Therapy sleep apnea syndrome
Sleep apnea syndrome therapy
The main purpose is to reduce body weight (diet) contributes to lowering blood pressure Sleep apnea syndrome and the breathing pauses in sleep itself:
Weight loss leads to a reduction in the severity of the disease. Patients can preferably lie on their side to sleep in order to achieve better breathing. Of the Refrain from alcohol, smoking and certain medicationsthat promote apnea (e.g. sedatives or sleeping pills) can lead to better sleep. The sleep apnea syndrome patient should be on good Sleep hygiene pay attention, i.e. Have a regular sleep schedule and avoid strenuous activity or eating greasy food before bed.

If there is no significant improvement in the nocturnal breathing pauses, the patient with sleep apnea syndrome can have a so-called sleep syndrome CPAP treatment to be helped. CPAP stands for "Continuous positive airway pressure", ie for "constant positive airway resistance". The CPAP treatment works as follows:
The patient wears a mask over the therapy during sleep nose, possibly also over the mouth. The mask is pressed onto the nose or nose and mouth using headbands. The mask is connected to a device that generates positive pressure so that a continuous pressure is applied to the patient's airways via the mask.
This pressure is used to keep the airways open. Without the therapy, the airways would slacken in the area of the throat, so that less oxygen-containing air per breath enters the lung got. This method can be used very effectively to eliminate airway instability and at the same time lead to an improvement in the quality of life, restful sleep at night, reduced daytime sleepiness and a lowering of blood pressure. The patient with sleep apnea syndrome should wear the mask regularly at night in order to improve the symptoms.
Treatment controls are carried out at regular intervals: The patient is monitored in the sleep laboratory during ventilation with CPAP in order to check the success of the therapy with this method, because the patient should benefit from the sleep apnea syndrome therapy and experience an improvement in symptoms!
If the patient has nasal polyps or a sloping nasal septum, these breathing obstacles in the area of the upper airways can be removed by an operation, which leads to an improvement in breathing during sleep.
What therapy options are available?
Depending on the risk profile of the person affected, various therapeutic measures can either lead to a cure or at least to a more significant improvement in the symptoms and thus to a reduction in the incidence of secondary diseases.
Note
This topic is the continuation of the topic
- Sleep apoee syndrome
General information on this topic can be found there!
Basic therapy (conservative therapy) for mild forms and the corresponding patient profile:
Weight reduction; Avoidance of alcohol (at least in the 2 hours before going to bed), nicotine as well as sleep and sedation medication; Observance of a regular sleep cycle; possibly avoiding a supine position during sleep, in which the tongue falls backwards due to the force of gravity and represents a relevant airway barrier in the case of low muscle tone.
A positive effect of theophylline, a drug that increases the central respiratory drive, is also described.
Mechanical therapy (apparatus therapy) for mild to severe forms and the corresponding patient profile:
- (Nasal) Continuous Positive Pressure Ventilation (nCPAP)
In (nasal) ventilation therapy using CPAP (continuous positive airway pressure), a breathing mask (usually a nasal mask) creates a slight overpressure in the upper airways, from the nasal entrance to the windpipe, so that they are kept open permanently. In this context, one speaks of a “pneumatic railing”. Ventilation takes place with room air; additional oxygen treatment is possible.
A large number of systems from different providers are available. The individual setting takes place in the sleep laboratory or on an outpatient basis. If necessary, adjustments, e.g. in case of weight changes, necessary.
As a rule, the ventilation system must be used every night and for life. This can be found annoying. One of the side effects that can occur is a drying out of the mucous membranes in the nasopharynx, which in turn can be countered with an additional humidifier.
Since the counter pressure generated by the CPAP machine when you breathe out can be strenuous, switching to a BiPAP machine is an alternative. This is a self-regulating system in which the pressures during inhalation and exhalation are continuously monitored and adjusted.
- Bite splints (mandibular protrusion splints)
This keeps the airways open by slightly shifting the tongue, soft palate and jaw forward.
- Game brace
A palatal brace is a device that can be used while you sleep to prevent snoring and sleep apnea. Such a snoring clip has an omega shape and fits the palate.
If you are interested in this topic, read more about it under: Palate Brace - How is it used?
- Nasal aids (e.g. nasal plasters)
Used for the external or internal enlargement of the nasal atria. Their effect is very controversial. The prices for such products are very different. You can usually get cheap offers from internet pharmacies.
Surgical therapy (surgical measures) in severe forms and the corresponding patient profile:
Invasive or minimally invasive surgical interventions that are ultimately intended to remove obstructions. They can also be performed in addition to nasal ventilation therapy or enable this in the first place. The following are conceivable:
- Nasal and sinus surgery:
Nasal septoplasty or correction of the Nasal septum with curvature (Septal deviation), Removal of growths (Polyps), Nasal concha.
- Oral surgery measures:
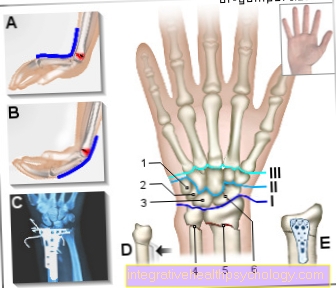
Forward shift of upper jaw and Lower jaw by maxillo-mandibular osteotomy (MMO). Requires an operation under general anesthesia and inpatient follow-up treatment.
- Operations on the soft palate:
such as. uvulopalatopharyngoplasty (UPPP):
A surgical procedure to remove excess tissue from the uvula, tonsils, and parts of the soft palate.
- Operations on the tongue and tongue base:
During lingual plastic surgery or glossectomy, parts of the posterior tongue are removed in order to enlarge the space there.
- Removal of tonsils (tonsillectomy)
The tonsils are often the focus of recurring inflammatory processes (p. Tonsillitis).
As a result, they tend to enlarge (overgrowth, hypertrophy, kissing tonsilles). In some cases the almond enlargement can favor the creation of a negative pressure in the throat and a snoring favor. In such cases, the ENT doctor recommends removing the tonsils.