Peritonitis
introduction
Peritonitis (Peritonitis) is an inflammation of the peritoneum (peritoneum), which can occur locally or generalized throughout the peritoneum. Depending on the cause of the inflammation, a distinction is made between primary and secondary peritonitis. If therapy is inadequate or too late, it can be fatal.
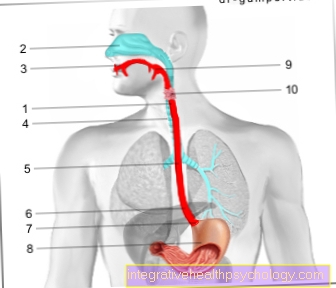
Information on anatomy can be found here: peritoneum, abdomen

Symptoms
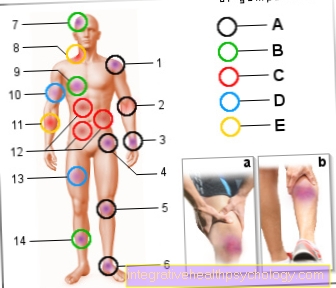
Local inflammation of the peritoneum causes severe localized abdominal pain, such as appendicitis. Often there is strong local pressure pain, possibly also a pain to let go and a tension in the immune system in the area of the inflammation. Pain by tensing the thigh and lifting the thigh against a force can cause pain in the area of inflammation. This is called Psoas pain designated. The general condition is often not impaired and the pain can cease at rest.
Generalized peritonitis, on the other hand, makes the patient look seriously ill. It can be seen at first glance that the patient has a life-threatening illness.
The face is often very sunken and gray, and breathing accelerates.
The patients suffer from severe abdominal pain in the entire abdominal cavity with increasing immune tension. The abdominal muscles harden so that the stomach becomes as hard as a board. The entire symptomatology of acute generalized peritonitis is referred to as acute abdomen and is usually associated with an intestinal obstruction.
This is caused by inflammation and is therefore called a paralysis-related intestinal obstruction (paralytic ileus) designated.
Intestinal noises are then no longer audible.
Read more on the subject at: These are the signs of a bowel obstruction
Furthermore, generalized peritonitis is usually caused by symptoms such as nausea, vomiting, constipation (Constipation) and fever.
If the treatment is not sufficiently rapid, the symptoms can range up to shock symptoms with low blood pressure, palpitations (Tachycardia) or massive slowing of the heartbeat (Bradycardia), Clouding of consciousness and death.
Diagnosis is more difficult in older patients with atrophic abdominal muscles. Here the typical symptoms of the acute abdomen are not always present.
If the peritoneal dialysis is the cause of the inflammation, the first thing that is noticeable is the changed dialysate, which is clouded due to numerous inflammatory cells.
root cause
The most common cause of peritonitis is appendicitis (appendicitis).
This releases germs such as Escherichis coli, enterococci and, rarely, salmonella, staphylococci or streptococci.
If appendicitis is detected in good time and operated on, the peritoneum is only locally inflamed. For a ruptured appendix (Appendix perforation) or a perforation of other organs in the abdomen results in an acute and life-threatening generalized peritonitis very quickly. In addition, acute biliary inflammation is a common cause of peritonitis in the right upper abdomen.
Read more about this under Ruptured appendix
Due to the eradication of Helicobacter pylori carried out today, perforation of a duodenal ulcer has become very rare. Inflammation in the left descending part of the colon (Diverticulitis) can also lead to local or generalized peritonitis in the left lower abdomen.
Inflammation of the female internal sexual organs also leads to peritonitis.
Another form is wandering peritonitis.
This can occur due to an untreated intestinal obstruction and an escape of germs through the damaged thin wall of the intestine.
Peritonitis can also be a complication of medical treatment.
The most important cause is peritoneal dialysis in the case of long-term treatment. The reason is that germs migrate through the open abdominal wall during non-sterile work.
A rarer cause is that Carcinomatous peritonitis.
