Tibialis posterior syndrome
Introduction - what is tibialis posterior syndrome?
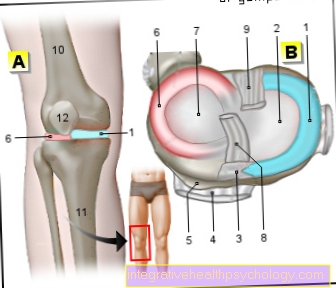
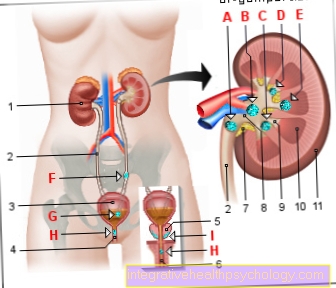
The tibialis posterior syndrome is derived from the tibialis posterior muscle of the same name. This is located directly behind the shin (tibia). Its tendon runs along the back edge of the inner ankle of the foot. In a healthy state, the muscle ensures that the heel is straight when walking, running and standing. This prevents the heel from buckling inwards (overpronation / pronation).
Muscle and tendon can be damaged due to various causes, which is known as tibialis posterior syndrome. The longitudinal arch of the foot sinks and the acquired flat foot develops. Women are more likely than men to develop tibialis posterior syndrome, although the exact cause is not known. It is believed that hormonal changes in women affect the stability of muscles, tendons and ligaments.
Read more about the topic here: Correction of a flat foot

Causes of tibialis posterior syndrome
The causes are varied. In addition to rheumatic diseases, traumatic sports injuries and accidents involving the tibialis posterior muscle and its tendon are the main reasons. At the same time, constant, chronic incorrect and overstressing of the foot worsen the symptoms. Patients who suffer from diabetes mellitus, overweight, high blood pressure or who have been taking cortisone for a long time have a higher risk of developing the disease.
Untreated foot deformities such as B. a buckle foot in children and adolescents can lead to a tibialis posterior syndrome in later adults.
By jogging
When jogging, about twice the body weight acts on muscles, tendons and ligaments. If an athlete has an untreated foot deformity (e.g. flat foot) or a muscular imbalance, excessive jogging leads to the occurrence of tibialis posterior syndrome. Therefore, you should pay attention to the right choice of running shoes when jogging. At the same time, special insoles must be worn if necessary in order to avoid excessive and incorrect stress on the musculoskeletal system (muscles, tendons and bones).
Find out more about the topic: Orthotics for the foot
These symptoms indicate tibialis posterior syndrome
The symptoms can vary individually. In most cases, there is pain on the inside of the inner ankle that is independent of the load, whereby the pain can also radiate to the outer ankle and the entire lower leg. In addition, swelling and warming occur along the tendon of the tibialis posterior muscle on the medial malleolus. Many patients also describe muscle weakness and tiredness in the affected foot.
You can find out more about the topic here: Pain in the feet - what can it be?
Inflammation of the tibialis posterior tendon
Chronic, pathological incorrect loads or misalignments lead to constant excessive and incorrect loads on the feet. The muscles involved respond with pain, hardening and shortening.
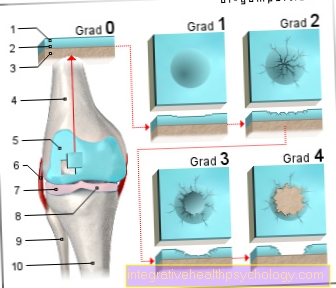
In the area of the tendon of the tibialis posterior muscle, there is initially massive swelling and inflammation. If these are not treated quickly and adequately, small longitudinal tears will form in the tendon over time, which ultimately leads to its tearing (rupture). In this case the longitudinal arch of the foot collapses completely and the acquired flat foot develops.
Read more about the topic here: Tendonitis of the tibialis posterior tendon
Diagnosis of tibialis posterior syndrome
A precise clinical examination of the affected foot is of enormous importance for the diagnosis. The practitioner pays particular attention to the prevailing, known foot misalignments, painful pressure points and swellings in the tendons. In addition, an X-ray examination should be carried out under stress, since irregularities in the anatomy of the foot and misalignments can be detected.
Treatment of tibialis posterior syndrome
Treatment and therapy depend on the extent of the damage. Basically, protection, cooling and a reduction in stress are advisable. Furthermore, an individual supply of insoles for the patient is important to correct existing foot deformities.
Physiotherapy, targeted muscle building training of the calf and shin muscles as well as cold therapy can help improve the symptoms. The use of anti-inflammatory, decongestant drugs such as B. Ibuprofen are helpful in the acute phase. The injection of cortisone directly into the affected tendon should only be done once, if at all, as this can further damage and weaken the tendon and its structure. Care should also be taken to wear sturdy shoes. If all conservative, non-surgical methods lead to no improvement, surgical intervention is the last alternative.
Exercises for tibialis posterior syndrome
Special exercises for the entire foot and lower leg muscles can have a positive effect on the course of a tibialis posterior syndrome. These should be individually tailored to the patient and should be supervised and controlled by an experienced physiotherapist at the beginning of treatment. In principle, well-developed muscles protect the musculoskeletal system from damage.
Duration of the tibialis posterior syndrome
The duration of tibialis posterior syndrome depends on the severity of the condition and on early diagnosis and treatment. If it is recognized and treated too late, many structures are usually irreparably damaged as a result. In this case, only a surgical intervention can often help.
Prognosis of tibialis posterior syndrome
The earlier the diagnosis is made and treatment started, the better the prognosis. If there is continuous incorrect and overstressing over a longer period of time, this leads to further damage to muscles, tendons, bones and ligaments.
Find out more about the topic: Insoles for flat feet
Tendon tear complication
Tendons initially react to incorrect stress with swelling, warming and inflammation. If this is not treated, longitudinal tears can develop, which over time lead to the tendon rupturing. In the case of the tibialis posterior tendon, the longitudinal arch of the foot collapses completely, the stability of the foot is reduced, and ultimately the acquired flat foot develops.
You can find out more about the topic here: Tendinitis in the foot