Rheumatoid arthritis
Synonyms in a broader sense
- Rheumatoid Arthritis (R.A./ RA)
- chronic polyarthritis (c.P. / cP)
- Rheumatic disease
- primary rheumatoid arthritis (pcP / p.c.P.)
English: Rheumatoid arthritis, rheumatism
definition
The most common inflammatory joint disease belonging to the rheumatic group is the so-called (seropositive) Rheumatoid arthritis or rheumatoid arthritis.
It is a systemic, i.e. Inflammatory disease affecting the entire body, usually progressive, which affects the organs (joints, tendon sheaths, Bursa) infects.

In the course of the disease, Joints and tendons, which leads to deviations in shape and axis as well as restricted movement.
The course of the disease from rheumatism is very different, in rare cases organs outside the musculoskeletal system are also affected (Eye, skin, Vessels, lung, heart, kidney or gastrointestinal tract).
Approx. 1% of the population, with no significant geographic or racial differences, suffer from rheumatoid arthritis.
Women are three times more likely to be affected than men.
Men usually get sick between the ages of 45 and 65, women between the ages of 25 and 35 or after the age of 50.

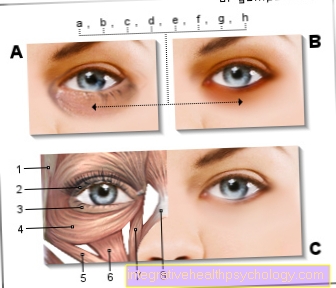
Illustration rheumatism of the hand
Typical x-ray of a hand suffering from advanced rheumatoid arthritis.
The medically termed “ulnar deviation” of the hand is typical. This means that the fingers deviate in the direction of the little finger as part of the disease.
With modern drugs one sees these pronounced rheumatic changes less and less.
root cause
The cause of the R.A. (= rheumatoid arthritis) is largely unknown. An isolated familial accumulation of the disease makes a genetic component likely. Several genetic factors are assumed that control certain immune reactions and, under certain conditions, become independent and thus those for the rheumatoid arthritis / primary rheumatoid arthritis trigger characteristic inflammation. Various pathogens (e.g. Epstein-Barr Virus) or a common pathogen substance (e.g. a glycoprotein) is suspected.
Symptoms
The misdirected immune reaction leads to inflammation of the synovial membrane lining all the joints (= synovitis). This thickens and forms more synovial fluid (joint effusion). A painful swelling of the joints develops. As a result, the joint capsules and the ligaments of the joints are overstretched and the joints can become unstable. The inflamed and overgrown synovial membrane gradually encroaches on the articular cartilage. Together with released enzymes (aggressive joint proteins), the joint cartilage is destroyed over time. In the advanced stage, the inflamed tissue undermines the bone from the joint edges and ultimately leads to the destruction or deformation of the entire joint.
Also read on this topic: Inflammation of the synovial membrane
Rheumatoid arthritis (RA) usually begins gradually.
Typical symptoms are:
- Pain on pressure or movement,
- Swelling and
- Overheating of joints.
Usually there is morning stiffness for up to three hours, i.e. Loss of function of the affected joints and subsequent “thawing” with a significant increase in function. Finger, hand, elbow, shoulder, knee, ankle and toe joints are most frequently affected, mostly symmetrically. However, rheumatoid arthritis (cP) can affect virtually any joint, including the spine.
Sometimes general symptoms such as fever, rapid exhaustion, loss of appetite and weakness also appear.
In addition to the joints, the tendon sheaths can also be affected by rheumatoid arthritis. This tendovaginitis usually occurs in the hand area and can lead to tendon rupture.
Furthermore, so-called rheumatic nodules occur in around 30% of patients. These are small nodules that form in the area of protruding bones, tendons or ligaments and the size of which often depends on the inflammatory activity of the disease.
Read more on the subject at: Tendonitis in rheumatism, swollen ankles
diagnosis
The Diagnosis rheumatoid arthritis results from:
- Symptoms
- physical examination
- Laboratory values and x-ray.
