Lowering of the uterus
introduction
A lowering of the uterus describes the lowering of the uterus in its holding apparatus. This means that the uterus sinks down and moves into the vagina (Scabbard) can push in. The uterus is not yet visible from the outside. However, it can happen that the uterus sinks so far that the uterus can prolapse, i.e. the uterus may emerge from the vagina (so-called prolapse uteri). The uterus can then even be seen from the outside.
Read more on this topic at: Prolapse of the uterus

causes
The cause of a uterine subsidence can be weak connective tissue. The consequence of this is that the ligament structures with which the uterus is anchored in the pelvis can no longer hold the uterus so tightly in its actual position.
Another cause can be pelvic floor weakness. For example, a weak pelvic floor can occur after pregnancy. If the pelvic floor muscles are not strong enough, this means that the uterus can no longer be held properly and the uterus can sag, sometimes with a simultaneous lowering of the pelvic floor. Obesity (adiposity) can also be the cause of weak pelvic floor muscles and thus lowering of the uterus.
A lowering of the uterus is always associated with the Anteversio and Anteflexio the uterus are lifted. This means that the uterus is now more vertical in the pelvis (Retroversio and Retroflexio).
If the anterior vaginal wall subsides, the posterior bladder wall can also sink (cystocele). If the posterior vaginal wall subsides, the same thing happens with the anterior intestinal wall, i.e. a subsidence of the rectum into the vagina (rectocele).
Uterine sagging during pregnancy
Pregnancy means that the uterus is exposed to special conditions. The normally quite small organ grows to a much larger extent and is significantly stressed. Because the unborn child and the uterus are much heavier, this weight then also weighs on the pelvic floor. This can lead to increased stress on the muscles and ligaments of the pelvic floor during pregnancy and develop a certain degree of weakness.
A slight lowering of the uterus during pregnancy does not mean the highest level of alarm. Of course, it becomes more critical when the uterine subsidence reaches or exceeds a certain level. If this happens, so-called pessaries can be inserted. In this case, a pessary would be a hard plastic piece in the form of a ring, which is inserted by the gynecologist and supports the posture of the uterus and cervix. However, such a pessary should be checked and changed regularly to ensure that it is correctly fitted and to prevent infections.
Uterus subsidence after childbirth
One risk factor for uterine subsidence is natural birth. Since the ligamentous apparatus and the muscles of the pelvis are particularly stressed during a natural delivery, the pelvic floor may become weak afterwards.Especially if there are additional birth injuries, this increases the risk of weakness of the muscles and ligaments. The weakness of the pelvic floor can in turn lead to a lowering of the uterus.
There are many ways to treat pelvic floor problems after birth.
Read more about this under: Pelvic floor training
With every further pregnancy or vaginal birth, the risk of pelvic floor weakness and thus of uterine subsidence increases. Another stress factor in a natural birth is a prolonged expulsion period or the use of forceps.
As a general rule, however, the uterus does not sag immediately after every natural birth. As a preventive measure, it is important to avoid heavy physical labor during the puerperium. This would further affect the muscles that are weakened after the birth and promote the development of a uterine subsidence. In the same way, certain postnatal exercises are recommended in order to strengthen the stressed muscles again and to counteract a weakness of the pelvic floor.
Read more about this under: Uterus subsidence after birth
Lowering of the uterus after a caesarean section
A caesarean section alone is not a risk factor for a uterine subsidence. In a caesarean section, the uterus is opened through an incision in the lower part of the abdomen and the child is born. This means that the pelvic tissue and the pelvic floor muscles do not have to expand, as would be the case with a natural birth, because the uterus is opened above these structures. It is precisely this excessive stretching that causes the uterus to sag later, which is why there is not necessarily a higher risk of sagging after a caesarean section. However, every pregnancy is a risk factor for uterine subsidence later in life.
Uterus subsidence during menopause
Age is a major risk factor for the development of uterine subsidence. Especially during the menopause and afterwards, the tissue of the holding apparatus in the pelvis loses more and more of its elasticity and only enables the uterus to sink. In addition, the blood supply to the muscles of the pelvic floor is weaker, which means that the muscles lose strength.
These changes are partly triggered by the fact that the body changes its hormonal balance during the menopause. Local therapy with the hormone estrogen can therefore effectively counteract uterine subsidence during menopause. The hormone is either brought into close proximity to the uterus in the form of creams or suppositories, or a vaginal ring can be inserted to secrete the hormone.
Read more on this topic at: Menopause symptoms
What influence does a womb subsidence have on sexuality?
