Cracked skin
introduction
The skin is the largest and probably the most sensitive organ in the human body. On the one hand, it forms an indispensable barrier and protects the sensitive inside of the body from harmful environmental influences. On the other hand, our skin mediates temperature regulation, pain, touch and temperature senses.

Due to the sebum glands it contains, it constantly produces a protective, oily film that ensures that the skin does not become too dry. There are different skin types. On the one hand, the skin may tend to produce too much sebum (oily skin) or too little (dry skin). A so-called “mixed form” exists when both forms occur side by side.
Internal or external causes can lead to dry, cracked and rough skin. In addition to cosmetic aspects, those affected often suffer from itching, a feeling of tension and even pain. Thorough research into the causes, appropriate care and good therapy are therefore absolutely recommended for cracked skin.
Read more on the topic: Brittle hands
Diagnosis and symptoms of cracked skin
Cracked skin is very common on areas of the body that tend to dry out, such as the hands and feet. These skin areas have a reduced number of sebum glands.
Here, very small tears appear in the dry skin, which, as the skin dries out, grow larger and can become inflamed. Then they cause uncomfortable pain in the person concerned. There may also be a feeling of tension.
The skin often feels very rough and can cause itching. If dry skin is itchy, it may be eczema. Dandruff can also occur.
With good care or avoidance of the triggers, the skin condition can often be significantly improved. Sometimes, however, an exact medical diagnosis must be made in order to be able to choose the best possible therapy options.
Therefore, if your cracked skin has the following characteristics, you should definitely consult a dermatologist:
- Pain, stronger itching, intense Redness
- inflammation
- Accompanying symptoms (e.g. Hair loss, Nail discoloration etc.)
- General Feeling sick
In order to clarify possible causes of the cracked skin, the dermatologist can carry out various examinations. Besides the inspection, can be a detailed survey (anamnese) Provide information. In addition, small Tissue sampling (biopsy) or various Allergy tests are used.
Causes of Chapped Skin
Cracked skin has numerous causes. In addition to external factors, various skin diseases can lead to cracked skin.
1. Cold and wind
Healthy skin has a very thin, natural protective film, the so-called "Hydro-lipid coat", consisting of sebum, sweat and other metabolic products. It covers the entire surface of the skin and prevents dehydration and the colonization of undesirable germs. Cold winter air damages the hydro-lipid coat and the skin loses valuable moisture.
At below 8 degrees Celsius, the sebum glands stop their activity. In addition, warm and dry heating air removes moisture from the skin, so that dry and chapped skin quickly occurs. Cracked areas can easily develop, particularly in unprotected areas such as the face and hands.
2. Excessive use
Our hands in particular are strained in many situations. Strong cleaning agents, chemicals, soaps and, above all, excessive hand washing can lead to cracked hands. Forced cleaning of the hands with e.g. Although brushes and washing salt remove dirt, they put an unnecessary strain on our skin. In addition, if conventional soaps are used too often, the horny layer swells and the fats and other protective substances are washed out, so that the skin becomes easily dry and cracked.
3. Contact eczema
Rubber gloves, cosmetics, latex, cleaning agents, metals, soap, solvents, etc. can cause so-called "allergic contact eczema". In this extremely common skin disease, individual substances trigger a type IV ("delayed type") allergic reaction. Those affected suffer from cracked, flaky and reddened skin, as well as itching. During the acute phase, small vesicles or nodules can also be observed. Particularly frequently affected are e.g. Hairdressers or cleaning staff, as they often come into contact with allergenic substances such as dyes or cleaning agents in everyday work.
4. Neurodermatitis / atopic eczema
Neurodermatitis, often also called atopic eczema, is characterized by extremely dry and reddened skin, combined with severe itching. Inadequate care or therapy can cause the skin to crack. In the worst case, the affected areas can even burst and bleed! Most patients fall ill in infancy or toddlerhood ("cradle cap") and experience a relapsing course of the disease. Currently, there are still no adequate explanations for the exact origin of the disease. However, allergic reactions seem to play an important role. Various substances or situations (pollen, animal hair, stress, weather changes, cleaning agents, etc.) can provoke a "flare" of the disease. In addition, neurodermatitis occurs more often together with diseases such as bronchial asthma or pollen allergy. Overall, atopic eczema can be extremely agonizing for those affected because, in addition to dry and cracked skin, sometimes extreme itching (lat. Pruritus) is available. The flexor sides of the arms and legs, face, neck and neck are among the particularly afflicting areas of the body.
Since the natural protective cover is disturbed in neurodermatitis, the skin can be extremely susceptible to various infections with pathogenic germs. These so-called "super infections" are among the most significant complications of the disease.
5. Athlete's foot
Athlete's foot (Foot mycosis) is the most common fungal disease in our latitudes. In swimming pools, communal showers, saunas or changing rooms, those affected get infected with the annoying disease extremely easily and quickly. Redness, slight itching and flaking mark the beginning of athlete's foot. As it progresses, cracks form in the spaces between the toes, followed by blistering and extensive detachment of the skin. Sometimes, the said fungi can also spread to the palms of the hands and lead to cracked skin there (Hand mycosis). Frequent wearing of synthetic protective gloves or wet work with the hands have a positive effect on the development of the disease.
This is how cracked skin is treated

Based on the various causes of cracked skin, the therapy is aimed at the underlying cause.
1. Protection against the cold
Protect sensitive areas of the body from wind and cold to prevent cracked skin. In particular The face and hands are particularly vulnerable! Warming gloves and consistent skin care with moisturizing creams protect your skin from the cold winter air. humidifier or damp towels on the heater, have a positive effect on the dry heating air.