The American College of Rheumatology (ACR) established criteria for the diagnosis of rheumatoid arthritis (R.A.) in 1987. From one chronic polyarthritis (cP) can be assumed if a patient fulfills at least four of the seven criteria, whereby criteria 1-4 must have passed for at least six weeks.
ACR criteria for the diagnosis of rheumatoid arthritis:
- Morning stiffness of at least an hour
- At least three joint areas must show soft tissue swelling or joint effusion at the same time
- At least one joint swelling affects a hand, metacarpal or medial joint
- Symmetrical simultaneous involvement of the same joint regions on both sides of the body
- Rheumatism - lumps over protruding bones or near joints
- So-called. Rheumatism factor (RF) detectable in the blood
- Radiographic changes typical of rheumatoid arthritis (RA) on an X-ray of the hand
ACR-EULAR classification criteria for rheumatoid arthritis
In 2010, on the joint initiative of ACR (American College of Rheumatology) and EULAR (European League against rheumatism), new criteria were created, which offer the possibility of a very early diagnosis as the main advantage.
In contrast to the old criteria from 1987, the new criteria dispense with the characteristics morning stiffness, symmetry of the joint involvement and rheumatic nodules. The presence of erosions in the X-ray image is considered a reliable diagnosis from the outset. Joint involvement not only includes joint swelling, but also tenderness in the joints.
ACR-EULAR classification criteria for the R.A .:
Joint involvement
- 1 medium / large joint: 0 points
- > 1 medium / large joint, not symmetrical: 1 point
- > 1 medium / large joint, symmetrical: 1 point
- 1-3 small joints: 2 points
- 4-10 small joints: 3 points
- > 10 joints, including small joints: 5 points
Serology (RF + ACPA)
- neither RF nor ACPA positive: 0 points
- At least 1 test weakly positive: 2 points
- At least 1 test strongly positive: 3 points
Duration of synovitis
- <6 weeks: 0 points
- > 6 weeks: 1 point
Acute phase proteins (CRP / BSG)
- Neither CRP value still increased BSG: 0 points
- CRP or ESR increased: 1 point
If 6 points are reached, a R.A. in front. Requirements: confirmed synovitis in at least one joint, exclusion of other diagnoses that could explain the synovitis, no typical erosions on the X-ray (then the R.A. is considered confirmed).
Laboratory values

Laboratory diagnostics are used to make a diagnosis, but also to assess the course / activity of the disease, the response to therapy and it has a prognostic value. The laboratory values must always be assessed in conjunction with other findings.
Rheumatoid factor (RF) or antibodies against citrullinated cyclic peptides (CCP antibodies or ACPA: anti-citrullinated protein antibodies) are available for diagnosis.
The rheumatoid factor is detected in the blood. It develops in the first few years of the disease. It is an immunoglobulin that is formed in the synovial membrane of the diseased joints. Rheumatoid factor becomes positive in 75-80% of patients with rheumatoid arthritis / primary rheumatoid arthritis as the disease progresses. However, it can sometimes also be detected in other diseases and in old age.
CCP antibodies / ACPA are better suited for early diagnosis, as they can be detected in the very early stages of the disease. The combination with a positive rheumatoid factor increases the likelihood of rheumatoid arthritis to almost 100%.
The so-called rheumatoid factor (RF) is probably one of the best-known autoantibodies. Find out more about many other autoantibodies and their clinical pictures under the following article: Autoantibodies
The ACPA seem to be of considerable importance for prognosis. If the ACPA titre is high, the risk of severe disease progression increases.
Other typical laboratory findings in the blood of patients with primary rheumatoid arthritis are increased inflammation levels, e.g. CRP (C - reactive protein), and an accelerated erythrocyte sedimentation rate (ESR). The iron value as well as hemoglobin (Hb) and leukocytes (= white blood cells) are often low, the copper value, gamma globulins and thrombocytes (= blood platelets) can be increased.
Laboratory diagnostics also serve to rule out other diseases.
roentgen
The affected joints should be x-rayed annually to establish a diagnosis and, particularly in the first few years, to monitor the progress.
The radiological changes on the X-ray image are narrowing of the joint space, decalcification near the joint (osteoporosis), erosion of the joint surfaces, later destruction of the joint surfaces as well as stiffening / osseous development of the joints or joint dislocations / joint misalignments.
