Liver cancer
Synonyms
- primary hepatocellular carcinoma
- hepatocellular carcinoma
- HCC
- Hepatoma
Note
All information given here is only of a general nature, tumor therapy always belongs in the hands of an experienced oncologist (tumor specialist)!
definition
Under a Liver cancer (Hepatocellular carcinoma) one understands a malignant degeneration and uncontrolled growth of the cells of the liver tissue.
Causes and forms

The most common cause of liver cancer (hepatocellular carcinoma) is cirrhosis of the liver. Patients who suffer from cirrhosis of the liver (a spongy, spongy structure of the liver with a loss of function) either from hepatitis or from excessive alcohol consumption have a greatly increased risk of developing liver cell carcinoma (liver cancer) in the further course.
80% of all liver cell carcinomas (liver cancer) are diagnosed as a result of liver cirrhosis. 4% of all liver cirrhosis patients develop liver cell carcinoma. 50% of patients with hepatocellular carcinoma (liver cancer) previously had hepatitis B, 25% had hepatitis C.
The metabolic disorder hemochromatosis and patients with an early childhood infection with HB viruses have an increased risk of liver cell carcinoma. The regular intake of androgens (male sex hormones) e.g. bodybuilders have also shown an increased risk of liver cell carcinoma.
The connection between diabetes mellitus and an increased risk of developing liver cancer (hepatocellular carcinoma) also seems to be confirmed today. The latest studies have also discovered a molecular mechanism that is believed to be responsible for the development of liver cell carcinoma (liver cancer). It has been shown that in 60% of cancer patients, a so-called tumor suppressor gene (FHIT) is disturbed.
This is a mechanism at the genetic level that is supposed to suppress tumor cell growth and the disruption of which leads to uncontrolled cell division via protein formation.
You may also be interested in this topic: End-stage liver cancer
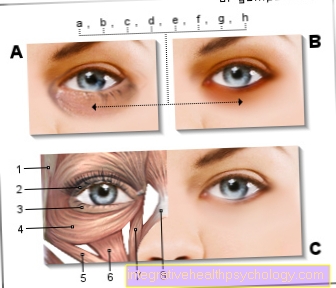
Illustration liver

- Right lobe of the liver -
Lobus hepatis dexter - Gallbladder duct -
Cystic duct - Gallbladder -
Vesica biliaris - Main bile duct -
Common bile duct - Portal vein -
Vena portae hepatis - Hepatic artery -
Hepatic artery propria - Round liver band -
Ligamentum teres hepatis - Common
Liver bile duct -
Common hepatic duct - Sickle ligament of the liver
Falciform ligament - Left lobe of the liver -
Lobus hepatis sinister - Hepatic veins -
Hepatic veins - Lower vena cava -
Inferior vena cava - Diaphragm - Diaphragm
You can find an overview of all Dr-Gumpert images at: medical illustrations
Dem Aspergillus flavus mushroomwho i.a. grows on grain in humid climates, is also thought to have a carcinoma-promoting effect.
The subdivision of the hepatocellular carcinoma (Liver cancer forms) occurs through the different types of growth according to solitary (single), multicentric (in several places), diffuse infiltrating (distributed everywhere and growing into), according to the histology and the tissue structure as well as the so-called TNM classification.
If the liver tumor has not yet broken through a blood vessel, it would be classified according to T1. It is important that this is only one tumor.
If there are several, but not larger than 5 cm, or if there is already an intrusion into the blood vessel system, this stage would be referred to as T2. Multiple tumors larger than 5 cm or one in size Invasion of the hepatic vein (V. portae) were given the designation T3.
T4 is used to name all the tumors that already have neighboring organs or the peritoneum (peritoneum, Peritoneal cancer) have infiltrated. Are there already lymph node metastases in or around the liver to find, this stage would also be classified with N1 (N = nodes), and if distant metastases were to be found in the body, with M1. In summary, these findings are again divided into stages.
That's how you understand under stage I.: T1N0M0 under stage II: T2N0M0 under stage III: T3-4N0M1 and under stage IV: all findings with M1.
There is also a so-called CLIP Score, in which points from 0-2 in the Categories Child Pugh (Statement on liver restriction), tumor morphology, proof of Tumor marker alpha-fetoprotein and presence of one Hepatic vein thrombosis be awarded.
diagnosis
As with any illness, it is very important to ask about the medical history (anamnesis), in which the type, time and duration of the symptoms must not be missing. In many cases there is yellowing of the patient's skin and eyes, which should make the doctor think of a liver disease upon eye contact. The doctor should also ask whether the patient is already known to have cirrhosis of the liver or a hepatitis infection, or whether the patient has an alcohol problem.
In addition to the general physical examination, the doctor should also feel (palpate) the area above the liver to find out whether one can either feel an enlarged liver or even the actual tumor. Sometimes it happens that listening (auscultation) with the stethoscope reveals a pathological flow noise, which is caused by compression of the corresponding blood vessels or high blood pressure in the hepatic vasculature caused by liver cirrhosis and / or liver carcinoma.
Another important examination option is ultrasound, with which the doctor can already recognize a tumorous change in many cases. A statement can also be made here as to whether a finding is a primary carcinoma or daughter tumors (metastases) from other organs. A so-called color Doppler examination as part of the ultrasound makes the flow of the blood clear and indicates whether there has been an overpressure in the liver system and whether any changes found in the liver are already supplied with blood or have broken through the blood vessel system (see staging).
Computed tomography (CT) can also be used afterwards. An X-ray of the chest or a scintigraphy of the skeleton should be performed later to rule out a primary tumor elsewhere in the body. Smaller tumor foci (1-2 cm) can best be detected with magnetic resonance imaging of the vessels (MR angio). A general MRI of the liver can also be useful.
A blood test may be able to detect proteins that are formed by the tumor (tumor markers). The so-called alpha-fetoprotein is specifically increased in patients with liver cell carcinoma (liver cancer). The search for tumor markers, however, is less the possibility of a primary diagnosis than an option of follow-up, in which a sudden further increase can mean a recurrence of the tumor or a transition from cirrhosis of the liver to liver cell carcinoma.
At the time of diagnosis of hepatocellular carcinoma (liver cancer), 50% of the cases have multiple tumors in the liver (multilocular growth), 25% thrombosis of the portal vein and 10% of the cases infiltration of the hepatic veins and the inferior vena cava. After the diagnosis of hepatocellular carcinoma it must always be assumed that the tumor has already spread daughter tumors in other organs.
Liver cell carcinoma is feared for its rapid metastasis in the brain, lungs and bones. The doctor should also order what is known as “tumor staging” as soon as possible, in which he examines the metastatic organs most frequently affected by liver cell carcinoma using appropriate imaging (X-ray, CT, scintigraphy).
Find out all about the topic here: The therapy of liver cancer.
frequency
90% of all hepatocellular carcinomas (liver cancer) are actually liver metastases that were spread over the course of another malignant tumor located in the body. The liver is therefore the most frequently affected organ of metastasis after the lymphatic system. In Germany, around 5-6 people per 100,000 inhabitants develop hepatocellular carcinoma every year. The cause is very different here (see above).
In tropical countries (Africa, Asia), hepatocellular carcinoma reaches a frequency of 30 people per 100,000 inhabitants per year and is the most common malignant disease in men. In Germany, too, men are affected somewhat more frequently than women (ratio 3: 1 ). Worldwide it is assumed that there are up to a million new cases per year. In Germany, the disease mostly occurs between the ages of 50 and 60. In tropical countries, patients often fall ill between the ages of 30 and 40.















.jpg)