arthritis
General
synonym: Joint inflammation
English: arthritis
Arthritis is an inflammation of the joints that can occur in connection with various diseases.
A distinction is therefore made between different forms of arthritis, see causes.
Arthritis manifests itself through the typical symptoms of inflammation: the joint is reddened, swollen, overheated and painful.
If only a single joint is affected, it is called monoarthritis.
Involvement of multiple joints, on the other hand, is called oligoarthritis.
The term polyarthritis is used when a large number of joints are affected.
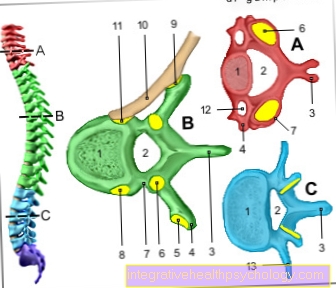
Arthritis in the spine is known as spondyloarthritis.
A differentiation from arthritis is osteoarthritis, in which the joint is initially not damaged by inflammation but by wear and tear. However, in advanced stages, osteoarthritis can lead to arthritis.

causes
The two most common causes of arthritis are infections and autoimmune diseases. There are also the so-called crystal arthropathies, in which crystal deposits in the joint cause inflammation, as well as rarer special forms of arthritis.
Infectious or septic arthritis is most often caused by bacteria. However, infection of the joint with viruses or fungi can also lead to arthritis.
The pathogens can get into the joint in the following ways:
-
via the blood (haematogenous spread), for example in the case of blood poisoning (sepsis)
-
by opening the joint space, either in the event of injuries or in the case of non-sterile medical interventions (punctures, operations)
-
through spread of a neighboring infection of the soft tissues (for example after hip replacement) or of the bone (osteomyelitis)
In addition, arthritis can occur as a symptom of a Lyme borreliosis infection after a tick bite (Lyme arthritis).
A large subgroup of arthritis occurs in the context of autoimmune diseases.
These are characterized by the fact that the immune system is directed against its own body. If parts of the joint such as the joint cartilage or the synovial membrane are attacked, arthritis can develop. The most common form of such autoimmune joint inflammation is rheumatoid arthritis, popularly known as rheumatism.
The following autoimmune diseases can also involve joint involvement:
-
Psoriasis
-
Systemic lupus erythematosus
-
Sjogren's syndrome
-
Scleroderma
-
Dermatomyositis
-
Bechterew's disease (ankylosing spondylitis)
-
Chronic inflammatory bowel disease (Crohn's disease, ulcerative colitis, Whipple's disease)
-
Sarcoid
-
Inflammation of the blood vessels (vasculitis) such as Wegener's disease
A special form of immune-related arthritis is what is known as reactive arthritis. Arthritis occurs after a bacterial infection of the gastrointestinal tract, the urinary tract, the genital organs or the respiratory tract, although the mechanism by which it develops has not yet been finally clarified. One suspicion is that the bacteria have components on their surface that resemble the body's own molecules from cells in the joint.
After successfully fighting the bacteria, the immune system may also recognize these molecules as foreign and therefore trigger an immune reaction against the body's own cells. This type of “mix-up” is also known as cross-reactivity.
Another theory says that components of the pathogen remain behind after the infection has been overcome, are deposited in the joint and thus reactivate the immune system. If, in addition to reactive arthritis, an inflammation of the urethra and conjunctivitis is also a secondary disease after an infection, it is called Reiter's syndrome or Reiter's triad.
Another cause of arthritis are the so-called crystal arthropathies. The deposits of crystals in the joint cause an inflammatory reaction.
The best-known form of crystal arthropathy occurs in the context of gout, in which uric acid crystals form (arthritis urica). Arthritis is more rarely caused by calcium pyrophosphate crystals, which are deposited in the cartilage in pseudogout (chondrocalcinosis), or by apatite crystals, which are formed in hydroxyapatite disease.
In addition, arthritis can be caused as a result of joint wear and tear in osteoarthritis, as well as joint bleeding in hemophilia.
Appointment with ?

I would be happy to advise you!
Who am I?
My name is dr. Nicolas Gumpert. I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
In order to be able to treat successfully in orthopedics, a thorough examination, diagnosis and a medical history are required.
In our very economic world in particular, there is too little time to thoroughly grasp the complex diseases of orthopedics and thus initiate targeted treatment.
I don't want to join the ranks of "quick knife pullers".
