of an impingement syndrome occurring increases.
The lateral lifting of the arm (= Abduction) is done by the train of Rotator cuff especially through the Supraspinatus muscle. As part of this movement, the humerus head slips under the shoulder roof, with the result that both the rotator cuff itself and the Bursa (Bursa subacromialis) slides under the roof of the shoulder. This process is considered normal physiological, so that there is usually enough space for these shifts. However, if there is not enough space for various reasons, the so-called occurs Impingement Syndrome, the subacromial tight syndrome on. The problem here is that due to the constant rubbing of the rotator cuff on the shoulder roof over the long term Rotator cuff damage can occur, which in the final state can also result in a complete crack of the same.
Depending on the cause and location of the impingement, a distinction is made between different forms in the shoulder area, which, however, require a more detailed knowledge of the shoulder anatomy.
diagnosis
Patients usually suffer from pain that is independent of movement, which - if it is also the Bursa have inflammation, can also occur at rest and at night. If you exert pressure on the anterior joint space in the area of the greater tuberosity and other examination points, so-called pressure pain occurs. Raising the arm against resistance is also painful when lifting in the range between 60 and 120 °. This is known as the so-called "painful arc" or "painful arc". There are also further function tests that target the Rotator cuff pinch under the shoulder roof.
The pain can be reduced by injecting a local anesthetic below the roof of the shoulder. In the event that the arm still cannot be raised despite freedom from pain or reduced pain, damage must be in the area of the Rotator cuff should be considered.
In order to be able to estimate the exact extent of the disease, one can use X-ray control assess the bony structure of the shoulder joint. The shape of the shoulder roof and the position of the humerus head or any calcifications of the Rotator cuffthat indicate wear in a special way are to be assessed.
There is also the option of an ultrasound examination or magnetic resonance imaging. It is possible to determine the condition of the rotator cuff and the size of the rotator cuff without side effects by means of an ultrasound examination Bursa to judge.
Investigations
During the physical examination, the examiner can sometimes cause pain by pressing the anterior joint space. When trying to raise the arm over the side against resistance, a pain event also occurs. If you imagine the range of motion of the lateral arm elevation (abduction) as a semicircle, the pain typically comes between 60-120°. This is where the Supraspinatus tendon in the said bottleneck and this phenomenon is called the "painful bow"(" Painful arc ").
In order to verify the diagnosis of the impingement syndrome, a so-called Switch-off attempt be performed. A local anesthetic is injected below shoulder level. If it is still not possible to raise the arm afterwards, there could be an injury to the Rotator cuff exist.
As an instrumental examination in suspected impingement syndrome, the Sonography, the roentgen and the Magnetic resonance imaging (Marne resonance imaging) consulted. In the ultrasound, the tendon can be searched for calcifications, the size of the bursa can be measured and the rotator cuff assessed. In the X-ray it is possible to examine the position and configuration of the bony structures and to measure the distance between acromion and humeral head (acromio-humeral distance), which is less than 10 mm speaks for the presence of an impingement syndrome. In addition, calcareous areas in the tendon can be seen in the X-ray. Magnetic resonance tomography provides information about the anatomy and pathologies of the shoulder joint, especially when the diagnosis is unclear.
Hawkins test
The impingement test after Hawkins is an orthopedic test that can indicate or disprove impingement syndrome. The test is mainly used when there is suspicion of an orthopedic disease in the shoulder joint or in the area of the upper arm.
The implementation of the Hawkins test takes place in which the patient either stands or sits in front of the examiner with the corresponding arm hanging relaxed next to the body.
The examiner grabs the with one hand Elbow of the patient, with the other he grasps that wrist of the patient.
First, the arm is im Shoulder joint bent 90 degrees, then the arm in the elbow joint. The patient then holds his arm straight in front of him.
The examiner then moves the patient's arm up and down, similar to a windshield wiper, and thus performs a passive rotation in the shoulder joint 130-145 Degree by. This combination of movements leads to an increasing constriction in the area of the shoulder joint. If this joint is already narrowed by an impingement syndrome, complaints are reported by the patient.
Above all, the pain indicated at the end of the pendulum movement leaves the Hawkins Test are positive and strongly suggest an impingement syndrome.
The Hawkins test denotes when the movement sequences described above do not result in movement pain. The falls Hawkins test negative, an impingement syndrome is as good as impossible.
