Kidney transplant
Synonyms
Kidney Tx, NTX, NTPL
engl. = kidney transplantation, renal transplantation
Definition kidney transplant

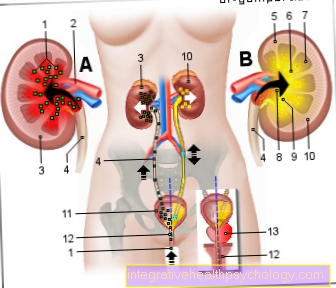
Under one Kidney transplant one understands the operative implantation of a donor organ in a recipient. A kidney transplant is required in the presence of end-stage renal dysfunction (terminal Renal failure).
A distinction is made between living donations and corpse donations, with relatives or people close to them being one of them in the first case Kidneys donate, in the latter case the organ comes from a dead person. The fact that the foreign kidney does not contain the same genetic material as its own means that a patient who has had a transplant usually has to take medication for life that contains the immune system consciously weaken to Rejection reactions to prevent. However, the chances of success have increased significantly in recent years.
In addition to the kidney transplant, blood washing (dialysis) at Kidney failure used. Blood washing removes harmful substances from the patient's blood, as the kidneys can no longer take on this task. Here, however, the patient has to have his kidneys cleaned by a machine several times a week. In general, a surgical procedure, i.e. a kidney transplant, is associated with a high gain in quality of life for the patient, as his / her everyday functions are more unrestricted and can participate far more in social life than with a patient who requires dialysis.
Epidemiology
In 2008 in Germany 1184 kidneys (Corpse organs) donated for a kidney transplant. From living donations, 609 organs were transplanted in the same year. On average, this is around 2000 kidneys transplanted each year. In the US, however, there are around 25,000 per year. The kidney transplant is dependent on the individual body characteristics and the activity of the immune system.
In the case of kidney transplants, 80% of the cases are a corpse donation, while 20% are living donations.
A total of 7703 patients from Germany were on the waiting list for a donor kidney in 2008.
history
The first Kidney transplant was in years 1902 made by Emerich Ullmann on a dog. The first human kidney transplant took place 1947 in Boston by David H. Hume, but was unsuccessful due to a rejection reaction to the donated kidney. Six years later 1953, Jean Hamburger was able to perform the world's first successful kidney transplant in Paris on a young boy. The child survived for several days with a poorly functioning kidney.
Less than a year later, Joseph Murray performed a successful twin transplant in Boston. These survived eight years. 1962 he carried out a kidney transplant with subsequent treatment Immunosuppressants so that he successfully transplanted a kidney between two non-blood relatives. Rheinhald Nagel and Wilhelm Brosig led 1964 carried out the first successful kidney transplant in Germany. Günther Kirste made the breakthrough 2004 in Freiburg, where he and his team performed a live transplant on a patient with incompatible blood types.
diagnosis
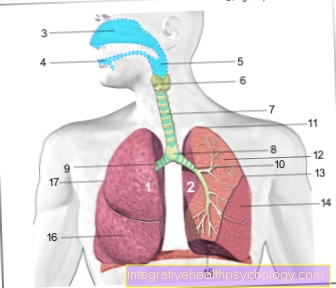
To confirm the diagnosis of kidney failure or kidney failure, the Filtration rate the kidney determines Ultrasonic and imaging techniques like a CT and MRI used, as well as various Laboratory parameters (Creatinine, Cystaine C, 24-hour urine collection). In individual cases, a piece of tissue is surgically removed from the kidney and examined in the laboratory (biopsy). An important prerequisite for a kidney transplant is the match of the blood group of the donor and the recipient. Contraindications are patients with severe Tumor disease with poor chances of recovery, acute infections and severe ones Heart disease.
Indication / requirement

A kidney is transplanted in patients who have terminal renal failure (irreversible renal dysfunction) are ill. This can also be due to the fact that more than a third of one's own kidney tissue (on both sides) is already inoperable and the patient therefore remains for the rest of his life requires dialysis is.