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You will find me:
- Lumedis - orthopedic surgeons
Kaiserstrasse 14
60311 Frankfurt am Main
You can make an appointment here.
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
For more information about myself, see Lumedis - Orthopedists.
Symptoms
All forms of arthritis manifest themselves through the typical signs of inflammation: The affected joints are reddened, overheated, swollen and painful. This usually results in a restriction of mobility. Especially with the rheumatoid arthritis the pain and immobility are usually strongest in the morning and after long periods of rest and improve with movement. This so-called Morning stiffness also occurs in osteoarthritis, but it is in the rheumatoid arthritis more pronounced and can last up to several hours.
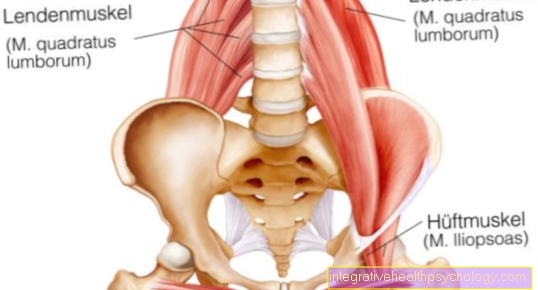
The pattern of joint involvement varies with the different forms of arthritis: This is how it begins Rheumatoid arthritis usually on the little finger and toe joints on both halves of the body and only later changes to larger joints such as the shoulder joint. That is why it is also called chronic polyarthritis. In contrast, the reactive arthritis preferably on the larger joints of the lower half of the body (hip, knee, ankle), whereas on the gout usually only one joint is affected at first - particularly often the base joint of the big toe. During the ankylosing spondylitis is primarily an inflammatory disease of the spinal joints and the symptoms therefore tend to occur in the back area, psoriatic arthritis can manifest itself through different patterns of involvement.
In addition, various accompanying symptoms can occur in the individual subclasses of arthritis, which are often characteristic of the underlying diseases that have already been listed under causes:
infectious arthritis: fever, occasionally skin rash
Rheumatoid arthritis: Rheumatoid nodules (small, not painful, movable nodules in the subcutaneous fatty tissue)
Psoriatic arthritis: scaly rash, itching, nail changes
Systemic lupus erythematosus: butterfly-shaped rash on the face
Sjogren's syndrome: Dry eyes, dryness of the mucous membranes
Scleroderma: Hardening and thinning of the skin
Dermatomyositis: Rash, muscle weakness, muscle pain
ankylosing spondylitis: Inflammation of the tendons, Inflammation of the eyes (Uveitis), pronounced forward curvature of the spine
Inflammatory bowel disease: diarrhea, stomach pain, nausea, Vomit, Loss of appetite, fever
Sarcoid: Fever, to cough, Shortness of breath
Vascular inflammation: Fever, fatigue, night sweats, muscle pain
Reactive arthritis: Urethritis, Conjunctivitis
- gout: Gouty tophi (nodular swellings near the joints), inflammation of the kidneys
diagnosis
In order to correctly diagnose arthritis, careful questioning of the patient (medical history) is essential. The doctor asks for information about the type and severity of the symptoms, possible infections or injuries as the cause as well as previous illnesses and accompanying symptoms. This is followed by a physical examination to determine the extent of the inflammation and the restricted mobility of the affected joints as well as a possible joint effusion.
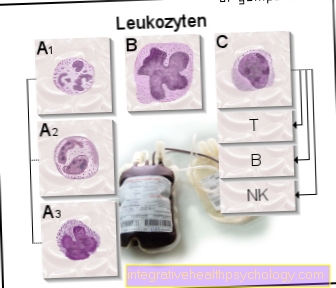
Another important part of diagnostics is the laboratory examination of the blood. All forms of arthritis are usually expressed as an increase in inflammation levels such as C-reactive protein (CRP), the erythrocyte sedimentation rate (ESR) and an increase in white blood cells (leukocytes).
The blood test can also provide clues about the cause of the arthritis:
If pathogens are detected in the blood by means of a blood culture, it is probably a question of septic arthritis, whereas in the case of reactive arthritis, antibodies against the pathogens that have already been combated are sought.
Arthritis caused by gout usually shows up in blood tests as increased uric acid levels.
In rheumatoid arthritis, the so-called rheumatoid factor - a defense substance produced by the body against the body's own antibodies - is typically present in the blood. However, since it can also occur in other autoimmune diseases such as systemic lupus erythematosus, the blood is usually also tested for so-called CCP antibodies, the presence of which is almost certain to prove rheumatoid arthritis.