There is a radiological staging on the X-ray according to the severity of the joint changes in 5 stages (classification according to Larsen).
Other diagnostic examinations that can be carried out for specific questions are:
Sonography (ultrasound) of the joints or tendons, e.g. to show a joint effusion on the hip joint, to show a Baker's cyst (popliteal cyst) in the hollow of the knee or to show tendon tears in the shoulder area (tear of the rotator cuff) or the Achilles tendon (Achilles tendon tear).
Further information can be found under our other topics:
- Sonography
- Baker's cyst
- Rotator cuff tear
- Torn Achilles tendon
Computed tomography or magnetic resonance tomography, e.g. if the spine is affected.
Synovial analysis and tissue (histological) findings: laboratory examination of the synovial fluid or the synovial membrane. However, this is only helpful for assessing the activity of the inflammation, not for making a diagnosis.
Stages of rheumatoid arthritis
Rheumatoid arthritis is one chronic inflammatory diseasewhich is due to an excessive reaction of the body to the body's own cells. One can say that the immune system does not recognize the body's own cells and therefore fights them. The disease, which mainly affects the joints of the body, has four different stages.
- Stage: It usually comes to one symmetrical involvement of the metatarsophalangeal joints of both hands, as well as a Joint swelling. Also, patients with stage 1 rheumatoid arthritis complain of one Morning stiffnessthat is still present for more than 30 minutes after you wake up.
- Stage: there is an increasing Increase in connective tissue in the area of the affected joints and an increasing influx of inflammatory fluid in the joints. This results in an increasing limitation in the mobility of the joints when moving. It can also become a Protrusion of the joint capsule come, which can also severely impair the ability to move.
- Stage: It is already coming to Misalignments of the finger joints. The fingers are mostly pulled in the direction of the ulna of the forearm. The chronic inflammatory processes also gradually lead to one Destruction of the tendon sheathsAs a result, the muscles that move the fingers can no longer be moved without resistance. So-called Gooseneck deformations the finger (see subsection Rheumatism hand / hands).
- Stage: The final stage of rheumatoid arthritis occurs when the disease is advanced. It shows severe deformities and Destruction of the finger bones. Furthermore, in this disease state too other organs affected by the rheumatic disease be. In some cases, the heart or the lungs and the connective tissue can be affected. Due to the very good treatment options available today, very few rheumatism patients go through this stage today, as the chronic disease can be treated with medication in earlier stages.
Physical examination
In addition to the above Symptoms such as morning stiffness, Joint pain, The doctor finds it easy to get tired during the physical examination at the chronic polyarthritis (cP) characteristic clinical changes or deformities (rheumatism - related deviation of the joints).
The examination usually includes the examination of:
- Hand / hands
- Foot feet
- knee
- hip
- shoulder
- Elbow
- Spine
- Laboratory values
- roentgen
- Further diagnostic examinations
Rheumatoid arthritis in various locations
Rheumatoid arthritis of the hands

There are painful joint swelling of the wrist, metacarpophalangeal and median joints, mostly symmetrical on both sides of the body. The joints are sensitive to pressure, e.g. when shaking hands. It can restrict movement of the Wrists and fingers exist, so that the fist is no longer complete. The muscles of the ball of the thumb and little finger as well as the muscles of the palm of the hand can be diminished and weak. Tendon swellings or tears occur. With advanced disease, typical deformities in the hands occur:
- Hand scoliosis: Deviating from Carpal in the wrist outwards (ulnar = ellenwards),
- Caput ulnae syndrome: Protrusion and hypermobility of the elbow at the wrist
- Buttonhole deformity: Fixed flexion in the middle finger joint and overstretching of the end finger joint
- Gooseneck deformity: Hyperextension in the mid-finger joint and fixed flexion in the end-finger joint
- 90 ° / 90 ° deformation of the thumb: Fixed flexion in the thumb joint and overstretching of the thumb joint
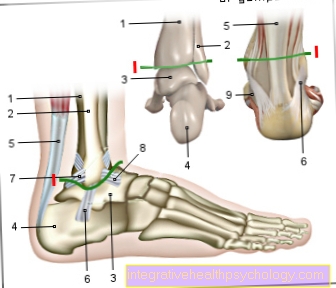
Rheumatoid arthritis of the feet
