Toxic megacolon
definition
The toxic megacolon is an acute, life-threatening clinical picture which can occur as a complication in other intestinal diseases such as Crohn's disease, ulcerative colitis, Chagas disease, and pseudomembranous colitis.
The toxic megacolon is an enlargement of the large intestine accompanied by severe colon inflammation. Those affected often come to the emergency room with acute, severe abdominal pain and fever and need intensive medical care.
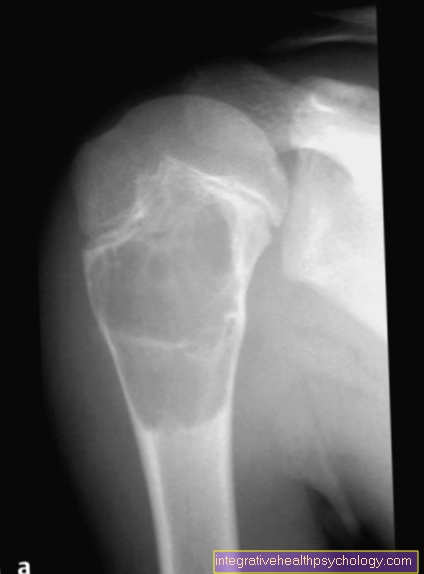
This complication rarely occurs. The diagnosis is confirmed with X-rays.

Causes of the formation of a toxic megacolon
The causes of a toxic megacolon are in many cases chronic or infection-related, inflammatory diseases of the large intestine.
Ulcerative colitis is one of the chronic diseases. This is a chronic inflammation that spreads continuously through the intestines and usually breaks out between the ages of 20 and 40. The disease manifests itself in bloody diarrhea and colicky abdominal pain, which occur in bursts.
Another chronic inflammation of the bowel is Crohn's disease. This is very similar to ulcerative colitis, but mostly affects isolated sections of the intestine and is therefore not continuous. The entire gastrointestinal tract can be affected. The disease usually only occurs between the ages of 15 and 35. It is an autoimmune disease with a family history.
In addition to chronic inflammation, infectious diseases can also be the cause of a toxic megacolon. A relatively common infection that leads to inflammation in the large intestine is an infection with the pathogen Clostridium Difficile, which occurs in the intestines of many people but does not cause any disease under normal conditions. The disease is often triggered by antibiotic therapy, as the normal bacteria in the intestine are attacked and Clostridium Difficile can multiply more strongly. The bacteria produce a poison that causes inflammation in the large intestine.
A very rare cause in Europe is Chagas disease. This is an infectious disease that is transmitted by parasites and is only found in Central and South America. Again, a complication of the infection is inflammation of the bowel.
In addition to those mentioned here, there are a few other causes of a Toxic Megacolon.
Find out more about chronic bowel diseases on our website.
Symptoms of a toxic megacolon
The main symptom with which those affected present themselves in the emergency room are very severe abdominal pain and a defensive tension in the abdominal area, which presents itself to the examiner as a hard stomach.
The pain is accompanied by a high fever and a significantly deteriorated general condition of the person concerned.
Listening to the abdomen reveals a paralyzed obstruction of the bowel known as a paralytic ileus. This means that further transport of the intestinal contents is no longer possible. This build-up of intestinal contents causes, among other things, the severe pain. The high fever also leads to an accelerated pulse and rapid breathing.
The combination of a high pulse and low blood pressure in a high fever is attributed to sepsis, which is better known as blood poisoning.
The damaged intestinal wall also shifts the body's water and salt balance, since the intestinal cells are closely involved in controlling this system under normal conditions. This often leads to water loss and thus dehydration of the patient, which in turn lowers blood pressure.
Furthermore, those affected often show anemia and are also prone to bleeding. The number of white blood cells, the leukocytes, can be significantly increased, which is a typical sign of inflammation.
Overall, the person concerned makes a very sick and weak impression and is in extreme pain.
Therapy of a toxic megacolon
The toxic megacolon is always an acute emergency that requires immediate treatment.
The therapy of the toxic megacolon usually begins with a conservative treatment. The shifted salt and water balance must be corrected. This happens with close-knit intensive medical care using syringe pumps. In addition, in conservative therapy, the toxins that triggered the condition must be removed. It is important to know the cause of the disease.
It has also been shown that it has a positive effect to carry out a leukocyte apheresis. This is a type of blood washing in which the leukocytes, which are excessively increased, are collected from the blood, which can reduce the inflammation.
Antibiotics and antibody therapy can also be administered medically.
If the person's condition does not improve within 48-72 hours, surgery is necessary. The affected section of the intestine is completely removed and an artificial anus is placed.
If the colon has to be completely removed, the artificial anus has to be kept for life. In patients where only part of the large intestine needs to be removed, the artificial anus can be removed after the intestine has healed.
Possible complications of a toxic megacolon
A number of potential complications are known with the Toxic Megacolon.
One possibility is that of a perforated bowel. In this case, the severely damaged intestine breaks open and the intestinal contents enter the abdominal cavity, which can lead to peritonitis.
There is also the risk that those affected will slide into septic shock. This means that the blood pressure continues to drop and the pulse continues to rise until the circulatory system can no longer compensate for this and multiple organ failure occurs.
In addition, it can lead to heavy bleeding, as the blood clotting of those affected is restricted.
When do you need an operation?
The focus of the treatment is the attempt to relieve and maintain the affected section of the intestine. At first, conservative attempts are made under strict intensive medical supervision to balance the water and salt balance and to remove the toxins that cause it.
Only if the conservative therapy shows no success within 48-72 hours does an operation have to be performed.
In some clinics, an earlier operation is now being sought. In the operation, the affected section of the intestine is completely removed and an artificial anus is placed.
Read more about creating an artificial anus here.
Antibiotics
In the best case, the underlying diseases are treated before a toxic megacolon develops. There are antibiotics that work against a Clostridium Difficile infection, for example.
If a toxic megacolon occurs, the person affected receives so-called broad spectrum antibiotics, which help against a large number of bacteria.
Even after the operation, people are given antibiotics to prevent infection.
Read more about the application areas of antibiotics here.
nutrition
During treatment on the toxic megacolon, the affected person is supplied with nutrients via the veins, as the intestine must be completely emptied for the intestine to heal.
After surgical treatment with the creation of an artificial anus, those affected should eat low-fiber foods and eat many small meals
Over time, the intestine can get used to its normal function again. It is particularly important that those affected ensure that they are drinking enough fluids.
Optimal nutrition for colon diseases? - Read more here.
diagnosis
The diagnosis of toxic megacolon is usually made with x-rays of the person's abdomen. Computer tomography can also be used. In both cases, the examining doctor can clearly see the enlarged section of the colon.
A blood count is also routinely done. There is usually anemia and increased inflammation levels. In order to confirm the diagnosis, it is always important to ask the patient whether an inflammatory bowel disease is known or whether there are other risk factors such as antibiotic therapy. In addition, the person concerned usually has a high pulse and low blood pressure.
Duration and prognosis of a toxic megacolon
The toxic megacolon is a very acute disease that develops and worsens quickly. This acute situation must be treated directly, so that the patient can be operated on after 72 hours without improvement.
In this case the acute clinical picture has been resolved, but the duration of the subsequent healing is very different.
The mortality rate is very high even with treatment at around 50%.