However, if these markers in the blood are negative, this does not rule out the presence of arthritis.
If an effusion has formed in the inflamed joint, the joint can be punctured as part of the diagnosis.
This is particularly useful if you suspect infectious arthritis, as in this case the type of pathogen can be identified from the synovial fluid.
In addition, the number of white blood cells in the synovial fluid is usually increased.
If, on the other hand, crystals can be detected during joint puncture, there is a high probability that crystal arthropathy is present.
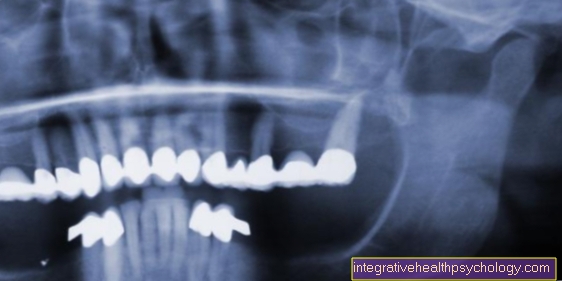
X-rays are the primary imaging method used to diagnose arthritis. Characteristic changes can usually be seen on the X-ray, which confirms the diagnosis of arthritis. In addition, the stage of the disease can be determined and any existing consequential damage to the joints can be determined.
X-rays are also indispensable for planning an operation and for monitoring the progress of therapy.
The MRI shows signs of arthritis in the very early stages, but due to the high cost and technical complexity it is used rarely and only when the diagnosis is unclear.
Please also read: MRI procedure, clothing in the MRI - what should I wear?
Computed tomography (CT) is particularly important in diagnosing arthritis of the cervical spine.
therapy
Once the diagnosis is made, treatment for arthritis should begin as soon as possible to prevent or at least delay damage to the joints.
The therapy initially depends on the underlying disease.
In infection-related arthritis, for example, the infection is fought with antibiotics or antiviral drugs or fungal drugs, depending on the pathogen.
Arthritis caused by gout can be treated by taking uric acid lowering drugs, such as allopurinol.
In autoimmune arthritis diseases, therapy is based on suppressing the immune reaction (immunosuppressants). As a rule, cortisone or drugs similar to cortisone (glucocorticoids) are used first.
If a single joint is severely inflamed, cortisone can also be injected directly into the joint.
This has the advantage that fewer side effects occur in the entire organism, since the drug only works locally in the joint.
If autoimmune diseases are severe, stronger immunosuppressive drugs such as leflunomide or methotrexate are used. The latter is used in high doses as chemotherapy for cancer diseases, but the usual dose for the treatment of arthritis is much lower and therefore has fewer side effects.
In the long-term treatment of rheumatoid arthritis, these drugs are grouped under the name of basic therapeutic agents or DMARDs - disease-modifying antirheumatic drugs - because they specifically intervene in the course of the disease. They prevent the progression of the disease and can avoid long-term consequences if therapy is started in good time. However, it can take up to several months for the effects to occur.In the initial phase, therefore, cortisone is also given, whereby the dose can often be reduced after the DMARDs take effect.
A new group of DMARDs are the so-called biologics. These are genetically engineered proteins that act against certain inflammatory substances or inflammatory immune cells. They often work faster than conventional DMARDs and are often used in patients who have not had any other therapy.
For pain in all forms of arthritis, anti-inflammatory pain relievers (NSAIDs, non-steroidal anti-inflammatory drugs) such as diclofenac can be taken as needed.
Physiotherapy and physical treatments such as cold therapy or electrotherapy can help reduce symptoms and improve mobility.
Long-term consequences and prognosis
While in the past patients with arthritis were often recognizable by their severely deformed hands, nowadays early treatment can prevent such long-term effects in many cases.
If left untreated, arthritis leads to the destruction of cartilage and bones due to the chronic inflammation of the synovial membrane.
This limits or completely prevents mobility.
In the long term, the joint loses its function and stiffens. Since tendons and surrounding soft tissue can also be attacked, deformations and misalignments can occur.
If arthritis is diagnosed in good time and treated accordingly, the disease can usually be controlled well today. Nevertheless, patients should take advantage of support in the form of training courses, self-help groups or occupational therapy in order to better cope with everyday life with the disease.
Read more about this at: Course of osteoarthritis