This is a pronounced tumor infestation of the peritoneum.
This leads to a non-bacterial inflammatory reaction, which often results in pronounced dropsy (Ascites) in the abdomen.
Even if the liver ruptures as part of trauma, peritonitis is a dreaded complication.
In rare cases, "Still's disease", a rheumatic disease, can also be the cause. For the most important information, read the article under: Still's disease - what's behind it?
Peritonitis after surgery
The causes of the emergence of a Peritonitis (Peritonitis) are very numerous.
If the peritonitis is triggered by a previous operation, it is called a postoperative peritonitis. There are many reasons for this.
- For one thing, it can get through lack of sterility During the operation, germs can spread into the operating area, which then trigger an inflammation there and thus lead to peritonitis.
- Often the peritonitis also results from a Suturewhich opens again so that secretions from the "leaking“Organ like that pancreas (pancreas), of the Gallbladder and the Intestines, leak and lead to strong inflammatory reactions. This progresses particularly quickly in the context of a gallbladder infection that is currently taking place, for example, whenleaking“Organ inflammation is taking place. However, simultaneous inflammation is not a prerequisite for peritonitis. The leakage of body fluids alone is sufficient, because gastric juice, bile and pancreatic secretions take effect, among other things because of their aggressive nature pH values the peritoneum and thus trigger chemical peritonitis. This is particularly dangerous if large amounts of intestinal contents get into the abdominal cavity.
The general rule is that no matter what the cause, a Peritonitis is always life-threatening. The increased life-threatening potency is due to the fact that the Intestinal contents very rich in bacteria is (especially rich in Enterococci and E. coli bacteria (Escherichia coli)). Peritonitis triggered by intestinal contents can for example be part of a Ruptured appendix arise or through a Colonoscopy triggered if there is a perforation (breakthrough) of the intestine. If an operation cuts off the blood supply to the intestinal loops (Intestinal artery obstruction) or if through surgery Intestinal obstruction (Ileus) is provoked, this part of the intestine dies at some point and the intestinal wall becomes permeable for bacteria, which can then pass into the abdominal cavity.
This process is known as migration peritonitis.
Diagnosis of peritonitis
In terms of laboratory chemistry, significantly increased inflammation parameters are initially noticeable in peritonitis.
These include CRP and a clearly too high leukocyte count in the blood count. In addition, the sedimentation rate (ESR) is greatly accelerated due to the high number of cells.
In the further course of the inflammation, changes in the coagulation parameters (Quick, PTT and drop in platelet count) appear as a sign of significantly increased consumption (Consumption Coagluopathy).
Changes in kidney values with rising creatinine and urea as well as rising transaminases and falling cholinesterase as signs of liver failure and a drop in hemoglobin are the first signs of multi-organ failure.
Read more about the topic here: Cholinesterase deficiency
In the ultrasound (Sonography) of the abdomen, free fluid and free air are recognizable as a sign of organ perforation. In addition, a significantly reduced movement of the bowel is visible as a sign of an intestinal obstruction.
In many cases it is possible to find the cause with the help of ultrasound, such as an organ rupture or an organ inflammation.
With a simple x-ray without contrast agent while standing and lying on one side, fluid levels in the intestine and free air under the diaphragmatic crowns are often visible.
The above diagnostic signs of peritonitis relate to generalized peritonitis.
In the case of local inflammation of the peritoneum, the inflammation values are often only slightly increased. Some free fluid in the area of inflammation may be visible on ultrasound as a sign of inflammation-related edema. Free air only occurs in the context of a hollow organ perforation.
Therapy peritonitis
The treatment of acute local inflammation of the peritoneum is always surgical. The attempt is made surgery to be carried out as early as possible to avoid serious complications and generalized peritonitis.
The basic principles of therapy for peritonitis are the Removal of the focus of inflammation, so a definitive operative therapy for the underlying disease.
That means, depending on the cause, the appendix, gall bladder or parts of the intestine are removed.