There is painful swelling of the ankle and toe joints, usually symmetrical on both sides of the body. The joints are sensitive to pressure. Tendon swelling occurs on the stretch side and behind the inner or outer ankle. With advanced disease, typical deformities occur in the area of the Feet:
- hallux valgus: Outward deviation of the big toe
- Hallux rigidus: Arthrosis of the metatarsophalangeal joint of the big toe with painful mobility and possible overstretching of the Big toe joint
- Hammer toe: fixed flexion of the toe joints
- splayfoot
- Windmill forefoot: Outward deviation of all toes due to rheumatic attack on the tendons and ligaments of the foot
- Flat buckle foot: also by softening the connective tissue through rheumatism
Further information can be found under our other topics:
- hallux valgus
- Hallux rigidus
- Hammer toe
- splayfoot
Rheumatoid arthritis in the knee
Mostly there is a soft tissue swelling and a Joint effusion with dancing patella (through the effusion in the Knee joint will the Kneecap (patella) lifted, which results in elastic resistance when pressure is applied to the kneecap), sometimes also one Baker's cyst in the hollow of the knee. The mobility in flexion and extension is limited. Muscle loss of the thigh muscle. Increasing instability can lead to If a or X - leg come. The consequences of this are usually one Gonarthrosis (Knee osteoarthritis). This often means a artificial knee joint be implanted.
Further information can be found under our other topics:
- Osteoarthritis of the knee
- artificial knee joint
Rheumatoid arthritis in the hip
A swelling is usually neither visible nor palpable. There is tenderness on pressure in the groin or over the outside of the thigh and the large hillock (greater trochanter). The mobility of the joint can be restricted. If this restriction occurs mainly in the morning, one speaks of Morning stiffness.
Consequences of long-standing rheumatism are usually osteoarthritis of the Hip joint (Coxarthrosis).Often there is a wandering of the acetabulum pool (Protrusio actetabuli). If the disease is severe, an artificial hip joint must be implanted.
Further information can be found under our other topics:
- Hip arthrosis
- artificial hip joint
Rheumatoid arthritis in the shoulder
There is a painful swelling, most likely to be felt from the front, as there is a relatively strong muscular jacket at the back Shoulder joint covered. The mobility of the joint is limited. The tendons surrounding the shoulder joint are usually painful on pressure, as is the ankle joint.
Rheumatoid arthritis in the elbow
Also in the area of Elbow If there is a painful swelling and movement of the joint, usually a stretch deficit.
Rheumatoid arthritis of the spine
Soreness from pressure occurs in the area of the spinous processes and in the area next to the spinous processes Musculature in front. Restriction of movement of the head and trunk. Depending on the position of the head, abnormal sensations in the arms, legs or trunk can occur. Sensory disturbances and Muscle weakness the arms and legs appear, as well dizziness, Nausea, or even difficulty swallowing or breathing.
Therapy (guidelines)
Some guidelines exist for treating rheumatoid arthritis. They all have a treatment of the complaints and symptoms with the so-called DMARD ("disease modifying antirheumatic drug ") Treatment. #
DMARD treatment is an anti-inflammatory drug treatment with a non-steroidal anti-inflammatory drug such as ibuprofen or diclofenac, as well as treatment with a steroidal, anti-inflammatory drug. This includes cortisone, which usually makes up a large part of the treatment for rheumatoid arthritis.
The line stipulates that treatment with an anti-inflammatory drug and with cortisone in combination should be started immediately if the diagnosis of rheumatoid arthritis is confirmed. Treatment should only be carried out under close supervision. The goal should be to curb disease activity as quickly as possible. The drug treatment may have to be adjusted. Cortisone preparations should be started with a lower starting dose than the starting dose. If the symptoms do not improve quickly, the medication should be increased rapidly.
The DMARD treatment also includes the drug methotrexate, which is also used and helps to reduce the immune system.
If the treatment with a DMARD does not achieve the desired success, a complementary treatment with a so-called biological should be started.