Depending on the severity, a lowering of the uterus can cause pain during intercourse. Because the uterus is lower than normal, it can be an obstacle to sexual intercourse. Especially when the uterus is already emerging from the vaginal outlet, this is not only a cosmetic problem, but also has a negative impact on a woman's sexuality. In addition, it must be noted that an exposed uterus is very susceptible to damage, as the sensitive mucous membrane dries out in the air. Mechanical effects on the vagina or uterus can therefore be damaging to the organs. A lowering of the uterus can also trigger feelings of shame in women, especially if incontinence occurs as part of an additional bladder lowering. These feelings of shame continue to have a negative effect on sexuality.
therapy
A distinction is made between conservative and surgical therapy in terms of therapy options.
First of all, pelvic floor exercises fall under conservative therapy. This is recommended to stabilize the pelvic floor. The pelvic floor training must be carried out constantly and lifelong, as these muscles can easily regress again. A conservative therapy with estrogen preparations can also be tried. These are applied locally as suppositories or ointments. Furthermore, of course, risk factors such as obesity must be reduced.
Read more on this topic at: Pelvic floor training
Another therapy option for a uterine subsidence is the use of a pessary. A pessary is ring-shaped or cube-shaped and is inserted into the vagina. Here it is held by the pelvic floor and supports the uterus from the inside. Pessaries must be adapted and used by the gynecologist. Pessaries must also be cleaned regularly.
If the conservative therapy options are no longer sufficient or if there is already a prolapse of the uterus, surgery can be used. On the one hand, a vaginal plasty (Colporrhapy) can be made. With this, vaginal tissue and ligaments are gathered and fixed. If there is a relevant uterine prolapse, it may be necessary to completely remove the uterus.
Read more on this topic at: vaginal hysterectomy
After the uterus has been removed, pregnancy is no longer possible, so it should be considered whether the patient still wants to have children. Sexual intercourse is still possible after just having the uterus removed. During all operations, care is taken to ensure that organs involved, such as the urinary bladder and rectum, are returned to their original location. Pelvic floor exercises are recommended after an operation. This prevents organs from sinking again. Lifting heavy loads (> 5 kg) should also be avoided.
Surgery for a uterine sagging
Whether an operation is necessary for a uterine subsidence depends on various criteria.
On the one hand, of course, there is the question of what kind of uterine subsidence is present, i.e. how strong it is and what the symptoms are. Then it is important how much the patient is suffering. Age and health also play a role. Furthermore, it should of course be noted whether there is still a current desire to have children.
The so-called vaginal hysterectomy is the most common operation that is performed when the uterus is lowered. This means removing the uterus through the vagina. In comparison to abdominal hysterectomy, no incision on the abdomen and therefore no large surgical scar is necessary.
Read more on this topic at: Hysterectomy
During the operation, the uterus is completely removed and at the same time the urinary bladder is lifted and fixed a little again, so that the symptoms of bladder weakness and the feeling of pressure of the bladder on or out of the vagina are reduced (anterior vaginal plasty). The perineum area (between the vagina and anus) is also strengthened. This is done by uniting your own musculature and, if necessary, a plastic mesh can be inserted (posterior vaginal plasty).
If bladder weakness has occurred at the same time as the uterus subsidence, this can also be corrected during the operation. A TVT (tension-free vaginal tape) is performed here. A plastic tape is draped around the urethra in such a way that there is no more involuntary urination and that normal urination is possible.
The risk with such an operation is that the operation can lead to bladder weakness (stress incontinence). Relapses can also occur, so that uterine subsidence can occur again. In general, however, the operation is carried out in such a way that relapses (recurrences) should be as good as impossible.
For more information, see: Operation of a lowering of the uterus
Exercises
As a preventive measure, structured pelvic floor training has a positive effect on the supporting tissue of the pelvis. Once the uterus has subsided, it cannot be reversed with the help of exercises, but further subsidence can possibly be prevented. In practice, this means that women who have risk factors for uterine subsidence should do regular pelvic floor exercises.
There are many specific exercises you can do to strengthen your pelvic floor. In addition, every other form of sport, such as fitness classes or jogging, also strengthens the pelvic floor muscles and is also recommended. Also because a body weight in the normal range is good for the progression of the uterine sagging. In addition, exercises for the pelvic floor have a positive influence on incontinence. Studies have shown that women who exercise their pelvic floor suffer from incontinence less often.
Read more on this topic at: Pelvic floor training
diagnosis
First of all, an anamnesis, i.e. a systematic questioning of the patient, is carried out. The doctor asks about complaints or symptoms as well as possible risks for weak pelvic floor muscles, such as Births and their number.
Next, a physical exam will be performed on the patient. During a palpation examination, the doctor can assess the strength of the pelvic floor or get an idea of any bulges in the vagina.