2. Care for stressed skin
Our skin has to withstand many stresses in everyday life and at work. However, targeted care can support their ability to regenerate and prevent cracked skin. Use for Wash your hands ideally with lukewarm water and mild, pH-neutral soap. For example, if you If you work in the medical field and very frequent hand washing is an absolute must, you should regularly moisturizing hand lotions use. So that your hands are not in direct contact with e.g. It is recommended to wear protective gloves.
3. Treat contact eczema
The best therapy for contact eczema is this consistent avoidance of the triggering substances, there one Desensitization ("Allergy Therapy"), e.g. with hay fever, not possible is. Gentle skin cleansing and rich, oily creams can help with cracked skin caused by eczema. If there is inflammation in addition to cracked areas, anti-inflammatory ones can also be used Anoint be helpful to rebuild the lost skin barrier. In particularly acute cases, the use of cortisone Preparations to be thought about.
4. Get a handle on neurodermatitis
Nowadays, eczema sufferers are available numerous therapeutic approachese available. What ultimately helps each individual can be extremely different. Basically, the main triggers should always be eliminated or avoided. Good skin care, such as. Urea-containing creams and ointments, gentle cleaning and consistent refatting of the cracked skin areas are to be considered useful in any case. Many of those affected continue to feel Bath therapies as beneficial. During particularly bad phases or inflammation of the cracked skin, can Cortisone ointments are used. Sometimes it is even necessary to have an internal one medical therapy with e.g. Steroids, Calcium or antiallergic substances to start. In addition to the conventional medical measures mentioned, there are a large number of naturopathic and homeopathic therapy principles.
5. Fight athlete's foot
In almost all cases, help with athlete's foot special, so-called antifungal ointments and creams. These anti-athlete's foot ointments are available without a prescription in any pharmacy and must be applied to the affected areas several times a day. In rare, very pronounced cases, antifungal tablets must also be taken.
forecast
At long last The prognosis of cracked skin varies depending on the cause. By consistently avoiding triggering factors, the skin quality improves significantly in most cases.
Atopic dermatitis, on the other hand, can often become a lifelong burden and challenge for many sufferers. Unfortunately, complicated processes are not uncommon and challenge our modern medicine every day. Fortunately, the disease has been the subject of much research and the prognosis is steadily improving.
prophylaxis
True to the motto "As thoroughly as necessary and as gently as possible" our skin should be cleaned to prevent cracked areas.
Regular, individually tailored care is another important pillar in prophylaxis. It is also important not to "overcare" the skin with too many products at the same time, as e.g. Contact eczema can develop.
If your skin is prone to cracking, don't hesitate See a dermatologist. He will be happy to give you valuable tips on prevention or treatment.
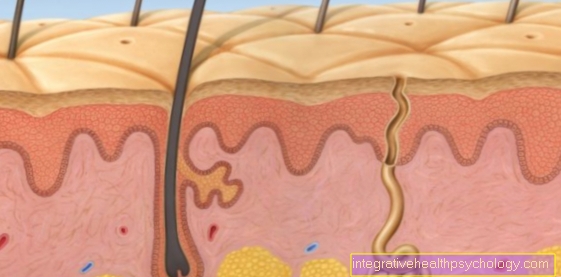
Anatomy of the skin
Overall, our skin consists of three layers: Subcutaneous tissue (lat. Subcutis), Dermis (lat. Corium, Dermis) and Epidermis (lat. epidermis).
The deepest layer, the subcutaneous tissue, is mainly found Adipose and connective tissue. It represents the most important energy reserve and fulfills important tasks in the Thermoregulation of the body.
The connective tissue dermis forms the middle layer and can be divided into Network layer (lat. Stratum reticular) and Cone layer (lat. Stratum papillary) organize. Their composition is decisive for whether our skin looks smooth, fresh, wrinkled, dry or even cracked. Next Blood vessels, sebum and sweat glands, there are numerous Sensory receptors resident. They convey important functions such as touch, sense of touch, pain and temperature sensation. The epidermis is located on the surface of the skin and can be divided into 5 zones (Stratum basale, St. spinosum, St. granulosum, St. lucidum and St. corneum) organize. Essentially, it forms the actual protective barrier against the environment.
Figure skin
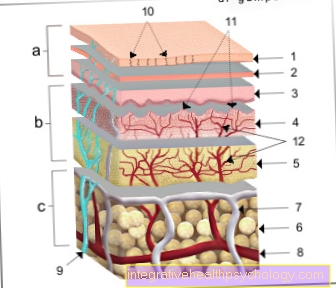
a - epidermis (1st - 3rd) - epidermis
b - dermis (4th - 5th) - Dermis
c - subcutaneous tissue (6.) - Tela subcutanea
- Horny layer - Stratum corneum
- Cornifying layer
(light layer
and granular layer) -
Stratum lucidum and
Stratum granulosum - Germ layer (prickly cell layer
and base layer) -
Stratum spinosum and
Stratum basale - Papillary layer -
Stratum papillary - Network layer - Stratum reticularre
- Subcutaneous tissue - Tela subcutanea
- Lymph vessel - Vas lymphaticum
- Artery - Artery
- Cutaneous nerve - Cutaneous nerve
- Duct of a sweat gland -
Ductus sudorifer - Papillae of the dermis -
Papillae (dermidis) - Vascular network of the dermis -
Subpapillary venous plexus
You can find an overview of all Dr-Gumpert images at: medical illustrations