Overweight in children
introduction

In recent years there has been a significant increase in overweight among children and adolescents. Obesity is the most common nutritional disorder in children in developed countries.
Studies of primary school students in grades 1-4 showed a rate of 12 percent of severely overweight children.
According to the results of the MONICA project of the World Health Organization (WHO), one in five children and one in three young people in Germany is classified as overweight. Half of these children are pathologically overweight.
A recent investigation by the conventional medical service in the south-west Palatinate
(Rhineland-Palatinate) has shown that 20% the fourth graders are overweight.
The signs are already in 9 percent of them Obesity (Obesity) pronounced. However, these are by no means special conditions in the south-west of the Palatinate, but - as has been shown in studies - representative figures for the whole of Germany.
It is expected that around 80 percent of overweight children will become fat adults. The World Health Organization therefore classified morbid obesity as a chronic disease and experts even speak of the largest epidemic of the 21st century.
Since obesity does not develop overnight, the first signs should be taken seriously and the children should be supported to keep their weight in the normal range. It is primarily about more exercise and a healthier diet.
In particular, children and young people should learn that exercise is fun and that healthy food tastes good.
In no case should an idealization of slimness be conveyed, but rather the aim is to make children and young people aware of their own strengths and to strengthen self-confidence.
The treatment of overweight children is controversial.
The opponents are of the opinion that obesity grows in old age anyway, that the children are unnecessarily burdened, eating disorder can arise, the children are labeled and they are trimmed to the ideals of beauty of our society.
Proponents assume that children are already under psychological and physical stress and with targeted therapy concepts one would like to ensure a long-term reduced body weight and thus a higher quality of life.
When is it overweight?
Obesity is defined as an excessive increase in adipose tissue.
It occurs when the body weight is above the age and gender norms.
Any therapy must be preceded by a medical diagnosis and assessment of body weight
With the help of BMI (body mass index) and the so-called weight percentiles, a distinction is made between normal weight, overweight and underweight. The terms overweight, obesity, obesity and obesity are often used synonymously, despite their different meanings. Obesity and obesity should not be mentioned because of their discriminatory character.
To determine the BMI you need the current weight and height of the child.
The formula for calculating the BMI in adults goes back to the Belgian mathematician Adolph Quetelet and reads:
Weight / kg
BMI = -----------------------------------
Height x height
Example: The child weighs 60 kg and is 1.40 m tall.
BMI = 60: (1.4 x 1.4) = 60: 1.96 = 30.6
In this case, the BMI is rounded up to 31.
There is a percentile table for boys and one for girls. The age of the children is also taken into account.
The current Body mass index (BMI) is entered in combination with the age of the child in the percentile table and read off on the horizontal axis between BMI and age.
Values above the 85th percentile can be described as conspicuous and above the 90th percentile the child is overweight. Values above the 97th percentile mean that there is obesity.
The fat distribution pattern is also included in the diagnosis.
A distinction is made between a female (gynoid) form, which mainly has increased fat tissue on the hips and thighs (so-called pear type) and a more male (androgens, central, (abdominal) form, with a concentration of fat mainly in the abdominal region
(so-called apple type).
In adulthood, the risk of medical sequelae increases with the so-called apple type. There are controversial findings in children and adolescents. However, there is a risk that overweight children will stabilize and continue into adulthood.
Fat deposits in the abdominal region can be most accurately identified with the help of Computed Tomography and Magnetic resonance imaging represent.
Causes and Health Effects of Obesity in Children
causes

Usually the cause is positive Energy balance in front. This means that either too many calories are consumed over a long period of time or too few due to a lack of exercise Calories burned. Excess food energy is stored in fat deposits over the long term.
However, there are other causes of Obesity. These forms make up only 5 percent of childhood obesity cases. Even so, these disorders must be carefully ruled out in overweight children.
A distinction is made between primary (too many calories or too little exercise or both) and secondary obesity. Secondary means that the obesity is due to endocrine (affecting the hormonal system) or genetic (inherited) underlying diseases. Medicines can also trigger obesity.
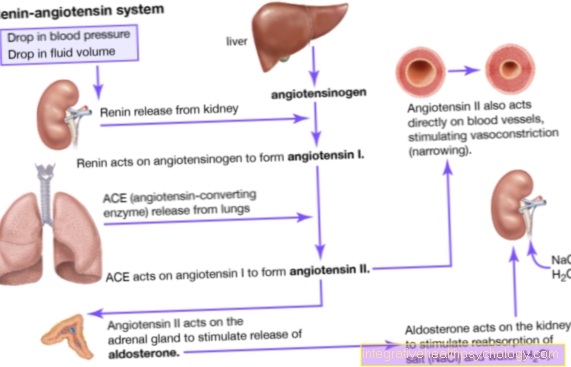
Endocrine causes
Endocrine (affecting the hormonal system) causes include in particular Cushing's syndrome (including full moon face, trunk obesity) with impaired function of the adrenal cortex. There is an increased cortisol production.