Existing Ulceration are sewn over and thus firmly closed. If parts of the intestine have to be removed, a artificial anus (Enterostomy) because anastomoses of intestinal sections often do not hold in inflammatory tissue.
The relocation and final anastomotic closure of the intestinal parts takes place after a few weeks and the inflammation has subsided.
In addition, rehabilitation and removal of all necroses, pus and fibrin coatings. These represent an ideal breeding ground for bacteria and germs and must therefore be removed thoroughly.
Often with generalized peritonitis, purulent ascites is found throughout the abdominal cavity. In order to completely rid the abdominal cavity of pus residues, the abdomen is thoroughly rinsed with saline or Ringer's solution.
A drainage system is then always applied to drain away the accumulating secretions. Since generalized peritonitis is a life-threatening septic clinical picture with possibly existing organ failure, follow-up treatment always takes place first in the intensive care unit.
Many patients have to continue to be ventilated during this time, as the circulatory situation can be critical.
This also facilitates adequate pain medication, as most highly potent pain medication such as morphine dampen the respiratory drive. Broad-spectrum antibiotics are also administered to combat blood poisoning. Fluid and organ-supporting drugs are given intravenously depending on the individual situation.
forecast
Depending on the severity of the peritonitis, the time of the corresponding therapy and the general condition of the patient, the mortality rate of pronounced peritonitis is 50%.
Duration of peritonitis
The Duration of peritonitis depends on its course.
It can be a localized infection or an inflammation that has spread through the bloodstream over the whole body and thus a Blood poisoning (sepsis) was created. The duration of the disease also depends on its cause and treatment.
In very few cases a targeted one is sufficient Antibiotic therapy which is then administered over at least five to seven days.
In 99% of cases, surgery must be taken against peritonitis. The surgical treatment also entails a subsequent antibiotic treatment. Due to the individual course and the various factors such as cause, condition and age of the patient, no general duration can be predicted.
Is Peritonitis Contagious?
As already described, the most common cause for peritonitis one previous appendicitisthat has not been treated properly or quickly enough. This made the appendix brittle, which allowed germs and inflammation-promoting substances to enter the abdominal cavity. This However, germs areas long as they are located in the intestine for the people not harmful. Some of them are even useful and support our digestion. Even with other causes of peritonitis, such as inflamed protuberances of the large intestine (diverticulitis) or inflammation due to a previous, untreated intestinal obstruction, germs can escape from the intestine. The processes that ultimately lead to inflammation of the peritoneum play out within the patient's body from.
For outsiders and supervisors no risk of infection through excretions of the sick person or the air. As already said, peritonitis is often triggered by germs that a healthy person would excrete in the stool.
Malignant germs are sometimes also responsible for the development of peritonitis. However, these germs are only able to trigger such an inflammation if they get directly into the abdominal cavity of a person via the brittle intestine or other non-intact abdominal organs. Infection with these germs can occur through contaminated food and could cause gastrointestinal illness in healthy people with intact internal organs, which would manifest itself in diarrhea and vomiting, for example. There is therefore no risk of contracting peritonitis if you have come into contact with a person who is sick with this person.
A Special form of peritonitis is the so-called Feline infectious peritonitisthat through a virus is triggered, but almost mainly in cats occurs. The Excretions from an infected cat are contagious, so infectious for other cats, which can then also get sick. For the people is the virus responsible harmless, it thus exists no risk of infection in contact with an infected cat.
Peritonitis children

In children, the disease peritonitis, or "peritonitis", plays a major role in that the Appendicitis peakwhich is an important cause of the development of peritonitis, in school age lies.
There is also a very rare form of peritonitiswhich accounts for only 1% of all peritonitis and especially children and people with an already weakened immune system concerns, namely the so-called "Primary peritonitis“.
This is the form of peritonitis not triggered by bacteriawho have broken and inflamed abdominal organs, like stomach, Intestines or appendix found their way into the abdominal cavity.