In the rarest of cases, the test can be negative despite the presence of an impingement syndrome. In particular, lighter courses or very early stages often leave the Hawkins test negative, although there has been a pathological narrowing in the shoulder joint.
The Hawkins test is one of like in addition to the imaging tests Ultrasonic or X-ray examination to the most important measures in the diagnosis of a Impingement Syndrome.
The test can be carried out quickly, does not cost anything and gives a high diagnostic grade compared to the loads. Do patients have anatomically large spaces in the area of the Shoulder joint, the Hawkins test can also be negative if an impingement is in training.
Conversely, in this case a positive Hawkins sign indicates an already advanced impingement syndrome.
MRI of the shoulder joint
To possibly accompanying Injuries to the tendons of the Roator cuff or to assess the extent of the bursitis of the shoulder, the MRI of the shoulder joint has proven particularly useful.
However, the MRI of the shoulder is not a diagnostic tool that is always used in the early stages of an impingement.
You can also read more on this topic at: MRI scan of the shoulder joint
therapy
In the Impingement therapy - Syndrome one differentiates between a conservative and a non-conservative therapy.
As a rule, you start with a conservative treatment attempt, which mainly consists of:
- physical form of treatment and one
- drug treatment consists.
In the acute treatment phase, the arm should be spared and strained as little as possible. Strong lifting and carrying movements should initially be avoided and consistent physiotherapy should be started in parallel to the rest. The aim of this is to specifically train little used muscle groups in the shoulder area in order to relieve the shoulder joint as much as possible.
The training succeeds initially with so-called isometric building exercises. This is understood to mean muscle exercises that should be carried out statically with as little weight as possible and without self-loading. Most of the time, these muscle exercises are done passively. In the further course, active muscle exercises can also be added.
Medicinal treatment is also included in the conservative treatment of impingement syndrome.
The pain treatment and the anti-inflammatory effect of the medication are particularly important here. For this reason, drugs of the group are mostly used for drug treatment non-steroidal anti-inflammatory drugs (NSAIDs) used to which Ibuprofen or Diclofenac is counted.
The aim is to use the pain-relieving effect to get the patient out of the constant relieving posture caused by the pain.
Only then can further damage caused by a Impingement Syndrome can be triggered, avoided. Furthermore, conservative approaches include cooling and thus physical anti-inflammatory measures.
Bring in conservative therapy Impingement no improvement, it must be considered whether it makes sense one not conservative or operational Start therapy.
Exercises for the home
The aim of the exercises is the subacromial To enlarge space. It is important for that Muscles of the shoulder to train that the humerus head down (caudal) pull. Furthermore, the muscles of the Rotator cuff and also the muscles of the shoulder blade are trained.
An exercise to enlarge the subacromial There is room to lie the affected arm backwards on the back while standing (hand is above the buttocks) and then carefully pull this arm towards the buttocks with the other hand. This pull is then maintained for 20-30 seconds.
Another exercise is that oblique pushups. With your elbows almost extended, you push yourself shoulder-width apart in an inclined position on the edge of a table or chest of drawers. From this position, the arms are now slowly bent to almost 90 ° at the elbows. Then the arms are carefully stretched again. This exercise is done in 2-3 sets of 15-20 repetitions each.
Another exercise is straightening the trunk. You are sitting in a bent (slightly hunched) position. Then straighten up by pulling your shoulder blades back and lifting your head so that you are looking straight ahead. You almost take a tight military stance. This is an exercise that can also be done standing up and is definitely useful in between when working on the computer.
Two more home exercises will require one Theraband. You can get these for less than 20 euros in sports shops or orthopedic shops. The first exercise trains the external rotation in the shoulder. The arms lie against the body and are bent at 90 ° at the elbow. A Theraband is now held with both hands. The best way to do this is to put the Theraband around your hand like a loop. One elbow stays close to the body. With the other arm, slowly and steadily pull the Theraband outwards. It is important that the elbow also remains close and the movement is only a rotation in the upper arm - the palm of the hand rotates towards the back. This movement is done in 3 sets of approx. 20 repetitions. And that for every arm.
