Therapy diabetes mellitus
Synonyms in a broader sense
Sugar, diabetes, adult onset diabetes, type I, type II, gestational diabetes
Literal translation: "Honey-sweet flow"
English: diabetes
Therapy diabetes
A close take on the Blood sugar level The primary goal of therapy is to achieve an almost normal range, since in this way the development and progression of late-stage diabetic complications can be prevented or delayed.
It is important that the patient get the disease diabetes into his life and is aware that he is responsible for controlling his metabolism. The patient has to continuously and independently implement the therapeutic measures because the natural control loop has become inoperative.
These include metabolic self-controls, physical activity, and avoidance of risk factors such as Smoke, Obesity or high blood pressureto keep the risk of vascular changes low.
A comprehensive therapy, which restricts the patient as little as possible, should be aimed for, especially in young type 1 diabetics.

General measures that belong to the therapy of diabetes mellitus are as follows:
- Diets and weight normalization,
- physical activity, as it increases the sensitivity of muscle cells to insulin,
- Refraining from / reducing nicotine and alcohol.
Further diabetes-specific therapy options are:
- Medication: oral anti-diabetic drugs or insulin
- Training the patient
- Measures to avoid complications (prophylaxis) and therapy for the same.
All of these measures aim to create a metabolic situation that is similar to that of a healthy person (normoglycemic metabolism).
Read more on the topic: Abandonment of insulin
The fasted blood sugar level should be between 90 and 120 mg / dl, before and 2 hours after the meal the blood sugar level should be below 130 mg / dl and one hour after the meal it should be below 160 mg / dl.
The diabetic's urine should contain neither glucose nor ketone bodies.
Normalizing body weight and blood lipid levels is critical to avoiding diabetes complications.
Target values cholesterol
The setting of the blood lipid values should correspond to the following values
- Total cholesterol <180 mg / dl (<4.7 mmol / l)
- LDL cholesterol below 100 mg / dl (below 2.6 mmol / l)
- HDL cholesterol above 35 mg / dL (above 0.91 mmol / L)
- Triglycerides (fats) below 150 mg / dl (below 1.7 mmol / l)
The desired value for the diabetes - setting - long-term parameter HbA1c ("sugar memory") is below 6.5% (for an explanation of the parameter see "Course and prognosis").
Further Risk factorswhich, in addition to diabetes, promote vascular changes, should be switched off. Specifically, this means that the Smoke set and the Blood pressure readings of the patient should be reduced to deeply normal values (below 130/80 mmHg).
Medical studies show that lowering the anterior systolic blood pressure value by 10 mmHg reduces diabetic complications by 12%.
In addition to all of these preventive measures, it is important that the patient become aware regular examinations to the doctor (internist / family doctor). Any late complications of the sugar disease can be identified and the doctor has the opportunity to initiate appropriate therapy immediately.
An extensive Diabetes education should be done as soon as the diagnosis "diabetes" is made, because only then does the patient know how to deal with the disease and can actively carry out the therapy. As part of this training, the patient is explained the clinical picture and receives important information about treatment. The right diet, the use of medication and the determination of the blood sugar level are part of the training course, and what to do in an emergency "Hypoglycaemia“Discussed and measures to avoid Consequences of diabetes shown. The health insurance pays the costs for this!
Specific therapy for type 1 diabetes
The treatment of type 1 diabetes is based on insulin injections under the skin (subcutaneous injection) with the help of so-called “pens”, since insulin cannot be taken as a tablet due to its instability to the acid in the stomach.
Diet, physical activity and intensive patient education are also part of the therapy.
The patient's food and insulin supply must be optimally coordinated so that a normal high blood glucose level is achieved over the long term. A distinction is made here between conventional and intensified conventional insulin therapy and insulin pump therapy, which is a form of intensified insulin therapy.
The patient must be at the conventional therapy Use intermediate or mixed insulin to adapt your meals to a strictly prescribed insulin therapy schedule:
He administered insulin twice a day, namely 2/3 to ¾ of the required daily dose before breakfast and the rest before dinner, with an interval between injection and eating of 30 minutes. This means that the insulin is injected and should not be eaten for 30 minutes afterwards. This procedure results in optimal insulin action.
The rigid meal schedule must be adhered to, as the patient injects a certain dose of insulin and "intercepts" it with the meals.
So the patient has to eat because he has injected insulin. If he eats too little, his insulin dose is too high and he goes into a state of hypoglycaemia; if it is too much, on the other hand, his insulin dose is too low and too much glucose remains in the blood.
The therapy of hypoglycemia consists in the administration of glucose and in hypoglycemic shock 1 mg glucagon must be injected into the upper arm muscle (intramuscular injection) or under the skin (subcutaneous). Because of the possible occurrence of such an emergency, the relatives or the patient's environment should be informed about the disease and familiarized with the emergency treatment.
The intensified conventional insulin therapy of type 1 diabetes is based on the basic bolus principle. The amount of insulin that the patient needs during the day is divided into a basic amount (BaseBolus principle) of insulin and additional, meal-dependent doses of insulin (basicBolusPrinciple). An intermediate insulin is given twice a day for the basic insulin supply, which covers 40-50% of the total daily insulin dose. The other 50 - 60% are divided between the meal-related bolus doses, which consist of regular insulin or a short-acting insulin analog. The amount of the individual doses before meals depends on the size of the following meal, the time of day (the body's insulin sensitivity varies depending on the time of day), the upcoming physical activities and the blood sugar level measured before meals (preprandial blood sugar level).