During a speculum exam, the doctor inserts an examination instrument into the vagina. This gives him a better view of the vagina and, among other things, can assess the cervix and cervix. Normally you can see the portio, the transition from the cervix to the vagina, slightly protruding into the vagina. If a uterine subsidence is suspected, the patient is allowed to press briefly during this examination. If the uterus has subsided, the cervix moves visibly further downwards while pressing. A speculum examination can also show protrusions of the vagina wall, which suggest a cystocele or rectocele.
If the urinary bladder is involved in the course of a uterine lowering and the resulting incontinence problems are involved, further examinations can be made in this regard.
How can you feel a uterine subsidence?
In many cases, a uterine subsidence can be felt by the gynecologist using a routine palpation examination. The palpation examination does not initially differ from that carried out during the annual cancer screening. If the suspicion of uterine subsidence is confirmed, the gynecologist will carry out a more detailed examination to determine how far the uterus has already sunk. The cervix is used as a guide. It represents the lowest part of the uterus. The height of the cervix provides information about the severity of the depression.
The cervix is felt as a ring-shaped, coarse structure in the vaginal canal. Usually it is just above the vagina. Severe uterine subsidence can usually be felt more easily than those that are still in an early stage. An ultrasound examination can provide further information here. However, the cervix extends far into the vagina even with a grade 1 uterine sagging, so that a palpation examination is often sufficient to confirm the suspicion.
During the palpation examination, the gynecologist asks the patient to perform various maneuvers such as coughing and pressing. This increases the pressure in the abdomen and can affect the extent of the depression or unmask it in the first place. In the case of advanced subsidence, these can also be felt by the patient himself. If the uterus already protrudes above the level of the vaginal outlet, parts of the uterus located further up can also be felt in addition to the cervix.
Would you like to learn more about this topic? You can find detailed information on this at: How can you feel a uterine subsidence?
Symptoms
Various symptoms are described when the uterus has subsided. There is a feeling of pressure or a foreign body in the vagina. The patients report the feeling that something is falling out of the vagina. This is because the uterus pushes into the vagina, creating the sensation.
Some patients also report pain in the lower back, i.e. in the lower back. The fact that the uterus is attached to the holding apparatus in the pelvis and the uterus now pulls the uterus downwards by these ligaments due to the uterus subsidence results in a feeling of pain. That this is mainly registered in the lower back is due to the fact that the ligaments in the pelvis are tight on the back.
Furthermore, it can lead to bladder problems, especially bladder weakness. This includes stress incontinence, pollakiuria and possibly also recurrent urinary tract infections.
Stress incontinence means that the urine can no longer be held correctly when the pressure increases, such as when coughing, laughing or sneezing or even in more severe cases when climbing stairs or standing up and urine is involuntarily released.
Pollakiuria is the frequent emptying of the bladder, whereby only small amounts are given off at a time.
Urinary tract infections occur because the anatomically incorrect structure of the urinary tract and vagina means that germs can more easily ascend into the body.
It can also lead to urination problems. These are due to the fact that the uterine subsidence has progressed so far that it squeezes the urethra. This means that it is difficult to empty the bladder, which can lead to urinary retention.
If a rectocele occurs as part of the lowering of the uterus, i.e. the bowel protrudes into the vagina, symptoms can also occur during bowel movements. This includes, for example, difficult defecation or constipation.
Read more on the subject at: What are the symptoms of uterine subsidence?
Pain
Pain occurs mainly in the back and pelvic area. They are triggered by pulling on the support structures or by changing your posture. Therefore, they are typically also described as pulling.
Uterine sagging and back pain
A common accompanying symptom of uterine subsidence is back pain. These are mainly located in the area of the sacrum and coccyx. Classically, the pain is described as pulling. The pain is caused by the fact that the sunken uterus is still connected to the holding apparatus in the pelvis and exerts a pull on it. In the case of more advanced uterine subsidence, the posture and gait of those affected can also change. These changes are related to the foreign body sensation that women feel and the feeling that something could fall out of the vagina at any moment. These changed postures can also trigger back pain.
Can a lowering of the uterus also cause bowel problems?
A lowering of the uterus can also cause discomfort in the intestines, especially in the area of the rectum. This lies directly against the back wall of the vagina. A lowering can trigger intestinal problems in the form of constipation and discomfort when defecating. On the other hand, fecal incontinence can also be the result of a uterine sagging.
forecast
All surgical methods have one Success rate from 90 – 95 %.
What can the long-term consequences be?
The long-term consequence of untreated uterine subsidence is the uterus sinking further and further until the uterus prolapses. Since the urinary bladder and rectum are in close proximity to the uterus, these organs can also sink and cause symptoms of incontinence or difficult stool or urination. Before the lowering of the uterus progresses so far that an incident occurs, specific therapeutic measures can be used to intervene.