This can be innate and acquired. Medication (for example the long-term use of Cortisone preparations) can trigger Cushing's syndrome.
An underactive thyroid (hypothyroidism) or increased insulin production could also be considered as further endocrine causes.
Acquired malfunctions of the pituitary gland (hypothalamus) are also possible, although very rare. This can be triggered by injuries, infections or tumor growth.
Hereditary diseases
There are some very rare hereditary diseases that are associated with being overweight:
- Prader-Willi Syndrome
This hereditary disease (dominantly inherited) is associated with obesity, short stature, decreased muscle tension and an intellectual disability. - Bardet-Biedl syndrome
The children suffer from a mental handicap, retinitis pigmentosa (the nervous parts of the retina go under and go blind). There is usually overweight. - Alström syndrome
The children suffer from diabetes, deafness, retinitis pigmentosa, overweight etc.
Genetic disposition
In twin studies, the genetic predisposition as a cause of obesity has been examined in detail. Identical twins (identical in terms of hereditary disposition) showed surprisingly similar rates of obesity, even though they grew up in different living conditions.
This could prove a certain predisposition to the development of obesity. However, it is not overweight that is inherited, but rather the susceptibility to becoming overweight.
Social factors
In America in 1997, studies found an association between overweight parents and their children.
The likelihood that the children will become overweight in the course of their lives increases if only one parent is overweight. Behaviors, eating habits and preferences for certain foods within a social reference group certainly also play a role. The role model function of the parents is of particular importance.
According to the latest study by the Federal Research Institute for Nutrition and Food (presented by Consumer Minister Seehofer on January 30, 2008), there is a connection between high body weight and social origin (education, income). For example, 35 percent of women from the lower social class are obese. In the upper class, this proportion is only 16 percent.
Advertising and ideals of beauty also influence behavior in different ways. A development of obesity is just as possible as the development of eating disorders.
Biological factors / energy balance
So far it has not been possible to clarify clearly whether children of normal weight differ from overweight children in terms of energy utilization based on their basal metabolic rate. Studies available to date deal with children who are already overweight and therefore do not allow any conclusions to be drawn about the development of obesity.
Stress and emotional health
Eating is often used as a substitute for suppressing negative feelings and moods. Moods such as loneliness, sadness, fear, longing for love, feelings of guilt, boredom, anger, frustration, disappointment and fear of failure can be triggers for ingesting food.
Hunger takes a back seat and the natural hunger and satiety signals are ignored.
Patterns that have been learned, such as: empty plates so that the sun shines tomorrow, eat something first before difficult tasks, and eat as a reward and consolation must be taken into account here.
Eating at certain usual times (without feeling hungry) also plays a role here.
also read Lose weight without hunger.
Physical activity
In fact, our children's physical activity behavior has deteriorated dramatically over the past few decades.
According to a long-term study by the AOK, the physical fitness of children fell by 20 to 26 percent between 2001 and 2003 alone.
As a result, primary school students only move an average of 1 hour per day. The rest of the time they spend at school, with homework and in their free time in front of the television and computer.
In 1976 it took a ten year old child six minutes to run 1000 meters. Today it only manages about 870 meters on average during this time.
Some toddlers spend up to 4 hours a day in front of the TV or PC. The German Nutrition Society (DGE) clearly indicates in its Nutrition Report 2000 that there is a connection between television consumption and obesity.
The reasons for this are quickly clear: Those who exercise little use less energy - the result is gain. Little movement also means that fewer muscles are formed, or even regressed, and thus the basal metabolic rate drops. Since fat children do not like to move at some point because it becomes more and more strenuous, the weight spiral begins to turn upwards.
In addition, the child's physical development is closely linked to his or her mental development. Whenever we move, new circuits and networks form between the nerve tracts that can later be used for other services.
Children who move around and romp around regularly can concentrate better, attention is increased and they are more balanced.
Of course, physical activity can also be associated with a certain predisposition. The natural urge to move is different from child to child. Much more important for the physical activity of our children than this, however, is the role model of the parents and that of the wider social environment. If the parents exemplify the fun and joy of physical activity and instruct the children to do so, an important step towards normal-weight children has already been taken.
Can you lose weight with slimming drops? Read our article on this: Gracia slimming drops - a solution for obesity?
Eating habits and eating habits
Eating behavior, created by the role model function of parents and family, is shaped by habits. Not chewing properly, eating on the side, eating hastily, not enjoying food, eating standing up, eating while watching TV, reading while eating are the most common learned behaviors.
This also includes what is known as "snacking". This describes an eating behavior that is characterized by incessant eating on the side. These portions are usually only very small snacks, but often high in calories and the daily energy intake quickly becomes positive.
Eating habits and the preference for certain foods within a family or social group are adopted.
Energy supply
Obesity is based on either too much energy being supplied to the body or too little energy being used. This creates a positive energy balance, i.e. the energy input is higher than the energy consumption.
The energy consumption is made up of the basal metabolic rate (55 percent of the energy requirement), thermogenesis and the energy requirement for physical activity.