The other exercise needed one Theraband and some kind of fixing point on the ceiling (e.g. a stable hook or ring). The Theraband is placed over this fixation point so that you now have two equally long parts. You take this in your hands. You stand straight and stable. The elbows are bent at 90 ° and the upper arms are bent forward about 20 °. Now move both arms simultaneously and evenly backwards into extension. This movement is carried out in 3 rounds with approx. 20 repetitions. With all exercises, the rule is that they should not provoke any pain. In the event of pain or uncertainty about the exercises, a doctor should be contacted.
Operative therapy
Surgical therapies can be performed on the open shoulder joint or minimally invasive through arthroscopy.
In the second surgical procedure, a camera is advanced into the shoulder joint through a small incision. This camera delivers real images of the inside of the joint and shows the actual anatomical conditions.
In the case of open therapy, this is not necessary because the surgeon can take a look inside the joint himself. The aim of surgical therapy is on the one hand to remove inflamed tissue from the joint space and also to remove disturbing, bony protrusions from the joint space.
If the raven's bill contributes to the narrowing of the shoulder joint, it is notched both during open surgery and in minimally invasive arthroscopic surgery so that it is no longer in the way of the nearby muscles.
In older patients in particular, an impingement syndrome is only secondary to an anatomical narrowing. In most cases, an arthritic change in the shoulder joint is also to blame for impingement.
For this reason, as soon as severe osteoarthritis is seen in the shoulder joint, an attempt is made to remove parts of the collarbone.
One would like to achieve two different effects with this. On the one hand, this should create space in the already very narrow joint space; on the other hand, it should be avoided that the muscles involved in the shoulder movement increasingly rub against the bones and cause pain.
If parts of the clavicle are removed, there is inevitably a free space in the area of the clavicle and instability.
As a rule, however, this is not of long duration, since scarred tissue soon takes up the space between the collarbone and the shoulder joint. Consistent follow-up treatment through physiotherapeutic measures is essential, particularly after surgical, non-conservative therapeutic approaches.
Irregularly performed exercises can lead to a massive worsening of the prognosis and to chronic impingement syndrome.
In the surgical interventions, however, no relevant improvement can be achieved in around a third of those affected. In most patients with no major damage in the subacromial There is room, but conservative therapy works in the first few months. Therefore, in most of all cases it is worth trying to treat conservatively first. In around 80% of all patients, a relevant reduction in pain and symptoms can be achieved through conservative therapy alone. It is important that the patient really cooperates, spares himself and refrains from heavy work and movements that further promote impingement. If extreme defects in the tendons of the supraspinatus muscle or clear bony growths can be seen in the X-ray at the first presentation, then this can be a reason to resort directly to an operative measure.
Read more about this: Impingement syndrome surgery
If these measures are no longer effective, the next step is to start using medication. Here you can Painkiller from the group of non-steroidal anti-inflammatory drugs (NSAIDs) can be used, such as Ibuprofenthat counteract both pain and inflammation. Drugs that can be injected directly into the affected joint are more effective. This is often done cortisone used.Cortisone is a very effective anti-inflammatory, but it is quite strong and has many side effects, which is why it should not be used lightly and, if possible, only temporarily.
They also have an impingement syndrome physiotherapy and physical therapy very helpful. However, this should always be done under the guidance of a doctor or a trained physiotherapist so as not to cause even greater damage to the joint. Techniques that are helpful here are mainly special stretching exercises and Muscle building. The strength in the shoulder should be restored and movement restrictions are ideally minimized. In addition, certain mobilizations of the joint can also have a direct anti-inflammatory effect, as they stimulate the blood flow in the affected tissue and thus also the regeneration processes. However, it must be noted that these exercises can only have a positive effect if they are performed consistently, correctly and, above all, regularly over a longer period of time.
If conservative therapy does not lead to pain relief, surgical treatment can be considered. There are various options to choose from.
Surgery for impingement syndrome

First of all, you actually always try to get an impingement syndrome conservative, that is, to treat without surgery. If all the available possibilities of this form of therapy do not show the desired effect of freedom from pain or at least considerable relief, one must ultimately surgery can be used. There are several alternatives that must be weighed up depending on the severity of the disease and the individual condition of the patient.
It is the least invasive and costly arthroscopic intervention. Only very small incisions are necessary, through which the surgeon inserts a camera into the joint, with the help of which he can directly identify bony structures that lead to constrictions and, if necessary, remove them with a small device. In this variant, the intervention can normally outpatient takes place, i.e. the patient can leave the hospital on the day of the operation.
