Intubation anesthesia
What is intubation anesthesia?
Intubation anesthesia is general anesthesia in which the sleeping patient is ventilated through a ventilation hose (tube) that is inserted into the windpipe. Intubation is the gold standard of airway safety with the highest aspiration protection, i.e. the trachea is tightly closed by a balloon that is inflated around the tube to prevent the stomach contents from flowing back into the lungs.
Read more on the topic: Intubation

indication
The most important indication for intubation anesthesia is the increased risk of aspiration. Aspiration is the backflow of stomach contents via the esophagus into the windpipe. If a patient is anesthetized, all protective reflexes are switched off by the medication administered, i.e. stomach contents that get into the windpipe cannot be coughed up, but flow quietly into the lungs. This can cause significant damage and inflammation in the lungs. All non-fasting patients are at risk of aspiration, i.e. everyone who ate something 6 hours before the operation or had something to drink 2 hours before the operation. The same applies to all emergency patients, people with traumatic brain injuries and / or unconscious, as there are no protective reflexes here either.
In addition, all patients must be intubated with increased intra-abdominal pressure (pressure in the abdomen). This is the case with particularly fat (obese) and pregnant women. The pressure moves the stomach upwards and the risk of gastric contents reflux increases. The pressure in the abdomen is also increased in all operations in the abdomen, both laparoscopic and open operations are affected. During laparoscopic operations, the camera and surgical tool are inserted into the abdomen through small incisions in the skin. For a better view, the belly is filled with carbon dioxide and inflated, thus significantly increasing the pressure on the stomach.
Find out more about the topic: laparoscopy
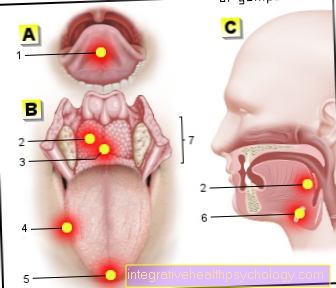
Other operations that require intubation are operations in the nose, throat, mouth, e.g. Throat tonsil removal or large facial skull injuries, as blood can run from there to the lungs. The blocked tube (inflated balloon around the tube) prevents this.
Long-term operations> 3-4 hours should also be better performed under anesthesia. Likewise operations in which the patient is placed on the prone or is operated on while sitting. Other indications are extensive burns, inhalation trauma, resuscitation, anaphylactic reactions and status epilepticus that cannot be broken.
Who Shouldn't Have Intubation Anesthesia?
Intubation also harbors some risks, such as damage to the vocal cords or other structures in the mouth and throat, which can lead to swallowing and speech disorders and even loss of voice. Accordingly, intubation should only be performed for the above-mentioned indications.
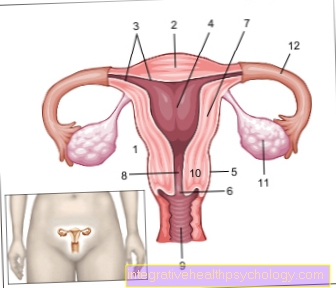
Brief operations on the extremities, the urogenital tract (except for laparoscopic interventions) or the skin can be performed under general anesthesia and using a laryngeal mask or possibly even under regional anesthesia.
Find out more about the topic: Laryngeal mask
The course of intubation anesthesia
The patient is supine with the head slightly elevated on a small pillow. A venous access is established in advance to administer the necessary medication. First a strong pain reliever (e.g. sufentanil or fentanyl) is administered. Next, the anesthetic (usually Propofol) is injected. If the patient sleeps and stops breathing, a mask that is placed firmly on the face is first used for ventilation.
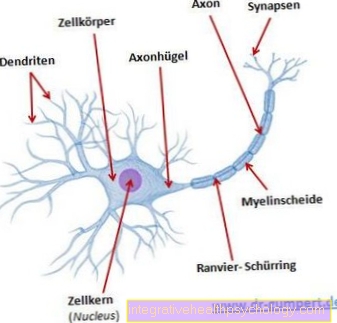
Then a muscle relaxant is injected (e.g. cis-atracurium or succinylcholine), which slackens all of the muscles in the body and especially the muscles of the larynx. The glottis opens and the tube (breathing tube) can be inserted into the windpipe with the help of a spatula (laryngoscope). The balloon is inflated (= blocked) around the tube via a small tube, thus closing the windpipe.
Air can now only be administered through the lumen of the tube. The ventilation hose is connected to the ventilation machine via a hose system, which takes over the breathing for the sleeping patient.
This article might also interest you: anesthesia
Induction of anesthesia
Initiation is understood to mean the transfer of the waking patient to the deeply sleeping patient. Pain, consciousness and muscle strength are switched off. Three drug groups are required for this - strong pain relievers (e.g. sufentanil), narcotic (propofol) and muscle relaxants (e.g. cis-atracurium).
Initiation also includes the process of intubation and setting the ventilator. At the end of the induction, the patient is positioned for the operation, making sure that the parts of the body are in an axially aligned, gentle position in order to avoid positional damage.
Read more on the topic: Induction of anesthesia - the right preparation
Maintenance of the general anesthesia
Anesthetic must be administered continuously to maintain intubation anesthesia. Two different principles are available here. You can continue to inject intravenous drugs via a perfusor (e.g. propofol, thiopental, etomidate, barbiturates) or you can switch to inhaled narcotics such as e.g. Desflurane or sevoflurane.