Of the Basal metabolic rate is the amount of energy the body needs to maintain all important body functions. So, in complete peace.
The Thermogenesis makes up about 25 percent of the energy requirement. It is used to describe the process of heat generation through the "burning" of food. Cold and food intake increase thermogenesis.
Depending on the level of activity, physical activity accounts for the remaining 20 percent of the daily energy requirement
Energy requirements in children and adolescents
Average energy requirements of children and adolescents in kilocalories per day / reference values
- 1-4 years
- Boys: 1100 kcal
- Girls: 1000 kcal
- 4-7 years
- Boys: 1500 kcal
- Girls: 1400 kcal
- 7-10 years
- Boys: 1900 kcal
- Girls: 1700 kcal
- 10-13 years
- Boys: 2300 kcal
- Girls: 2000 kcal
- 13-15 years
- Boys: 2700 kcal
- Girls: 2200 kcal
- 15-19 years
- Boys: 3100 kcal
- Girls: 2500 kcal
For example, if a ten-year-old girl eats a bar of chocolate or 100 grams of chips a day, she has already covered a third of her daily energy needs with around 500 kcal.
Critical phases for the development of obesity
Furthermore, it can be distinguished whether the obesity arose early (“child-houd-onset obesity”) or late (“maturity / adult-onset obesity”).
Basically, three critical phases can be identified in the development of child obesity:
- first year of life
- between five and seven years ("adiposity rebound")
- Puberty / adolescence
Medical sequelae and health effects
Obesity in children not only has "aesthetic effects", it is rather a chronic disease for body and soul.
Consequential physical stress
Even in children, being overweight can lead to a number of other diseases. These risk factors are a little less diversified in children than in adults. The WHO classifies these consequential damages according to the probability of their occurrence.
High probability: Faster growth, stability of excess weight, disorders of lipid metabolism, increased blood pressure, cardiovascular problems
Medium probability: Disorders in sugar metabolism, fatty liver Low probability: orthopedic problems, insomnia, gallstones
The cardiovascular system of overweight children suffers from the extra pounds. It's just as if the child had to carry around a backpack with weights every day. In the worst case, permanent heart damage can result.
Around 60 percent of overweight children have poor posture, which often manifests itself in stressful back pain.
Knee, hip and ankle joints are permanently exposed to high loads and osteoarthritis (joint wear) can set in at an early stage.
Diseases that otherwise only affect adults can also be observed in overweight children in exceptional cases. This includes what is known as sleep apnea. Because of the obesity, among other things, breathing stops during sleep, which can end in reflex startles in some cases.
This results in unrefreshing sleep, the children are tired during the day, cannot concentrate, often complain of headaches and are not able to perform well.
Metabolic diseases are also a common consequence of being overweight. More and more affected children suffer from type 2 diabetes.
Read more on the topic: Diabetes in Children
This is a form of diabetes that occurs when the pancreas is tired due to long-term peaks in blood sugar levels.
She is no longer able to produce enough insulin to keep the blood sugar level normal. The result is a form of diabetes that used to occur mainly in the elderly and was therefore also called adult-onset diabetes.
Other metabolic disorders such as lipid metabolism disorders (for example high cholesterol) and gout (high uric acid in the blood) can develop. These two diseases are directly related to excessive intake of animal fats (cholesterol) and the so-called purines from animal protein carriers.
Purines are broken down in the body, get into the blood as uric acid and are excreted via the kidneys. Increased blood lipids and uric acid in the blood is always an indication of a diet that is too fat and high in calories and contains many animal products such as meat, sausage and eggs.
Please also read our article on this Consequences of being overweight
Follow-up psychological stress
More common than the above are complications and comorbidities
the psychosocial stress of those affected.
Back pain is obvious and can be treated.
But much less conspicuous, but at least just as noteworthy, are the damage, invisible at first glance, which the psyche can take from being overweight.
First and foremost, there is the often broken self-esteem, which threatens to constantly decrease due to the more or less open remarks and looks in everyday life.
Overweight children and adolescents have a hard time among their peers and, if you look closely, in society in general. They are often teased and ridiculed for their looks and have difficulty belonging.
This is not just about being fat, but also about other things that are associated with being overweight. These are prejudices like fat people are unsportsmanlike, boring, ugly and generally do not correspond to the ideas of attractiveness.
A fat child is particularly deeply hurt and insecure when the criticism and condescension comes from within the family. If parents and siblings start with statements like: “You are too fat”, “You don't get any dessert, you are too fat anyway”, “Oh dear, just take a look at how you look”, then even children with stable characters will eventually become get the feeling that they are not right the way they are. You will feel uncomfortable and unhappy in your own skin. Sometimes this discomfort is tried to eliminate with food and then the cycle is perfect, from which it is difficult for the children to break without specific help.
Serious mental disorders such as anxiety, depression or eating disorders also arise due to this emotional stress.
Please also read our topic on this: Consequences of being overweight.








.jpg)