In the case of more pronounced clinical pictures, open therapy is usually preferable. Here larger bone spurs can be removed and any adhesions that may be present can be removed at the same time. If necessary, the surgeon can also remove parts of the joint and / or smooth joint surfaces. With this method, however, a larger cut of about 4 cm length take place, which is associated with a longer hospital stay.
The most drastic variant is the so-called subacromial decompression. The purpose of this operation is to expand the joint space in order to treat the existing impingement syndrome and to prevent a relapse. Depending on which structures of the joint were responsible for the symptoms, parts of the bones, tendons or parts of bursa can be removed during this procedure.
Following each type of surgery is a detailed one physiotherapy prescribed, whereby it is important to find a good balance between overloading the joint too early and immobilizing it for too long, both of which can negatively affect the healing process in the long term. The larger the operation, the slower the mobilization of the joint should be started and the longer it usually takes until the affected shoulder can regain completely normal mobility and freedom from pain.
Exercises after surgery
After the operation, not all movements should be performed with full force immediately. Since the subacromial Decompression not only removes bone and bursa, but often sutures or reconstructions of the supraspinatus tendon are also allowed not fully loaded become.
In the first 2 days After the operation, the arm must be in a so-called Gill Christ Association be worn. In the first week after the operation there should be no active movement of the arm. This means that the arm can only be moved by a physiotherapist. In addition, the surrounding muscles (neck, back, shoulder blade) should be trained because they are now increasingly needed to keep the upper arm in the ideal position.
Over the next few weeks, a plan is worked through together with the physiotherapist until the patient can put almost full weight on his shoulder again after approx. 4-5 weeks. But it also applies here that sports that allow violent shocks or strong forces to act on the shoulder should be avoided.
The exercises that are done with the physiotherapist after the operation correspond in principle to the exercises listed under Exercises for at home. It should be noted that some movements and exercises may not be done individually for each patient. This is included in the follow-up treatment plan by the surgeon and depends on the course of the operation and whether other muscles or tendons were affected.
Tap the shoulder
The Taping the shoulder in impingement syndrome is one frequently practiced technique. The aim is to relieve the muscles and improve the position of the humerus head. There are different methods that can be used. Depending on the method used, several tape strips of different lengths are required for taping.
In the first possibility an approx. 20 cm long tape (strongly depending on the size and muscle size of the patient) is stuck from the acromion (the shoulder height) diagonally over the shoulder blade to the spine. This happens under tension. A second tape is then attached to the deltoid along the shoulder blade.
A another possibility lies in the fact that a tape is affixed horizontally below the head of the humerus from the attachment of the pectoral muscle to the breastbone over the adjacent upper arm to the shoulder blade. A second tape is stuck diagonally from the chest over the shoulder to the side of the shoulder blade. The tapes are positioned so that there is an area between them in which the head of the humerus is located.
A third option uses a split tape. This is glued to the base of the deltoid muscle (lateral upper arm) with the upper arm lying flat. Then stick one part of the tape around the front of the deltoid muscle and the other part around the back so that the head of the humerus lies in between. Both parts are then put together in an adhesive point behind the shoulder roof (acromion). Another tape is then stuck from the upper side of the chest over this adhesive point to the shoulder blade. And a third tape is then stuck lengthways across the deltoid from the upper arm to the side of the neck.
The exact application of these methods should be done by an experienced person. Incorrect use will not achieve the desired effect and in the worst case may even worsen the problem.
forecast
Generally one has Impingement Syndrome a good prognosis compared to other orthopedic diagnoses.
However, this depends not only on the patient's age but also on the Severity impingement and the anatomical conditions.
Also decisive is the extent to which the patient adheres to rehabilitative measures.
If he does not carry out the necessary physiotherapeutic measures carefully, this worsens his prognosis immensely. As a rule, one can say that the conservative treatment approaches have a better prognosis than the surgical approaches.
But this is partly due to also because operative measures are only taken if the course of the impingement is severe, so the prognosis is already a little worse anyway.
Approx. 80% of the patients with a conservative therapeutic approach are symptom-relieved, even if not completely symptom-free. Between 60 and 75% of the patients who have to endure a surgical therapeutic approach are also symptom-free during the course.
However, this assumes that appropriate follow-up treatments are followed and that an adequate one Pain therapy is used.