In addition, painkillers have to be injected after longer or particularly painful operations; different groups of active ingredients are available here (opiates, non-steroidal anti-inflammatory drugs). As part of general anesthesia, blood pressure or heart rate fluctuations can occur, countermeasures may have to be taken with medication. In addition, fluids are always administered through infusions.
Find out more about the topic: Narcotics
Anesthesia diversion
The end of the anesthesia and the waking up of the patient are called diversion. Towards the end of the operation, the supply of the anesthetic is stopped; depending on the anesthetic, it takes 5-15 minutes until the patient regains consciousness, breathes independently, opens his eyes and reacts to speech. It is essential to ensure that the muscle relaxant has been completely broken down by the body, otherwise the patient will not be able to breathe independently.
If the patient is able to take deep breaths independently, the ventilation tube can be removed. The stomach should be sucked off beforehand, because stomach contents can also be swallowed when you wake up. After recovery, the patient is taken to the recovery room and monitored for at least one hour.
Read more on the topic: Anesthesia diversion - procedure, duration and risks
These risks exist
With any general anesthetic, there are some risks, such as allergic reactions to medication administered to anaphylactic shock. Circulatory disorders in the form of too low or too high blood pressure or heart rate. In addition, ventilation problems can arise, especially patients with lung diseases (asthma, COPD) and smokers are particularly at risk of bronchospasm (narrowing / cramping of the airways).
Special risks of intubation are tooth damage that can be caused by the rigid spatula, soft tissue injuries in the mouth and throat area with bleeding and swelling. Inserting the tube through the glottis into the windpipe can irritate or damage the vocal cords. After intubation, many patients complain of a slight sore throat and hoarseness, but these go away on their own after a few hours.
In rare, severe cases, serious speech disorders up to and including loss of voice can occur. As already described above, the loss of protective reflexes can lead to stomach contents being swallowed into the lungs (aspiration). Lung tissue is destroyed by the acidic gastric juice and inflammation is triggered. It can lead to severe pneumonia that requires intensive medical treatment.
The muscle tone of the body is reduced during anesthesia, so care must be taken to position all parts of the body carefully in order to prevent nerve damage (positioning damage). A very rare complication during anesthesia is malignant hyperthermia triggered by anesthetic gas. The body temperature rises quickly and uncontrollably, which can lead to death.
Further information on the topic can be found at: Risks of anesthesia
After-effects of general anesthesia
Immediately after intubation anesthesia, you are still tired for some time, and patients can sleep in in the recovery room. Many patients are also a little confused, the medication administered can cause a brief retrograde amnesia, so patients often ask the same questions until they are clear in their head again. In elderly patients, this condition may last a little longer and be more pronounced (delirium, passage syndrome).
Read more on the topic: Retrograde amnesia and continuity syndrome
In addition, some people are a little less inhibited by the medication, talk a lot and openly, or are tearful. A common after-effect of anesthesia, especially in women, is nausea and vomiting - this is known as postoperative nausea and vometing (PONV). If this is known before the anesthesia, drugs are given towards the end of the anesthesia to prevent nausea. As already mentioned under Risks, hoarseness and difficulty swallowing can occur after intubation. In the waking up phase, so-called shivering (involuntary tremors) can also occur.
Also read the article on the topic: Aftermath of anesthesia
Complications after intubation anesthesia
One possible complication after intubation anesthesia is respiratory depression due to opiate overhang. If too much of the strong pain reliever is administered during the anesthesia, breathing may stop even after the anesthesia or those affected may breathe slowly and deeply. So-called command breathing occurs - the patient must be reminded to breathe again and again. Therefore, all patients are monitored in the recovery room after general anesthesia. In the worst case, the patient has to be re-intubated and ventilated.
Nausea and reduced protective reflexes can lead to stomach contents being swallowed even after the operation. Patients are therefore always placed in a high position after anesthesia. The medication administered or circulatory fluctuations during anesthesia can lead to confusion, especially in older patients, with sometimes aggressive behavior (delirium, passage syndrome) after anesthesia.
Also read the article on the topic: Side effects of general anesthesia
These drugs are used
Intubation anesthesia has three functions, namely the elimination of pain, consciousness and muscle strength. A strong pain reliever is administered first - strong opiates are always used here, such as Sufentanil (1000 times stronger than morphine) or Fentanyl (100 times stronger than morphine).
Next, a narcotic ("sleeping pill") is injected. The most common is propofol, a white liquid that will make you fall asleep in a few seconds. Other options are thiopental, etomidate, or benzodiazepines. To maintain the anesthesia, inhalative anesthetic gases such as sevoflurane or desflurane can be used or you can continue working with propofol.
Further information on the subject can be found at: Narcotics
Muscle relaxants such as cisatracurium, mivacurium, rocuronium or succinylcholine are used to switch off muscle strength. Depending on how quickly the effect should be felt or how long the procedure is planned, different drugs must be used.
Read more on the topic: Muscle relaxants
Is an anesthetic possible despite a cough / runny nose?
If the patient is actually healthy, has no pre-existing cardiovascular or lung disease and only has a slight cough / runny nose without a fever, an anesthetic can still be considered. However, it is possible that symptoms worsen after anesthesia. The intervention puts additional strain on the immune system and cannot defend itself so well against pathogens.
However, if there is a strong cough or cough with sputum, as well as runny nose with yellowish secretion or fever, the operation should be postponed if possible. Intubation anesthesia puts a lot of strain on the body and a strong immune system is also important for healing after the operation.
You might also be interested in this topic: General anesthesia for a cold
Recommendations from the editorial team
- Intubation
- Laughing gas
- Types of anesthesia
- Sedation
- general anesthetic