The cause of the "primary peritonitis" are rather Bacteria that reach the peritoneum directly through the bloodstreamthat is well supplied with blood or those that rise from an infection of the pelvic organs into the abdomen. Once there, the bacteria are able to settle and cause the inflammation.
While in the more common form of peritonitis the bacteria Escherichia coli and enterococci are important pathogens that trigger inflammation, in the rare form described above, streptococci and pneumococci are found as triggers for peritonitis.
The Pneumococcal peritonitis is a peritonitis that is triggered by the bacteria that are also responsible for causing a lung infection are responsible. Especially often you can find it at Girls between the ages of 3 and 10. But since it is included in the primary form, it is one overall very rare disease. If there is a suspicion that an infection with these bacteria may be present, it does not necessarily have to be preceded by pneumonia. The pneumococci are often carried via the intestine and vagina of the child and from there via the bloodstream to the peritoneum and infect it.
Cause for the development of peritonitis Newborns and infants, are certain previous illnesses. It is important to mention the Necrotizing enterocolitis, in which there is a local reduced blood flow to the intestinal wall, whereby it is damaged, which in turn favors the colonization with bacteria. The intestinal wall ultimately dies as a result and the peritoneum adjacent to the intestine becomes inflamed. Other causes can be: A Volvulus, in which the intestine twists, which leads to constriction of the supplying vessels, as well as a so-called Meconium environments, an intestinal obstruction caused by the first feces the child produces. Both of these lead to the intestines becoming brittle and bacteria reaching the peritoneum and inflaming it.
At older children Common causes include those already mentioned Appendicitis, as well as the inflammatory bowel disease Crohn's disease, inflamed lymph nodes in the area of the intestine and so-called Intussusception in which a section of the intestine placed in front is everted into the one in front, like a stocking.
Peritonitis is noticeable in children and infants in a similar way to adults. So they show what is called when pressure is exerted on the abdominal wall Defense tensionswhereby the Stomach feels harder. If the disease is very advanced, the stomach can feel as hard as a board. The Children cheer and have severe abdominal painwhat makes them scared are and cry a lot. Can accompany diarrhea and Nausea with vomiting occur.
In infants there is a sign of weakness Poor drinking to observe. In some cases, the disease can begin slowly. The child is just weak and the symptoms slowly increase over time. There is no hard abdominal wall.
The early therapy is vital, as it can lead to fluid losses and an imbalance in the electrolyte and protein content in the child. There is also the Risk of blood poisoning.
pregnancy
If there has been a history of peritonitis, there is a risk that the inflammation will affect fertility, especially if the peritonitis has been untreated for a long time.
Since the peritoneum is also above the fallopian tubes, peritonitis can also lead to a Inflammation of the fallopian tubes come. Inflammation of the fallopian tubes (Adnexitis) can lead to adhesions and sticking of the fallopian tubes, which leads to a infertility being able to lead. Due to the adhesions or adhesions, the transport of the egg cell through the fallopian tubes can be greatly impaired or even completely impossible, so that the fertilized egg cell cannot implant itself in the uterus.
Sometimes the fallopian tubes can be exposed again through an operation.
Summary
The Peritonitis is an inflammation of the peritoneum, which lines the entire abdomen.
The causes can be organ inflammation, organ perforations, peritoneal dialysis or cancer.
Depending on the cause, a distinction is made between local and generalized inflammation.
In both cases exist strong pain of the abdomen, which in the case of local inflammation is limited to the focus of the inflammation. In the case of generalized inflammation, the patient is critically ill and suffers from severe accompanying symptoms.
In both cases, surgery is the only curative therapy and should always be carried out as early as possible, otherwise the inflammation can become fatal.
The local inflammation is treated by removing the appropriate organ and antibiotic therapy.
The generalized inflammation however, it requires extensive intensive medical treatment after the operation and is associated with a mortality of 50%.