However, long-term consequences can arise, especially with surgical therapy. The operation to lower the uterus does not cure the underlying disease, namely the weakness of the pelvic tissue and the pelvic floor muscles. It only treats the symptoms. It follows that, even after an operation, the uterus may come down again and this is not uncommon. Although the renewed decrease can also be treated surgically, it cannot be ruled out that decreases can occur again and again in the course of life.Furthermore, the operation can pull the bladder up too far, which can lead to incontinence. Incontinence can also be treated in many ways, but it cannot be ruled out that it will persist as a long-term consequence.
Is it allowed to jog with a lowered uterus?
Whether you are allowed to jog with a lowering of the uterus should always be discussed individually with your gynecologist. Jogging can put increased pressure on the pelvic organs and this can trigger pain or even incontinence. Nevertheless, there is no general ban on jogging for women whose uterine subsidence was caused by multiple births or a congenital weakness of the tissue. According to the current state of science, it has also not been proven that jogging could trigger a lowering of the uterus. Only women who have just given birth should not go jogging again immediately, as the pelvic floor muscles and pelvic tissue are still loosened during childbirth and have to regress again.
prophylaxis
A stable pelvic floor is the prophylaxis for a uterine subsidence. This can be strengthened by training the pelvic floor. Timely weight reduction can also be beneficial in the case of obesity.
Lowering of the uterus and urination
Since the bladder is in direct contact with the uterus and the anterior vaginal wall, in some cases, when the uterus subsides, it also subsides. The cause of the lowering of the bladder lies in the weakness of the anterior vaginal vault. If the stability of this vault is no longer guaranteed, the urinary bladder sags in the direction of the vagina and sinks from its original position. The symptoms that result from a lowering of the bladder are, on the one hand, difficult emptying of the urinary bladder, which can lead to frequent urinary tract infections. On the other hand, incontinence can also develop.
Frequency distribution
The frequency of uterine prolapse increases with age. One estimate is that around 12% of 80-year-old women have a finding that requires surgery.
Degree of uterine subsidence
There are four grades. In grade 1, the cervix reaches a maximum of one centimeter from the vaginal opening. The uterus is still completely in the vagina. A grade 2 is awarded if the cervix has sunk to the level of the vaginal opening. If it is lowered further to a maximum of two centimeters below the level of the vaginal opening, then it is grade 3. Finally, grade 4 represents the prolapse of the uterus, in which the cervix rises above the vaginal level by more than two centimeters.
Anatomy of the uterus
Various anatomical structures ensure that both the uterus and vagina are anchored in their place in the body. These include, on the one hand, the holding apparatus of the uterus, which is mainly from the Ligamentum latum uteri and Sacrouterine ligament is formed. These ligaments hold the uterus in place in the pelvis.
Furthermore, the pelvic floor prevents the uterus from sinking downwards. The pelvic floor consists of three levels: the Pelvic diaphragm, the Urogenital diaphragm and the outer Sphincters.
In addition, the uterus is usually tilted 90 ° towards the abdomen against the axis of the vagina (so-called Anteversio) and the body of the uterus is also tilted towards the abdomen by 135 ° in relation to the cervix (Anteflexio). Thus, the uterus normally rests on the urinary bladder.
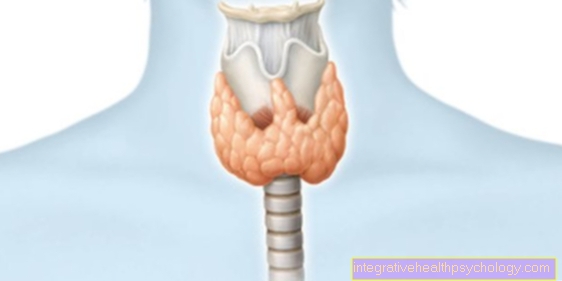
Illustration of the uterus
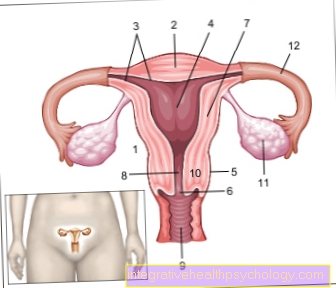
- Uterus -
uterus - Uterine tip -
Fundus uteri - Uterine lining -
Tunica mucosa - Uterine cavity -
Cavitas uteri - Peritoneum cover -
Tunica serosa - Cervix -
Ostium uteri - Uterine body -
Corpus uteri - Uterine constriction -
Isthmus uteri - Sheath - vagina
- Cervix - Cervix uteri
- Ovary - Ovary
- Fallopian tubes - Tuba uterina
You can find an overview of all Dr-Gumpert images at: medical illustrations