If symptoms improve with the individual or combined treatment, consideration should be given to reducing the medication gradually. However, it may be necessary that a certain basic medication must remain in place in order to draw out a relapse of the symptoms as far as possible.
In addition to these drugs, the anti-inflammatory drug Enbrel® can also help relieve symptoms
Read more on the subject here Therapy of rheumatoid arthritis
Biologics
The so-called biologicals have been used in the treatment of rheumatoid arthritis for several years. This term covers drugs manufactured using biotechnology. In the treatment of rheumatoid arthritis, mainly synthetically produced antibodies are used, which counteract the excessive immune system that triggers the symptoms of rheumatoid arthritis.
These include adalimumab, also known under the trade name Humira.
These so-called biologicals, which are also used for other diseases, are very expensive drugs. Since they would not get to their destination if they were taken in tablet form, they are given in the form of a syringe. The medication is usually injected into the muscle in the form of a depot syringe. Refreshing is done every few weeks or months. As a rule, the drugs are well tolerated.
Read more on the subject at: Biologics
Methothrexate
Methotrexate (MTX) is a Opponent of folic acid and inhibits a specific receptor. The drug is used on the one hand in the Cancer treatment but also in the Treatment of autoimmune diseases used. It ensures that the excessive immune system is throttled and that the strength of the rheumatism attacks is reduced or no longer takes place at all.
Methotrexate is used in the treatment of rheumatoid arthritis used when ibuprofen or diclofenac or cortisone do not lead to an improvement to the extent desired. MTX can be taken as a tablet or injected. While taking should be on a regular blood tests Pay attention and respond by changing the dose or discontinuing methotrexate in the event of abnormalities.
As a rule, MTX is well tolerated by the patient. Even so, there are some side effects that should be considered. One could be named increased susceptibility to infection, Pulmonary fibrosis, nausea and Vomit, Hair loss, Changes in blood count, Kidneys-, and Bladder damage such as Inflammation of the mucous membranes. In rare cases, it can also lead to a disorder of the central nervous system. When taking methotrexate, pregnancy must be ruled out beforehand. The drug is prescribed by the rheumatologist.
Naturopathy
In addition to conventional medical treatment of rheumatoid arthritis, there are also some naturopathic approaches that can be given at least in addition to conventional medical drugs. Naturopathic approaches have been used more and more in recent years. Naturopathic substances should always parallel to the conventional medical are given. This combination ensures that the Effect of conventional medicine improves will, but also the Side effects of these drugs reduced can be.
The has long been used in the accompanying rheumatism treatment Hydrotherapy. This means a Bath therapy as well as the well-known Kneipp therapy.
Even treatments with Healing mud (Fango) and cold and warm Castings are used in hydrotherapy. They ensure that rheumatism attacks occur less often and heal more quickly after they occur. The intensity the rheumatoid flare-up is also under the hydrotreatment reduced.
Naturopathic treatment also includes the right nutrition. You should above all little meat and fat and a lot of fish include. All products that are rich in arachidonic acid and omega 3 fatty acids are very suitable for a diet that counteracts rhematoid arthritis. Fasting is also always mentioned when it comes to the effects of diet on the development of rheumatism. Prior medical advice is important. The start of a fast should be carefully considered.
For more information, see: Diet for rheumatism
Abstract rheumatism
The Rheumatoid arthritis is the most common rheumatic disease with chronic inflammation of the synovial membrane, tendon sheaths and Bursa. The course is usually progressive in bursts. Starting with painful swellings and overheating, tenderness and restricted movement of joints, the rheumatoid arthritis / rheumatoid arthritis can lead to the complete destruction of joints and tendons.
The diagnosis is made on the basis of the symptoms and the physical examination findings. Should support the diagnosis Laboratory values such as X-rays of the affected joints.
On the one hand, the therapy is medicinal, and on the other hand, various surgical procedures are available. The aim of the therapy is to slow down the inflammatory process, relieve pain and, if possible, maintain the function and strength of the joints. Physiotherapy, occupational therapy and physical measures are also used.















.jpg)