The body is no longer able to carry out the vital detoxification function, which after a short time leads to multi-organ failure and thus to death. Kidney failure can be triggered, for example, by the regular intake of Pain medication over a longer period of time, diseases of the kidney corpuscles due to a dragged on cold, Cysts in kidney tissuethat affect kidney function, Inflammation of the renal pelviswhich occur frequently in patients and cannot heal properly, Water sac kidney with urinary obstruction as well as through diabetes and high blood pressure. Because the kidney is no longer working properly, it can no longer concentrate the urine sufficiently to remove the pollutants from the body.
This sets the guidelines for such an organ transfer in the context of a kidney transplant Transplant Act firmly. The prerequisite for receiving a donor kidney is that the blood group is compatible ABO systems. This means that the Blood types of donor and recipient match so that the recipient does not develop antibodies against the donor's blood group. If antibodies were formed, there would be one Rejection reaction the kidneys received that Organ transplant would have failed.
Contraindication
A Kidney transplant cannot be done in patients suffering from an already disseminated malignant tumor (metastatic malignancy) Suffer. Also in the presence of an active systemic infection or in HIV (AIDS) is not transplanted.
If the patient's life expectancy is less than two years, this also rules out a kidney transplant.
Particular consideration must be given to organ transfer in an advanced one arteriosclerosis (Hardening of the arteries) or if the patient does not cooperate (Compliance).
Complications
If the kidney transplant goes well, the kidney will pass urine immediately. If this is not the case, there is probably slight damage to the kidney tissue. This damage can be due to transport (transport from the donor to the recipient) or often also with donations from the deceased, since the kidneys are very sensitive outside of an organism. After the operation, the body must be given a blood-thinning agent (usually Heparin), otherwise there is a risk of a Blood clots forms on the surgical suture.
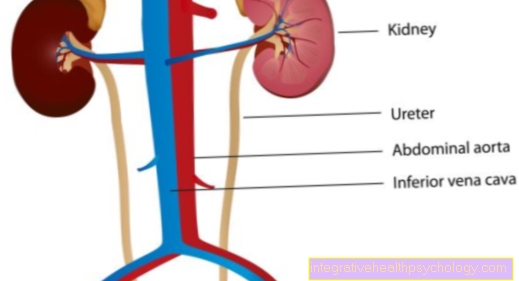
A blood clot is a clot of clotted blood that can loosen and block a kidney vessel, for example. This has life-threatening consequences. Despite the blood thinning, there is a residual risk that such a clot can form. In rare cases, the ureter (Connection between the kidneys and the urethra) in the execution on the kidneys, leak, which can only be fixed surgically.
If the operation goes according to plan, the kidneys can already produce and drain urine during the operation. If this is not the case even after a delay, it must be assumed that the kidney is in a damaged state. This can happen, for example, during transport from the donor body to the recipient body, since the kidney is not supplied with oxygen during this time.
The most common complications after kidney transplantation can be divided into four groups:
- postoperative complications
- Rejection reaction
- Consequences of immunosuppression therapy
- Recurrence of the underlying disease (Recurrence)
1. To the postoperative complications include bleeding, blood clot formation in the kidney vessels (thrombosis), acute kidney failure of the transplanted organ (acute loss of function) or leaks in the ureter (Ureteral leakage).
2. Acute rejection reaction after a kidney transplant means that the recipient organism recognizes the donated organ as foreign and rejects it as a defense mechanism. As a result, the new kidney cannot function.
To avert acute rejection reactions, so-called corticoid pulse therapy (high-dose administration of Cortisone in a short time without a subsequent slow dose reduction) or the immunosuppressive treatment intensified. If there is no response to Steroids (Steroid resistance) other drugs are administered (ATG, OTK3).
3. The complications that can occur after kidney transplantation also include the effects of the Immunosuppressive therapy. These include, on the one hand, an increased susceptibility to infections and, on the other hand, an increased development rate of malignant cancerous tumors (Malignancies).
