Therapy of inflammation of the pancreas
introduction
When treating pancreatitis, a distinction must first be made between what type of disease it is. The attending physician must therefore determine whether it is the
- acute or the
- chronic form.
The therapy of pancreatitis (Pancreatitis) can either:
- conservative (non-operative)
- endoscopic (minimally invasive) or
- done by surgery.

Acute pancreatitis
Non-operative therapy
Since acute pancreatitis is usually associated with severe pain and involves serious dangers, treatment is generally carried out in hospital.
In the case of very severe forms, a stay in an intensive care unit is inevitable.
In not a few cases, such a disease results in what is known as circulatory shock, in which the patient concerned is given blood reserves and / or infusions to compensate for the drop in blood pressure.
To relieve the severe pain, people who have an acute inflammation of the pancreas (acute pancreatitis) are given anticonvulsant and analgesic medication, which is usually administered to the body via the vein.
Furthermore, in the course of a glandular relief, it is necessary to refrain from eating for a certain period of time (2 - 5 days). During this time, the increase in fluid and nutrients occurs entirely through the blood or a small intestinal tube. This bypasses the natural digestive system with the involvement of the pancreatic enzymes.
After improvement of the symptoms and relevant blood values, a therapy phase begins, in which the slow diet begins. The patient is given a light one for a few days Light food, which is then increased. In many cases it also makes sense to give the patient enzyme preparations to reduce the pancreas continue to relieve.
alcohol should be used throughout the treatment period in no casel be consumed.
In the case of severe forms of acute pancreatitis, it is useful antibiotic take and thereby the risk of infection to minimize.
Operative therapy
In the course of an acute pancreatitis it can happen that a lot of tissue dies. In such cases, the non-surgical therapeutic measures are insufficient to remedy the critical situation of the patient. The dead pancreatic tissue must be surgically removed.
Chronic pancreatitis
Non-operative therapy

Since the consumption of alcohol plays a major role in the development of chronic pancreatitis (chronic pancreatitis) in many of those affected, it is imperative that these patients refrain from alcohol for their entire life.
A diet and a change in food intake also lead to a significant improvement in symptoms in the majority of cases and ultimately to recovery of the pancreatic tissue.
People who suffer from this form of pancreatitis are supplied with pancreatic enzymes and various vitamins (e.g. vitamins A, D, E and K; fat-soluble vitamins) from outside for life. This measure brings about permanent relief of the gland, since it only has to and / or can produce less enzymes itself. During the episodes of acute episodes, this form of the disease is treated in the same way as ordinary acute pancreatitis.
Surgical therapy
The non-surgical treatment measures are not always sufficient to keep the patient symptom-free.
Now it becomes necessary to resort to surgical intervention. The attending surgeon can, if necessary
- expand narrowed ducts of the pancreas,
- create an artificial passage to the small intestine and / or
- Remove dead parts of the pancreatic tissue.
Minimally invasive therapy
-
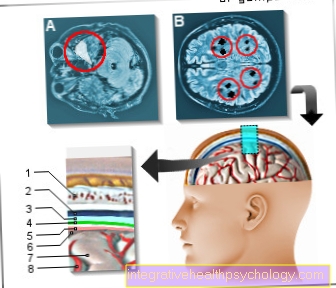
Are there inflammation of the pancreas (Pancreatitis) Underlying gallstones, which are common ducts of bile and pancreas (Common bile duct) clog, they must be removed.
This is now done using an endoscope. This is advanced through the intestine to the exit point of the common bile duct in the duodenum. The exit point is now opened by means of a small incision so that the stones can exit. -
In the case of an abscess of the pancreas (accumulation of pus due to bacterial inflammation), this is suctioned off and then rinsed. An abscess is an encapsulated collection of pus.