Since all these components have to be considered in this form of therapy, good training and a high sense of responsibility on the part of the patient are required. In contrast to conventional therapy, there is no need to maintain a spray-eating distance, as normal insulin or short-acting analogues take effect immediately.
The Insulin pump therapy takes place by means of an external pump, i.e. the device that delivers regular insulin under the skin is outside the body. The pumping device is the size of a cigarette pack and can e.g. worn attached to the belt. The basal rate delivered by the device is programmable and is automatically delivered to the patient. The bolus doses for the individual meals are called up by the patient himself, depending on the desired amount of food and the previously measured blood sugar value.
The indication for choosing this form of therapy is pregnancy and impending late complications of diabetes. Also read: Gestational diabetes
Possible complications are:
- local infections
- Derailment of the metabolism with blocked insulin flow and
- Hypoglycaemia with insufficient blood sugar self-control.
The prerequisite for the two intensified forms of insulin therapy is that the patient is cooperative and is able to make therapeutic decisions himself. In addition, he must be well trained and instructed in the function of the device and carry out at least 4 blood sugar self-checks every day. The care of the patient should be in the hands of a doctor with experience in diabetes (usually a specialist in internal medicine). The advantages are that an optimal metabolic control can be achieved and that an individual timing of food intake is possible, which offers young people in particular more freedom.
Specific therapy for type 2 diabetes
Type 2 diabetics should receive a phased therapy structured in stages.
The first stage and most important therapeutic measure is Weight normalization to mention that through a diabetic diet and regular physical activity (endurance training) should be achieved and maintained.
There are basically two different therapeutic approaches to drug therapy for diabetes mellitus.
- On the one hand, you try to use drugs that you have to take to reduce the residual function of the pancreas To support as much as possible that the amount of insulin still produced is sufficient for daily needs.
- On the other hand, if the pancreas is no longer able to produce enough insulin, you can inject the insulin from the outside in various forms.
The second stage involves the beginning of a drug therapywhen the disease cannot be stopped by weight loss. Obese patients received Metformin (e.g. Glukophage® Mode of action: Delayed glucose uptake from the intestine and decreased appetite), normal weight patients Sulfonylureas (e.g. Euglucon N® Mode of action: Stimulation of insulin release from the pancreas) as oral antidiabetic drugs.
If the diabetes setting with the individual preparation is not satisfactory, a second medication is added in the third therapy stage, usually Acarbose (e.g. Glucobay® Mode of action: Glucose breakdown in the intestine is delayed) or Glitazone (Mode of action: Increase in the sensitivity of cells to insulin).
If therapy with the drugs mentioned fails, conventional or intensified insulin therapy, i.e. injecting insulin.
For more information, see
- Drugs diabetes mellitus
and - Type 2 diabetes.
Complications
Possible complications of insulin therapy are Low blood sugar (hypoglycaemia) in the event of an insulin overdose or increased physical activity. Possible signs of a hypoglycemic condition include:
- Racing heart
- nausea
- weakness
- Restlessness
- a headache
- big appetite
- Tremble
- sweat.
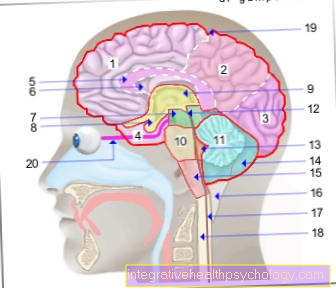
Since from a blood sugar level below 40 mg / dl the supply of the Brain is no longer sufficiently guaranteed with glucose, such low blood sugar levels lead to hypoglycemic shock.
If the diabetic notices the signs of hypoglycaemia, he should check his blood sugar and, if necessary, consume glucose or fruit juices.
Another possible complication is that fat cells accumulate under the skin at the injection sites and can cause hardening (Lipodystrophy).
A Insulin resistancei.e. an increased need for insulin due to insufficient effect on the target organs can occur. It's mostly done Obesity justified.
Diabetic secondary diseases, i.e. Diseases that result from diabetes are caused by the chronically high blood sugar levels and cause changes in the blood vessels. So-called microangiopathic changes, in which the small vessels of the body are affected, often occur on the kidney, the Retina and in the nervous system.
In addition, larger vessels under the Macroangiopathy be affected, e.g. the Coronary arteries or the Arteries of the legs, with the risk of Heart attack and Circulatory disorder.
Long term complications
Frequent concomitant and secondary diseases in type 2 diabetics
- 75.2% hypertension
- 11.9% damage to the retina (retinopathy)
- 10.6% damage to the nerves (neuropathy)
- 9.1% heart attack
- 7.4% circulatory disorder (peripheral arterial occlusive disease (PAD))
- 4.7% apoplexy (stroke)
- 3.3% nephropathy (Renal failure)
- 1.7% diabetic foot
- 0,8% Amputation of limbs
- 0.3% blindness