The transplant patient often becomes infected with Pneumocystis jiroveci (lung infection), Viruses of the Herpes group (CMV = C.ytomequal-Virus, HSV = Herpes Simplex Virus, EBV = Epstein-Barr Virus, VZV = Varicella zoster virus; various clinical pictures) or Polyoma BK virus (Nephropathy).
The increasing number of malignancies in kidney transplant recipients are above all Skin tumors or B-cell lymphomas caused by EBV, tumors of the Lymph nodes caused by that Epstein-Barr Virus.
4. Another complication that can occur after a kidney transplant is the Recurrence of the underlying disease This is understood to mean the recurrence of the disease originally affecting one's own kidneys in the new transplanted organ.
Finally, severely elevated blood pressure is often observed in kidney transplant patients, which requires lifelong treatment.
forecast
The prognosis after a kidney transplant is considered to be good. Over 90% of the transplanted kidneys usually function properly for about 5 years. Even beyond this period, good patient experiences have been reported. However, there are differences in the duration of functionality, whether one receives a living donation or a deceased donation. About 70% of the kidneys of deceased people are functional for about 5 years. If the new kidneys fail, the patient has to do blood washing (dialysis) or seek another kidney transplant, which is very rare. A kidney transplant increases the gain in quality of life and autonomy enormously. Patients usually benefit greatly from a kidney transplant.
prophylaxis

To prevent kidney transplantation, or kidney damage in general, you need to take extra care of your kidneys. Traumatic events caused by hypothermia or vibrations (for example when riding a motorcycle), but also diet and health behavior play a major role in prophylaxis and prevention.
If possible, the kidneys should not be cooled externally and should not be exposed to supercooling or continuous vibrations. You can protect yourself against this with a simple kidney belt when riding a scooter or motorcycle (even in warm seasons). In addition to diet, individual health behavior also plays a major role. CystitisKidney pelvic complaints in the form of back pain, discolored urine (brown, red, very dark) are often assessed too late by a patient as worthy of treatment, so that, among other things, an infection of the urinary tract can be carried on and consequential damage remains in the form of an incompletely functional kidney.
Eating healthily is also good for the kidneys. A protein-reduced (not low-protein) diet is also advisable for patients with no kidney damage. Salt should also only be consumed slightly, as it increases blood pressure, which in the long term is not good for kidney function. The daily intake of 1.5-2 liters of water is recommended. Less and significantly too much water damage the kidneys through increased kidney activity, but the heart is also affected due to a continuous increase in blood volume. Obesity should also be avoided, as this stresses the kidneys directly through the weight and indirectly through an increased intake of salt (through more food; eating ready meals that have a high salt content, etc.), as well as an increase in blood pressure and the Blood sugar levels.
High blood sugar levels increase the risk Diabetes mellitus (Diabetes) to get sick. A low-potassium diet is only required if kidney failure is diagnosed. Fresh fruits and vegetables as well as adequate exercise contribute to healthy kidney function. According to recent research, one suspects a connection between Vitamin D deficiency and electrolyte deficiency in kidney damage. Vitamin D can be produced by the body in the form of sun rays and electrolytes are absorbed with a balanced diet. Regular check-ups by your family doctor are also a well-proven means of early detection of possible diseases and prophylaxis.
Summary
The term kidney transplant describes the transfer of a foreign kidney from a donor to a recipient. In order to receive such an organ, the recipient must either be put on a list for the allocation of a cadaveric organ (responsible organization = Eurotransplant), or find a close person for a living donation.
In order to be allocated a donor organ, the patient must first meet various health requirements and is then allocated an organ based on certain criteria such as blood group compatibility (matching of the blood groups of the donor and recipient).
The actual organ transfer takes place in one operation. Thereafter, the transplanted patient receives drug therapy to suppress his Immune system (Immunosuppression therapy), which must be carried out for life. The goal of this treatment is to prevent organ rejection, one of the most important complications that can occur after a kidney transplant.
The prognosis for the functionality of the new kidney depends on the one hand on the origin of the donated organ (better prognosis for living donations) and on the other hand on the optimal setting of certain values such as blood pressure or blood lipids.